Overview
Humans are Occupational Beings
The science underlying the occupational therapy (OT) profession views humans as occupational beings.1, 2 Globally, humans are typically identified by their occupations. In other words, who we are is often determined by what we do. What we do are the activities (occupations) that comprise our lives. Thus, the focus of OT interventions with and on behalf of older adults is to address their unique needs and preferences for what they need and want to do in addition to what they are expected to do, typically concurrently with age-related changes and acute and/or chronic conditions. These potential or actual changes in the ability to perform necessary and desired activities (occupations) impact how elders conduct their everyday lives and present a threat to their overall health and identity.2–4 Typically, the identity and sense of wellbeing of the elders is expressed through their participation in the activities/occupations that comprise the roles, habits and routines that encompass their lives. These patterns of participation represent who they have been throughout their lives, who they are today and who they may yet become. Participation in society to the extent needed and desired by elders is fundamental to their perception of the quality of personal life and also a basic component of the World Health Organization (WHO) current disability model, the International Classification of Functioning, Disability and Health (ICF).5
Conceptual Foundations of Geriatric Occupational Therapy
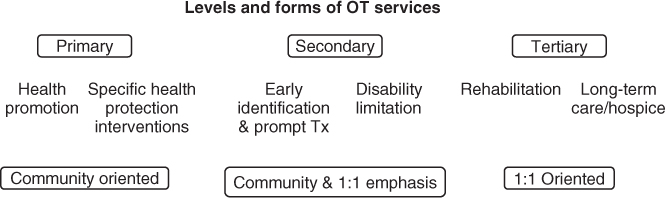
With a simultaneous focus upon intrinsic and extrinsic factors that impact elders’ participation in expected, desired and meaningful activities, OT personnel work in partnership with the individual or organizational client to promote the enablement of ageing adults to pursue a meaningful quality of life (QOL) at all levels of care. The WHO conceptual model and OT services interface intimately, as noted in Figure 141.1.
Figure 141.1 WHO ICF model. Adapted from International Classification of Functioning, Disability and Health (ICF), World Health Organization, Geneva, 2001, Figure 1.
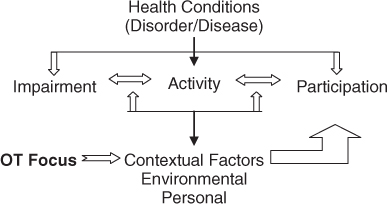
OT interventions centre on enabling elders to pursue the activities, tasks, habits and routines that are personally important and meaningful to them. All of these activities and occupational components contribute to the elders’ perception of their QOL. The WHO ICF is the currently accepted model for systematically grouping consequences associated with health conditions. Level of ability, function and/or disablement are seen as a dynamic interaction between the individual’s health condition and their personal environmental contextual factors. These intrinsic and extrinsic factors affect the individual’s ability to pursue the needed and desired activities that comprise their lives and to participate in individual and group societal functions. If impairment and contextual factors are incompatible, this set of circumstances in turn affects the individual’s overall sense of wellbeing and personal perceptions of their QOL.5
Person–Environment–Occupation–Performance/Participation Model
Figure 141.2 presents the OT Person–Environment– Occupation–Performance/Participation (PEOP) model that is complementary to the WHO ICF model.6 The PEOP model depicts wellbeing and QOL as a function of the relationship of the personal/intrinsic factors, the environmental/extrinsic factors, occupation/activity and occupational performance/participation in activity and society.6 These components are shown as being totally interdependent. Figure 141.2 and the following model express the P–E–O–P relationship:
where ‘elder quality of life’ is dependent upon and a function of the person’s unique health status and functional abilities, plus the degree to which their environment supports the occupations/activities that they need and want to pursue and allows them to perform/participate in society, to meet their requisite needs and desires.
Figure 141.2 Person–Environment–Occupation–Performance/Participation (PEOP) model applied to geriatric OT practice. Adapted from Christiansen et al.6
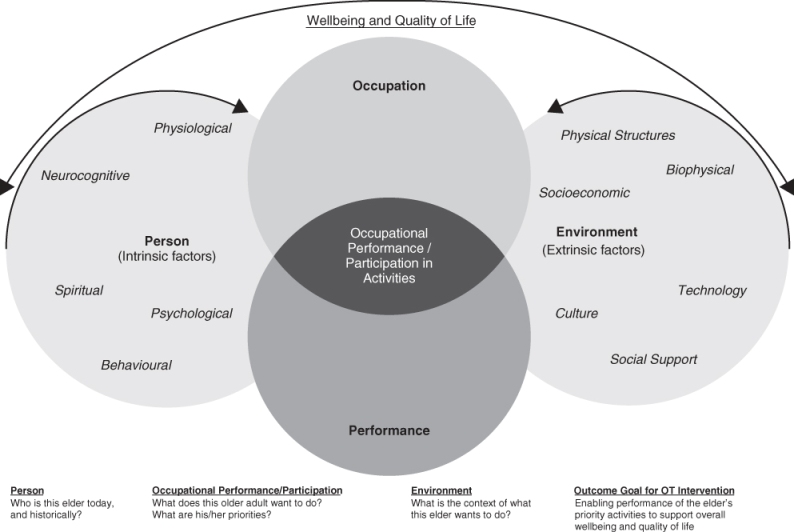
Person (Intrinsic Factors)
Occupational therapists assess and intervene to enable elders to cope with normal and inherent age-related changes known as intrinsic factors. These factors include physiological, motor, cognitive, spiritual, neurobehavioural and psychological components of human function. The older adult’s level of motivation, and also roles, habits and routines that comprise their lifestyle, are an integral part of occupational performance and QOL. Hence the capacity for life-long homemakers to continue cooking and taking pride in their culinary creations may be compromised by diminishing olfactory and gustatory ability. In addition, the elders’ individual beliefs about themselves and their life experiences—past, current and potential—impact their execution of self-maintenance, work, service, leisure and other activities.
Environment (Extrinsic Factors)
Extrinsic or environmental/contextual determinants of occupational performance include social support, social and economic systems, culture and values, technology, the built environment and also the natural environment.6, 7 Typically, intrinsic age-related changes in vision, hearing, olfaction, vestibular functions, musculoskeletal and other systems may alter the individual’s ability to cope with any or all of these extrinsic environmental factors. The elder’s physical surroundings may not adequately support their performance of necessary and desired activities because of age-related changes that they experience. Therefore, in order for elders to continue to live independently (if culturally appropriate) and participate as fully as possible, the inherent changes in sensory and other systems, and also in cognition, may require changes in their physical environment and other external support systems.
Occupation (Activity)
What humans do consists of occupation(s). Occupations, better known as activities, include all abstract and observable types, and comprise the everyday lives of people of all ages around the world.8 They also assist individuals in understanding who they are, as humans often define themselves by what they do. When younger adults are asked, ‘What do you do?’, they may respond by stating their role as student, the type of worker/vocation they pursue or their role as homemaker or parent. When elders are asked the same question, they may respond differently, depending upon what is important to their sense of identity at this later point in life. Nevertheless, occupation/activity in all conceivable forms is the fabric of human existence.
Participation
Active involvement in daily life and various life situations comprises participation. This concept includes the ability to perform roles at home, work and in the community. Various factors may hinder an individual’s ability to function in one or more of these environments, due to lack of support, attitudes, and physical, social and/or societal barriers.7, 9, 10 Throughout their lifespan, individuals encounter different forms of access or barriers to participate in activities that are necessary and meaningful to them.5, 11–14 In the latter years of life, elders may encounter limits to their participation due to decline in age-related or functional abilities, ageism or policies that limit continuation of involvement in activities such as employment or driving.
Scope of Occupational Therapy Services
OT services are provided at three different levels: (1) directly with individuals and/or family/caregiver(s), (2) consultation and administration with community organizations and (3) consultation and/or administration with governmental and/or international agencies. Historically, the majority of services have been provided for individual patients and clients; however, a growing number of community-level OT services have been established during the past several decades. Overall, geriatric OT services are designed to sustain or improve the everyday activity-related wellbeing and QOL of older adults. In addition, services aim to enable families, non-governmental organizations and government agencies to mobilize efforts that promote the health of elders, prevent deterioration of function associated with age-related changes, restore functions that are impaired by organic disease, impairment or disability, and/or provide compensatory techniques necessitated by age or disability-related changes. In providing services, OT personnel collaborate with older adults, medical providers and organizations, in order to sustain or improve the ability of elders to perform necessary and meaningful activities, taking into consideration their overall health status, personality, lifestyle, family and/or other support systems. Thus, whether administered with an individual, group or population, OT interventions aim to ensure a QOL commensurate with the elders’ priorities, and also those of their family members, carers and their communities.
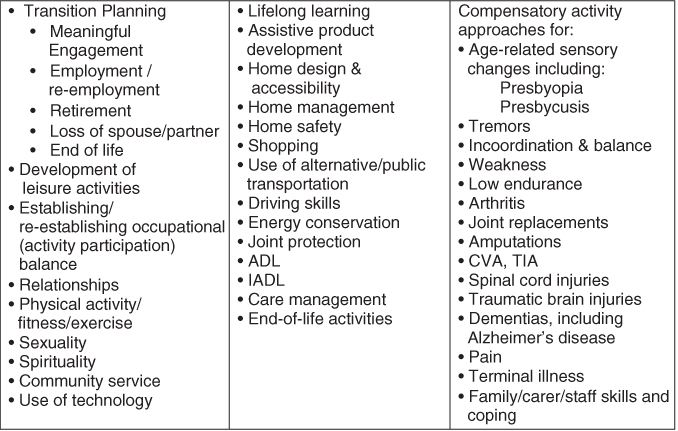
OT assessment and intervention services are provided collaboratively with or on behalf of older adults who are at risk for or experience limitations due to disease, acute or chronic illness, injury, developmental disability, ageing with an existing disability (e.g. cerebral palsy, spinal cord injury, post-polio) and/or the ongoing ageing process. For example, a person who has sustained a stroke may receive OT services in order to relearn how to dress or to feed themselves. Furthermore, an older adult with dementia may benefit from interventions that simplify tasks and routines, maintain safety within the environment and also support the daily routines and wellbeing of the carer. These services are provided throughout the continuum of care, to address the full range of daily activity (occupation) and participation needs of older clients or patients, as shown in Figure 141.3. The levels and forms of OT services range from the needs of older adults living in the community to the needs of those experiencing end-of-life circumstances.
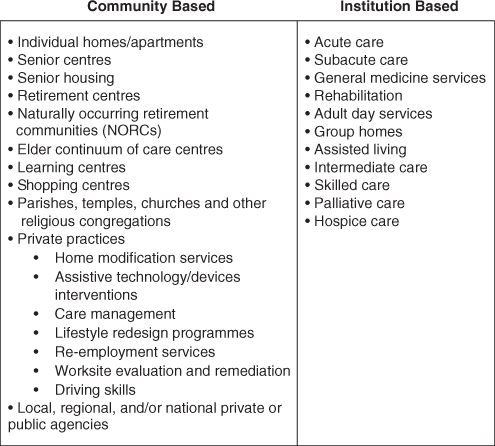
Hence primary, secondary and/or tertiary settings are included in this continuum of OT services. Primary care OT interventions include provision of health promotion and health protection services within communities, and also for individuals. Examples of these types of services include programmes on home safety to prevent falls and other injuries and driver screening, assessment and retraining, as elders experience age-related changes in function. Secondary care OT interventions include individual, group and/or community approaches for management of health conditions such as arthritis and Alzheimer’s disease. Figure 141.4 displays the categories of services that OTs provide to older adults, their family members, and/or carers.
This topical list depicts typical OT services and is not completely exhaustive. Professional OT services are provided in a range of settings throughout the continuum of care, as shown in Figure 141.5. OT services are coordinated with the providers of healthcare and other services, including physicians, nurses, physical therapists, speech therapists, social workers, community and public health agencies and others, whenever indicated and available. When services are provided on an individual basis, family members and/or other available support systems often become an integral component of the OT service team, to ensure successful intervention outcomes. Furthermore, in addition to working with the older adult, OT personnel provide services to their carers, in order to maximize efficiency, diminish stress and support the health and wellbeing of the carers.
Occupational Therapy Process
Assessment and Intervention
Wherever possible, an evidence-based process is applied to the determination of what should be included in the OT assessment and intervention with elders, as shown in Figure 141.6. In the standard practice in which OT personnel work with an individual older adult, a three-phase process of assessment is followed and considered to be ‘best practice’.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree