Introduction
Falls and imbalance are important causes of disability, morbidity and mortality in an ageing population. More than one third of adults aged 65 years and older fall each year. Among nursing homes residents, as many as three out of four residents fall each year; 10–20% cause serious injuries. Falls are the leading cause of accidental deaths and account for most of non-fatal injuries and hospital admissions for trauma. The direct cost of fall injuries in 2000 ranged from US$0.2–19 billion.1 Similar to many other conditions in the geriatric population, factors that can contribute to falls are multiple, and very often more than one of these factors plays an important role. For this reason risk factor assessment, prevention and therapeutic interventions will be the primary focus of this chapter.
Balance
Balance or equilibrium is an ability to maintain the centre of gravity (also known as the centre of mass-COM) of a body within the base of support with minimal postural sway. It is a complex process that depends on the integration of vision, vestibular and proprioception, central coordination and neuromuscular responses that control muscle actions. The senses must detect changes of body position with respect to the base, regardless of whether the body moves or the base moves. When standing, any changes in orientation are perceived by proprioceptive and cutaneous sensors in the feet. Vision detects linear and angular motion of the visual field and the vestibular apparatus detects sway-related linear and angular acceleration of the head. When the support surface is irregular or in motion, vestibular input becomes essential. When the surface is fixed and level, proprioception is predominant. An age-related decline in function can be demonstrated in all parts of this system.
Maintenance of this upright position is associated with postural sway mainly in the anterior/posterior (A/P) direction. Both A/P sway velocity and the area are seen to increase in normal older subjects. Increase in A/P sway has been correlated with spontaneous falls, but a better predictor is mediolateral (side to side) sway. Falls depend on the relationship between the COM and the base of support. In older people, postural reactions controlling the COM are slowed and there appears to be particular difficulty in controlling lateral instability. Moreover, unexpected perturbations require an adjustment of the base of support through compensatory stepping, and older fallers often have problems controlling these compensatory stepping movements. Experiments with a movable platform that can produce multidirectional perturbations show that younger controls react with a rapid compensatory abducting their arms uphill, and hinging at the hips and trunk, thus keeping their COM away from the direction of tilt. In older subjects, compensatory trunk movements are reduced (probably due to stiffening) and their arms are stretched in the direction of the fall.2
Peripheral sensation (proprioception and touch) is the most important afferent control mechanism of standing balance in healthy older people. Other factors that are highly correlated with increased sway are reduced muscle strength in the legs, poor near visual acuity, and slowed reaction time. Vision can partially compensate for loss of other sensory inputs, and with increasing age as the postural task gets harder so the reliance on vision becomes greater. Thus, patients with proprioceptive or vestibular impairments are easily upset if the visual field is faulty or misleading in any way. There is no doubt that some individuals maintain good postural control, even into extreme old age, indicating that age-related changes alone have only a minor effect and that imbalance is largely the result of pathology.
Disequilibrium syndromes are identified by inspection of arising, standing, turning and response to perturbation. There are four main syndromes: dysmetria, or lack of coordination of movement associated with cerebellar disorders; bradykinesia, or delayed postural responses associated with akinetic-rigid disorders (parkinsonism); sensory deprivation due to vestibular dysfunction, or loss of proprioception due to peripheral neuropathy; and apraxia, a central disorganization of learned motor programmes for standing and walking, mainly due to frontal lobe dysfunction.3
Disease-related balance disorders are also common, such as cerebrovascular, cognitive impairment and Parkinson’s disease (PD). Of major importance is the slowing of central coordination due to cerebrovascular or Alzheimer’s disease (AD). In its early stages, this is often unrecognized, and the diagnosis is not made until the patient is seen in a falls clinic. In cerebral multi-infarct states patients with few or any neurological signs may present with disequilibrium (during standing and with perturbations) and gait abnormalities (decreased hip and knee flexion during swing phase and instability during stance phase).4 Minor and even major cognitive impairment is often not considered in the differential diagnosis among recurrent fallers. Balance depends on cognitive processes and attention, which may be affected by anxiety and depression as well as brain pathology. The ability to recover balance demands more attention even for healthy older people when compared with young adults. Older people appear less able to shift weight and select appropriate responses quickly when the environment changes suddenly. The ability to perform multiple or dual tasks is challenged with ageing and becomes diminished in cognitive impairment. One study on institutionalized patients with dementia showed a tendency to stop walking while talking. The difficulties increase as the tasks become more complex, and both the young and the old tend to prioritize gait performance over the secondary cognitive task.5
Gait
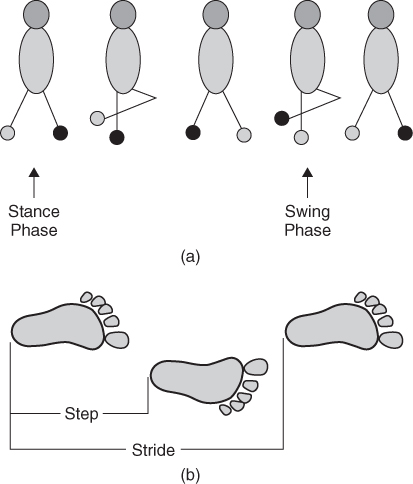
Gait is defined as the pattern of movement of the limbs during locomotion over a solid surface, ‘manner of walking’ or ‘sequence of foot movements’. Figure 91.1 illustrates the components of gait cycle.
Figure 91.1 The walking gait cycle. (a) During double stance, the weight is transferred from one foot to the other; this is known as the stance phase. During single stance, the centre of mass of the body passes over the foot in preparation for shifting to the other limb, resulting in the swing phase. (b) Step versus Stride. Step is described as the period from initial contact of one limb to the initial contact of the contralateral limb. Stride or gait cycle is described as the period from the initial contact of a particular limb to the point of initial contact of the same limb and is equivalent to one gait cycle. Therefore, there are two steps in each stride.
Human locomotion depends on higher command and control centres in the brainstem and forebrain. Its physiological function depends on the origin of stimuli, either internal or external cues. In normal walking–an internally cued, well-learned motor act–the supplementary motor area (SMA) of the frontal cortex engages in significant firing just prior to gait ignition. This preparatory activity represents submovement programme selection, which is subsequently sent to the primary motor cortex area (M1). This SMA activity is switched off by phasic activity generated by the basal ganglia (BG), which provides a non-specific cue both to trigger the submovement and to instruct the SMA to prepare for the next. It is this interaction between phasic activity from the BG and SMA, which is responsible for smooth running of predictable, well-learned, automatic movement sequences that depend on internal cues. The sequence of activation, however, is different when movement occurs in response to external cues. In this situation the BG/SMA pathways could be bypassed with sensory information from the environment feeding directly into the pre-motor area (PMA) through visual, auditory and propioceptive pathways, with the PMA subsequently activating the M1.4 The pedunculopontine nucleus (PPN), an area near to the nucleus cuneiformis below the cerebellar peduncle receives afferent connections from the BG, cerebellum and motor cortex and projects to the brainstem reticular nuclei. Then instructions for gait are passed along non-pyramidal pathways in the ventral spinal cord.6
Parkinson’s disease affects gait by disordered cueing from the BG due to a disturbance in internal rhythm formation in the BG such that the SMA is not switched off on time. This leads to some of the clinical features of PD including bradykinesia, gait ignition failure and freezing. For this reason PD patients seem to rely heavily on intact sensory/PMA pathways to initiate movements (i.e. better walking while stepping over coloured patterns on the ground and drawing movements when they are aided by external cues). An analogous situation may exist among vascular higher-level gait disorders from infarcts to the aforementioned pathways.4
Changes in gait patterns associated with advanced age have been identified, such as slow walking speed due to shorter step length and increased time spent in double limb support. Gait speed declines 12–16% per decade for self-selected gait speed and up to 20% decline for maximum gait speed.7 These age-related changes in walking patterns have been interpreted as indicating adoption of a more conservative or less destabilizing gait, suggesting that older people compensate for their reduced physical capabilities by being more cautious. Menz and colleagues compared a small sample of young and old subjects and found that old subjects exhibited changes in walking, sensory function and muscle strength. Authors concluded that the normal age-related decline in leg strength may be the primary limiting factor that prevents older people walking at an equivalent speed to younger people.8
Gait abnormalities are common in the elderly. An abnormal gait, defined by shuffling or degree of difficulty with turns, was observed in 31% of patients older than 67 years.6 The factors that affect gait in the elderly may include physiological, medical and social aspects. Individually or in combination, these risk factors predispose elders to gait and balance abnormalities.
Physiological factors include neural control, muscle function and posture control, which are impaired by ageing and/or degenerative disease. Neuromuscular ageing changes are contributors of gait alterations, specifically, the loss of cross-sectional muscle mass (10–40%), decrease in type I and type II muscle fibres, prolonged contraction and relaxation time, and a decrease in conduction velocity in sensory and motor nerves with resultant loss of proprioception. Further, within the articular cartilage, there is formation of cross-links and loss of elastic fibres, resulting in stiffer joint capsules and ligaments that affect the quality of movement and gait. The resultant movement pattern will be slower, more uncertain and uncoordinated, and lacking full range of motion.7
Medical factors include the use of psychotropic medications, previous falls, cognitive and neurodegenerative diseases, cardiopulmonary, musculoskeletal, psychological (i.e. depression, anxiety), visual, vestibular and proprioceptive impairments. Along with these factors related to gait impairments the following social factors need to be considered as potential contributors to reduced mobility. They consist of self-efficacy or dependence in activities of daily living (ADL), motivation, lack of social support, use of assistive devices and low level of physical activity.7
Gait disorders are particularly important in older people because they threaten independence and contribute to falls and injury. A classification of gait disorders based on neural system affected has been proposed.3, 6 The lowest-level gait disorders include peripheral sensory dysfunction with peripheral neuropathy, vestibular, visual and propioceptive deficits; and peripheral motor dysfunction with arthritis and neuromuscular diseases (focal myopathic, neuropathic weakness). Middle-level gait disorders consist of hemiplegia/paraplegia (arm and leg weakness, spasticity, equinovarus), cerebellar ataxia (poor trunk control, lack of coordination) and extrapyramidal syndromes (rigidity, bradykinesia, trunk flexion). The highest-level gait disorders are: cautious gait, mild AD, cerebrovascular disease and normal pressure hydrocephalus (cognitive impairment, gait apraxia, and urinary incontinence). Nevertheless, a clinical approach seems more useful for physicians to address gait abnormalities. Sudarsky and Nutt present a clinical syndrome classification of seven gait abnormalities: cautious gait, gait limited by weakness, stiff gait, ataxic gait, veering, freezing and toppling gait, and bizarre gaits3, 6 (see Table 91.1).
Table 91.1 Gait syndromes features and disease examples. Clinical syndrome classification of seven gait abnormalities with its features and disease examples.
| Gait syndrome | Features | Disease example |
| Dysmetria | Imbalance with slow and halting gait with wide base of support and irregular progression | Cerebellar ataxia (Friedreich’s ataxia), chorea, sensory ataxia |
| Stiff/rigid | Loss of fluidity, stiffness of legs and trunk with circumduction, scissoring and equinovarus gait. | Spasticity (cerebral palsy, spinal cord disorders), parkinsonism, dystonia, musculoskeletal |
| Weakness | Waddling, lateral path deviation with regular stride and foot drop | Myopathy, peripheral neuropathy (vincristine, cisplatin chemotherapy, paraproteinemia) |
| Veering | Deviation of gait or falls on one side | Vestibular disorders, thalamic astasia |
| Freezing | Start and turn hesitation, stepping movements with side to side shuffling | Multi-infarct, parkinsonism (PD, supranuclear palsy, Lewy body disease, multiple system atrophy) |
| Cautious | Slowing, short steps, en bloc turns, wider base, shorter swing base | Non-specific, multifactorial |
| Bizarre/psychogenic | Embellished, inconsistent, distractible | Anxiety, conversion disorder, fear of falling or space phobia |
Falls
A fall, defined by consensus statement as the ‘unexpected event in which the patient comes to rest on the ground, floor or lower level’,9 is one of the most common events that threaten the independence of older persons. As with other geriatric syndromes, falls result from the accumulated effect of impairments in multiple domains. The causes of falling often involve a complex interaction among factors intrinsic (medical and neuropsychiatric conditions; impaired vision and hearing; and ageing changes in neuromuscular, gait and balance reflexes) and extrinsic (medications, improper use of assistive device and environmental hazards) to the individual. Rarely is a fall related to a single factor.
Age-related changes in postural control and gait probably play a major role in many falls among older persons. Increasing age is associated with diminished proprioceptive input: slower righting reflexes, diminished strength of muscles, and increase postural sway. All these changes can contribute to falling, especially the ability to avoid a fall after encountering an unexpected trip or hazard. Although ageing changes in gait may not be sufficiently prominent to be labelled truly pathological, they can increase susceptibility to falls. Elderly men tend to develop wide-based, short-stepped gaits; elderly women often walk with a narrow-based, waddling gait.10
Although not all elderly individuals with orthostatic hypotension (OH) are symptomatic, this could play a role in causing instability and precipitating falls. People with orthostatic and/or postprandial hypotension are at particular risk for near syncope and falls, especially when treated with diuretics and antihypertensive drugs. Ooi and colleagues measured supine and standing blood pressure four times in a single day in 844 nursing home residents, both before and after meals. The outcome measure was any subsequent fall over 1.2 years. Fifty percent had OH on at least one measurement. OH did not predict falls in those who had never fallen, but was predictive of recurrence in previous fallers (relative risk 2.6). The timing of OH before or after meals did not affect fall risk. They conclude that OH is an independent risk factor for recurrent falls in institutionalized elderly.11
Other pathological conditions, such as degenerative joint disease, can cause pain, unstable joints, muscle weakness and neurological disturbances. Healed fractures of the hip can cause an abnormal and less steady gait. Diminished sensory input, such as in diabetes and other peripheral neuropathies, impaired hearing and visual acuity diminish cues from the environment that normally contribute to stability and thus predispose to falls. Some studies have shown certain gait abnormalities characteristics of patients with dementia and mild cognitive impairment that may lead to falls. Foot deformities (bunions, calluses, nail disease, joint deformities, etc.) can also cause instability and falls.10
Across studies, many risk factors were found to be consistently associated with falls. These included age, cognitive impairment, female gender, past history of falls, lower extremity weakness, gait problems, foot disorders, balance problems, hypovitaminosis D, psychotropic drug use and use of four or more prescription medications, arthritis, and PD. The risk of falling consistently increases as the number of these risk factors increases. Among these, previous history of a fall is the strongest risk factor for future falls, with sensitivity of 50%, specificity of 80% and 55% absolute risk of falling during follow-up (RR of 2.4; 95% CI 2.1–2.8) across studies.12 A history of stroke demonstrated an absolute risk of falling during follow-up of 34% and dementia demonstrated an absolute risk of falling of 47% across studies.
Risk factors might be easily remembered with the mnemonic ‘AGAIN I’VE FALLEN’ (see Table 91.2).13 In this way a risk-based assessment can help the clinician approaching geriatric fallers as well as non-fallers.
Table 91.2 Fall risk factors. ‘AGAIN I’VE FALLEN’ is a mnemonic for risk-based assessment to approach geriatric fallers.
| Fall risk factors |
| Again fallen (previous history of fall) |
| Gait and balance problems (arthritis, cerebellar disease) |
| Activities of Daily Living loss |
| Impaired mental status (cognitive impairment, dementia) |
| Number and type of drugs (more than four drugs and use of psychotropic, analgesic, diuretic and anti-hypertensive drugs) |
| Illness (new illness, delirium) |
| Vestibular disorders |
| Eyes (glaucoma, retinopathy, cataract), Ears |
| Foot disorders (bunions, calluses, nail disease, joint deformities) |
| Alcohol |
| Lower extremity weakness (stroke, myopathy, deconditioning) |
| Low blood pressure (orthostatic or postural hypotension) |
| Environmental hazards (loose rugs, clutter, poor lighting, wet floor, unstable furniture, patient restraints) |
| Neurological disorders (peripheral neuropathy, stroke, Parkinson’s disease, slowed reflexes |
Adapted from The Saint Louis University Geriatric Evaluation Mnemonics and Screening Tools (Flaherty and Tumosa13).
Clinical Presentation of Falls
More than half of all falls are related to medical conditions, emphasizing the importance of a careful medical assessment. There are multiple and often interacting causes of falls that include accidents, syncope, drop attacks, dizziness or vertigo, orthostatic hypotension, drug-related and specific disease process.
Accidental
Accidental or unintentional falls occur in less than half of all falls.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







