J. Mark Trotter, PharmD, BCPS; Michelle Moffa-Trotter, PT, GCS; and Wendy K. Anemaet, PT, DPT, PhD, GCS, CWS, GTC, COS-C
PEARLS
❖ Medication use in the older population exceeds that in the younger population in part because of the increased prevalence of disease, clinical practice guidelines calling for combination drug therapy, direct consumer advertising, inappropriate prescribing practices, and unmonitored self-medication.
❖ Detecting unintended drug effects, sub- and supratherapeutic dosing, and medication adherence issues are all within the purview of quality rehabilitation care provision.
❖ Pharmacokinetics describes how the body handles and disposes of a drug. Age-related changes in drug absorption, distribution, metabolism, and excretion help explain alterations in drug actions and drug effects in the older population.
❖ Pharmacodynamics describes what the drug does to the body, and age-related changes in homeostatic mechanisms and receptors place the older adult at an increased risk for drug sub- and supratherapeutic effects.
❖ Drug-related problems, including underutilization, inappropriate prescribing practices, polypharmacy, drug interactions, adverse drug reactions, and nonadherence, are twice as likely in the geriatric population and cost in excess of $75 billion annually.
❖ Close monitoring of patient signs and symptoms, particularly with newly prescribed medications or dose changes, assists in the early detection of adverse drug reactions.
❖ Medication nonadherence in the older population ranges from 40% to 76%, and common barriers cited by older patients include adverse drug reactions, knowledge deficit, sensory and language issues, cognitive impairment, dosing parameters, physical limitations, multiple pharmacy or prescribing physician source, and medication cost.
❖ Some medications have special rehabilitation considerations and may require adjustments in therapy scheduling and/or therapy provision.
The number of drugs prescribed to older adults continues to increase worldwide.1–7 Although the geriatric population represents less than 15% of the US population, this age group purchases over 30% of all prescription and 40% of all nonprescription medications nationally.8 Indeed, medication prescription is the most frequent therapeutic intervention offered, with 75% of older adults leaving a physician’s office with an order for a medication.9 Community-dwelling older adults use an average of 2 to 6 prescription drugs regularly, with most taking 3 agents daily.10–15 The 2002 Slone Survey found that over 50% of older adults use 5 or more different medications weekly, and 12% use 10 or more different medications weekly.16 Medication use in the institutionalized population is significantly higher than in the community-dwelling population, with an average of 5 to 8 prescribed drugs used on a regular basis.17,18
In addition to prescription drugs, those over 65 years consume an average of 1 to 3 over-the-counter medications,10,14 and the use of nonprescription agents is highest in this population.19 Herbal supplement use is also rising, with nearly 25% of older adults estimated to use such alternative therapies.20–22 Put together, 60% to 88% of the geriatric population takes at least 1 medication on a daily basis,8,15,23 and each older adult fills approximately 15 to 20 prescriptions per year.24 Annual prescription drug sales in the United States exceed 3.2 billion prescriptions with total direct drug costs of over $204.2 billion.25
MOST COMMON DRUG CLASSES PRESCRIBED TO THE OLDER POPULATION
▷ Analgesic agents
▷ Anti-infective agents
▷ Cardiovascular agents
▷ Gastrointestinal agents
▷ Hormones
▷ Psychotherapeutic agents
▷ Respiratory agents
▷ Topical agents
Adapted from Moxey et al.15
There are several reasons for the disproportionate use of medications in the older population. Most importantly, the prevalence of disease increases exponentially with age. For example, prevalence rates for coronary heart disease and cancer exceed 20%, and the rates for hypertension and arthritis each exceed 50% in the older population.26
PREVALENCE OF CHRONIC DISEASE IN THE OLDER POPULATION, 2003 TO 2004
▷ Hypertension 51.9%
▷ Doctor-diagnosed arthritis 50.0%
▷ Chronic joint symptoms 46.0%
▷ Coronary heart disease 21.4%
▷ Cancer 20.7%
▷ Diabetes 16.9%
▷ Ulcer 11.9%
▷ Stroke 9.3%
▷ Asthma 8.9%
▷ Chronic bronchitis 6.0%
▷ Emphysema 5.2%
▷ Liver disease 1.4%
Adapted from National Center for Health Statistics.26
With advances in medical understanding of disease pathophysiology and treatment, clinical practice guidelines increasingly call for combination drug therapy or the use of 2 or more medications to optimally manage the chronic conditions so common in the older population.
CLINICAL PRACTICE GUIDELINES RECOMMENDING THE USE OF COMBINATION DRUG THERAPY FOR THE OLDER POPULATION
▷ Hypertension: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. J Am Med Assoc. 2003;289:2560-2572.
Access at: www.nhlbi.nih.gov
▷ Coronary artery disease: ACC/AHA guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Circulation. 2006;113:2363-2372.
Access at: www.acc.org
▷ Angina: ACC/AHA guideline update for the management of patients with chronic stable angina. J Am Coll Cardiol. 2003;41:159-168.
Access at: www.acc.org
ACC/AHA guideline update for the management of patients with unstable angina and non-ST segment elevation myocardial infarction. J Am Coll Cardiol. 2002;40:1366-1374.
Access at: www.acc.org
▷ Acute coronary syndrome: Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2002;23:809-840.
Access at: www.escardio.org
▷ Myocardial infarction: ACC/AHA guidelines for the management of patients with ST-segment elevation myocardial infarction. Circulation. 2004;110:588-636.
Access at: www.acc.org
Management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2003;24:28-66.
Access at: www.escardio.org
▷ Heart failure: ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult. J Am Coll Cardiol. 2001;38:2101-2113.
Access at: www.acc.org
Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J. 2001;22:1527-1560.
Access at: www.escardio.org
Heart Failure Society of America. 2006 comprehensive heart failure practice guideline. J Card Fail. 2006;12(1):10-38.
Access at: www.hfsa.org
▷ Chronic obstructive pulmonary disease: Standards for the diagnosis and treatment of patients with chronic obstructive pulmonary disease: a summary of the ATS/ERS position paper. Eur Resp J. 2004;23:932-946.
Access at: www.thoracic.org
▷ Renal disease: National Kidney Foundation. Kidney Disease Outcome Quality Initiative Clinical Practice: Guidelines for Chronic Kidney Disease: evaluation, classification and stratification. New York: National Kidney Foundation; 2002.
Access at: www.kidney.org
▷ Diabetes: American Association of Clinical Endocrinologists medical guidelines for the management of diabetes mellitus: the AACE system of intensive diabetes self-Management—2002 update. Endocr Pract. 2002;28(suppl):40-82.
Access at: www.aace.com
▷ Gastroesophageal reflux disease: Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastrolenterol. 2005;100:190-200.
Canadian Consensus Conference on the management of gastroesophageal reflux disease in adults—update 2004. Can J Gastroenterol. 2005;19:15-35.
Access at: www.cag-acg.org
▷ Peptic ulcer disease: Management of helicobacter pylori infection. Am Fam Physician. 2002; 65(7):1327-1339.
Access at: www.aafp.org
Canadian Helicobacter Study Group Consensus Conference: update on the management of Helicobacter pylori—an evidence-based evaluation of six topics relevant to clinical outcomes in patients evaluated for H pylori infection. Can J Gastroenterol. 2004;18(9):547-554.
Access at: www.cag-acg.org
▷ Dementia: American Psychiatric Association. Treating Alzheimer’s disease and other dementias of late life. Am J Psychiatry. 1997;154(5 suppl):1-39.
Access at: www.appi.org
Practice parameter: management of dementia: report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2001;56:1154-1166.
Access at: www.aan.com
▷ Parkinson disease: Practice parameter: treatment of Parkinson’s disease with motor fluctuations and dyskinesia: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;66:983-995.
Access at: www.aan.com
▷ Pain: Advances in neuropathic pain. Arch Neurol. 2003;60:1524-1534.
The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50:S205-S224.
Access at: www.americangeriatrics.org
Practice parameter: treatment of postherpatic neuralgia. Neurology. 2004;63:959-965.
Access at: www.aan.com
Another contributing factor to the rise in medication use with age is the result of consumer advertising by pharmaceutical companies.27,28 Patients with symptoms often expect to receive prescriptions for their problems.29 With direct advertising, patients may be more likely to request a specific medication from their physician, even in instances when no clear indication for that drug class exists. Inappropriate prescribing practices also compound the problem.30 Finally, unmonitored self-medication with over-the-counter, herbal, and “leftover” prescription drugs may contribute to the higher rate of medication use and drug-related complications in the older population.
With the high prevalence of chronic disease, functional impairment, and pain in the rehabilitation population, the typical geriatric rehabilitation patient is often on a complex medication regimen to address his or her multifactorial needs.15
As part of the interdisciplinary team, therapists should gain competency in the drug regimen review and monitoring process. Discerning unintended drug effects, subtherapeutic dosing, and medication adherence issues are all within the purview of quality rehabilitation care provision. Competency begins with an understanding of the age-related changes that impact pharmacologic parameters in the older population.
MEDICATION USE AND EXPENSE ACCORDING TO HEALTH STATUS IN THE COMMUNITY-DWELLING OLDER POPULATION
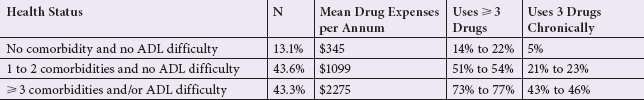
Comorbidity was defined as the presence of hypertension, coronary heart disease, acute myocardial infarction, angina, stroke, diabetes, arthritis, osteoporosis, emphysema/chronic obstructive pulmonary disease, Alzheimer disease, or Parkinson disease.
ADL, activities of daily living.
Adapted from Moxey et al.15
PHARMACOKINETICS IN THE OLDER POPULATION
Pharmacokinetics describes how the body handles and disposes of a drug. Age-related changes in pharmacokinetics may partially explain why the older population responds differently to drugs than the younger population. Absorption, distribution, metabolism, and excretion are 4 aspects of pharmacokinetics impacted by the aging process (Figure 7-1).29–38
Absorption
Absorption is the rate at which a drug leaves the administration site and the extent to which this occurs. Bioavailability is an index measure of the amount of drug that reaches the systemic circulation. Manufacturers use bioavailability data to determine the optimum drug dosage or strength that produces a desired therapeutic effect. For example, manufacturers compensate for low bioavailability with higher dose potency so that enough of the drug is successfully absorbed in the adult population. The largest determinant of bioavailability is the medication’s administration route. Intravenous agents have 100% (eg, ampicillin) bioavailability, whereas oral agents may have as little as 1% (eg, alendronate) or as much as 100% (eg, fluconazole) bioavailability. On the other hand, the bioavailability of topical agents is negligible; because topicals are designed to act locally, the drugs do not reach the systemic circulation to any large extent. Age-related changes that may impact absorption include changes in tissue perfusion, saliva production, and gastrointestinal function.
Reduced tissue perfusion and muscle atrophy may impair absorption of intramuscular injections, and, accordingly, they are less preferred in the older population.33 Impaired tissue perfusion may also affect the absorption of transdermal agents.33 Thus, transdermal agents seen in the rehabilitation population such as nitrate and fentanyl patches are dosed to therapeutic effect (ie, control of angina or pain) rather than standard dosing guidelines, which are geared toward a largely young population. Impaired saliva production may retard absorption of buccal route agents,32 but fortunately these are rarely encountered in the older population.
DRUG ADMINISTRATION ROUTES
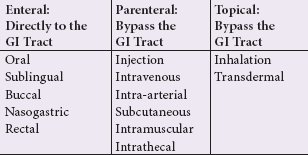
GI, gastrointestinal.
Adapted from Trotter JM, Moffa-Trotter ME, Anemaet WK. Medication Profile in Pharmacology for Rehabilitation Professionals course material. Clearwater, FL: A&T Rehabilitation Solutions; 2005:8.
Because of cost and ease of administration, oral formulations are the most commonly used. Following administration, oral agents largely undergo passive diffusion within the gastrointestinal epithelium. Age-related changes to the gastrointestinal system include increased gastric acid pH and reduced secretion, 30% smaller surface area, weaker peristalsis, delayed gastric emptying, 40% reduction in splanchnic blood flow, and slower intestinal motility.39 Although these changes do not reduce drug absorption per se, they may delay the rate of absorption and the time required to attain the peak drug effect. Some notable exceptions relevant to rehabilitation include l evodopa and propranolol, which may each have upward of 50% higher bioavailability in the older population and require compensatory dose reductions. Also of note, a minority of drugs use active transport for absorption, but the function of this mechanism is equivocal across all age groups.
In the older population, clinically significant changes in drug absorption are not common. However, therapists assist the physician by monitoring symptoms so that any needed dose adjustments may be made accordingly.
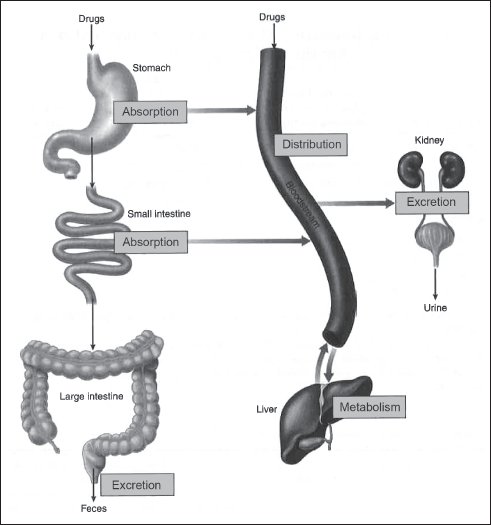
Figure 7-1. The 4 aspects of pharmacokinetics.
FACTORS INFLUENCING ABSORPTION AND IMPLICATIONS FOR THE OLDER POPULATION
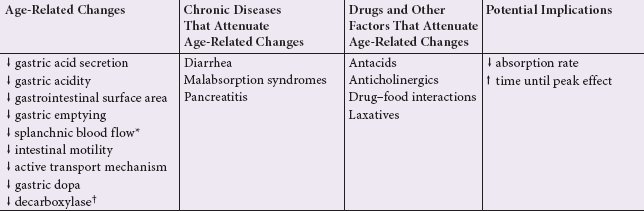
*Propranolol is extensively (near 90%) metabolized on first pass through the liver in the general population. The diminished splanchnic blood flow with age allows greater absorption of the drug into the systemic circulation before reaching the liver, so bioavailability of propanolol is significantly higher in the older population.
†Levodopa is degraded by decarboxylase, and reduced decarboxylase levels with age cause higher levodopa concentrations in the older population.
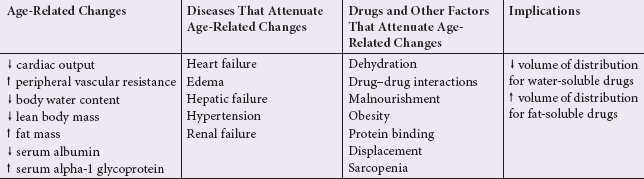
FACTORS INFLUENCING DISTRIBUTION AND IMPLICATIONS FOR THE OLDER POPULATION
Distribution
Distribution is the extent of drug dispersion in the systemic circulation to the site of action. Most of this occurs passively, and the remainder occurs with active protein transport via albumin, alpha-1 glycoprotein, and corticosteroid-binding globulin. Changes in central and peripheral circulation, serum protein levels, and body composition may impact distribution with age.
Passive diffusion relies on the cardiovascular system to carry the drug from the administration site to the target site. The lowered cardiac output and increased peripheral vascular resistance seen in the geriatric population slow the rate of passive drug transport within the body. Drugs that rely on active transport, specifically through binding of albumin or alpha-1 glycoprotein, may also experience a change in distribution with age.
Overall, the protein binding capacity diminishes 15% to 25% with age.40 Albumin levels decline 10% to 12% in the older population,41 and the prevalence of renal disease and malnourishment associated with low albumin is higher in this population. If less circulating albumin is available for drug binding, more of that drug remains in the circulation, causing a higher free fraction drug level. Clinical significance is usually negligible, but it may cause an exaggerated or supratherapeutic effect in older patients with low serum albumin levels. This is most likely in high-risk patients using drugs that have a high affinity for albumin and a narrow therapeutic index like phenytoin and warfarin. Conversely, levels of alpha-1 glycoprotein increase with age. The net effect is a nearly 40% reduction in free fraction drug levels in medications reliant on this transport mechanism,42 such as lidocaine and phenytoin; however, this has not been proven to be clinically significant in the older population.
The largest determinant of passive drug distribution in those over 65 is the change in body composition over time. Medications are largely water or fat soluble. Water-soluble agents like nonsteroidal anti-inflammatory agents, many antibiotics, and acetaminophen have decreased distribution with age because of the 10% to 25% reduction in total body water content43–45 and the 12% to 19% loss of lean body mass.44 As a result, more of the drug remains in circulation, causing a higher free fraction drug level and attenuated drug effects. In this case, lower starting doses are often beneficial. On the other hand, total body fat increases 20% to 40% with age,39,43,46 so fat-soluble drugs like many anti-arrhythmics, diazepam, and lidocaine are more rapidly and extensively absorbed into adipose tissue reservoirs. Here, the drug requires more time and a higher loading dose to attain the desired therapeutic effect. Fat-soluble agents may also have a prolonged duration of action because of the large drug reserve available.
Clinically significant changes caused by altered drug distribution are more likely in high-risk patients such as those with low albumin (eg, renal disease, malnourishment, and heart failure) and/or marked body composition changes (eg, dehydration, sarcopenia, and obesity). These factors should be addressed by the physician when he or she formulates the drug prescription. The therapist assesses patient symptomatology regularly to assist the physician in adjusting drug dosage and dosing intervals as needed to obtain a safe therapeutic effect despite any age-related change in distribution.
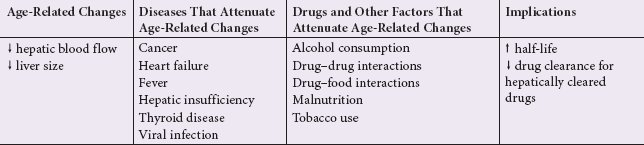
Metabolism
The biologic transformation of a drug into an inactive molecule, a more soluble compound, or a more potent metabolite is called metabolism, and it occurs primarily in the liver. With age, hepatic blood flow decreases 40%,47–51 and liver size declines 25% to 35%.51 Nevertheless, liver function is compositely unaffected by old age in the well older population. In old age, medications dependent on hepatic metabolism, such as the 50% of agents metabolized by cytochrome P450 enzymes, may be prone to drug accumulation and prolonged drug effects because less of the drug is metabolized through the liver. Indeed, these drugs, including warfarin, steroids, and ibuprofen, can have a 50% to 75% reduction in hepatic clearance compared to the younger population.31,33,50,52 Physicians adjust for this by prescribing a lower initial dose and titrating slowly to the desired therapeutic effect. Therapists assist in this process by updating the physician about sub- or supratherapeutic effects that warrant further dose changes.
FACTORS INFLUENCING METABOLISM AND IMPLICATIONS FOR THE OLDER POPULATION
FACTORS INFLUENCING EXCRETION AND IMPLICATIONS FOR THE OLDER POPULATION
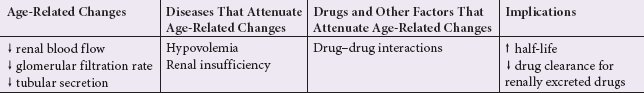
Excretion
Excretion is the elimination of the drug from the body, and it is the pharmacokinetic parameter most affected by age. Drug clearance describes the body’s ability to eliminate a drug and is used to determine the steady-state concentration for a given dose. The kidney is the primary organ responsible for drug elimination. Renal function declines by 35% to 50% with age53 and is marked by a 20% to 25% nephron loss,54 reduced tubular secretion, decreased renal blood flow, a 25% to 50% decline in glomerular filtration rate,37 and fibrosis. Average renal clearance declines 50% to 75% with age,31 so renally cleared drugs experience a prolonged half-life in those over age 65. This means that circulating free fraction drug levels are elevated, and a prolonged drug effect may occur, particularly in patients with marked renal impairment. Drugs dependent on renal clearance, such as gabapentin, multiple antibiotics, and antivirals, must be dose adjusted by the physician to avoid these adverse consequences.
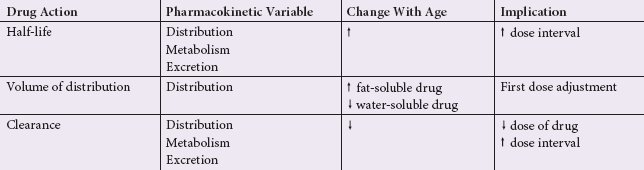
Pharmacokinetics assists in explaining drug actions and determining drug effects. For example, the processes of distribution, metabolism, and elimination all help determine the half-life (ie, the time it takes for one-half of the original drug dose to be removed from the body). Half-life may be reduced by 50% with age and is an important pharmacokinetic variable because it reflects the drug’s duration of action. Half-life is used to determine therapeutic dosing intervals so that a steady-state concentration of the drug remains within a therapeutic range. This is important for chronic diseases such as seizures, hypertension, and diabetes in which symptom fluctuations may precipitate adverse events.
The volume of distribution is the relative portion of a drug in the body as a function of body mass. At-risk older adults (eg, those with hypoalbuminuria, obesity, or heart failure) may require a 10% to 20% loading dose adjustment to compensate for alterations in distribution. In practical terms, this is done when physicians follow the “start low, go slow” principle of drug loading and titration for the older population.
Drug clearance is a function of the volume of distribution, metabolism, and excretion. Physicians use drug clearance to determine the drug dosage required at each dosing interval to achieve a consistent therapeutic effect.
Pharmacokinetics also helps determine important time-based drug effects such as onset of action, peak effect, and duration of action.
These pharmacokinetic variables may directly impact rehabilitation interventions. For example, a common area of disability among the rehabilitation population is pain. Physicians often prescribe analgesic agents to address this problem. To optimize pain management during rehabilitation, the therapist should consider specific analgesic drug effects to enhance patient tolerance of therapy and, ultimately, rehabilitation goal attainment. With a prescription for ibuprofen, the pharmacokinetics of this drug is such that the onset of action is 1 hour, the peak effect occurs within 1 to 2 hours, and the duration of action is 4 to 8 hours. Therefore, for ibuprofen, the ideal pretreatment window for the analgesic effect is 60 to 90 minutes before rehabilitation. Such drug-specific pharmacokinetic information could also be used in patients with gastrointestinal symptoms, respiratory impairments, and some neurologic disorders to optimize treatment scheduling and improve tolerance to the rehabilitation program.
IMPLICATIONS OF AGE-RELATED CHANGES FOR PHARMACOKINETIC VARIABLES
IMPLICATIONS OF AGE ON TIME-BASED DRUG EFFECTS
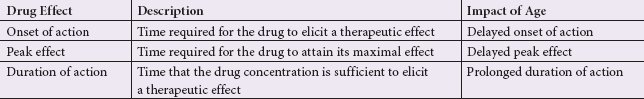
Adapted from Trotter JM, Moffa-Trotter ME, Anemaet WK. Medication Profile in Pharmacology for Rehabilitation Professionals course material. Clearwater, FL: A&T Rehabilitation Solutions; 2005:8.
PHARMACODYNAMICS IN THE OLDER POPULATION
Pharmacodynamics describes the response of the body to the effects of a drug at a given concentration. It explains what the drug does to the body. All medications elicit an intended or unintended response through their mechanisms of action. The ideal response is a therapeutic effect, but age-related changes in pharmacodynamics place the older adult at risk for sub- or supratherapeutic effects. Older adults exhibit altered drug pharmacodynamics, which is attributed to changes in homeostatic mechanisms and receptor alterations.29,31–34,36–38
IMPAIRED HOMEOSTATIC MECHANISMS WITH AGE
| Homeostatic Mechanism | Age-Related Changes |
| Thermoregulation | ↓ basal temperature Blunted febrile response |
| Blood pressure maintenance | Hypertension Prone to orthostasis |
| Volemic maintenance | Prone to dehydration |
| Respiratory function | Blunted sensitivity to ↑ carbon dioxide levels |
| Clotting cascade | Clotting response |
| Insulin regulation | Insulin resistance |
| Bone homeostasis | Bone absorption > bone formation |
| Skeletal muscle maintenance | Muscle protein catabolism > muscle protein synthesis |
| Bladder function | Incontinence |
| Bowel function | Constipation |
| Gait and postural stability | Prone to falls |
| Cognitive reserve | ↓ cognitive function, memory |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








