FOLLICULAR THYROID CARCINOMA
Part of “CHAPTER 40 – THYROID CANCER“
PREVALENCE
Follicular thyroid carcinoma accounts for ˜5% to 10% of all thyroid cancers in the United States.11 It occurs at a slightly older age than papillary carcinoma but in recent years has been diagnosed earlier; in some studies, almost half of patients are younger than 40 years of age at the time of diagnosis.180 This tumor is rare in children, occurs infrequently after head and neck irradiation, and is not commonly found at autopsy as an occult tumor.
PATHOLOGY
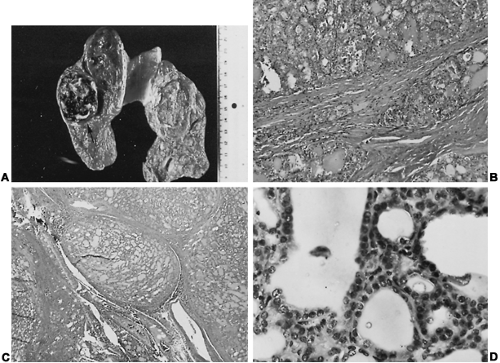
Follicular carcinoma, which is usually encapsulated even when it is aggressive, may initially appear benign on FNA, gross tumor inspection, and frozen-section study; this must be differentiated from follicular variant papillary carcinoma and follicular adenoma.11 Aggressive tumors show extensive vascular invasion or gross capsular penetration and satellite tumor foci around the periphery of the neoplasm (Fig. 40-8A). Most are single lesions that usually do not show necrotic degeneration. Large aggressive tumors extend into the opposite lobe or may lie in adjacent cervical tissue; they should not be mistaken for lymph node metastases, which ordinarily occur only in the more advanced cases with distant metastases.
Microscopically, these are usually compact, highly cellular tumors composed of microfollicles, trabeculae, and solid masses of cells (see Fig. 40-8B, Fig. 40-8C and Fig. 40-8D). Less often, follicular carcinoma has medium-sized or large follicles and such low invasive characteristics that it is difficult to differentiate from a benign adenoma. Such carcinomas have an excellent prognosis.11 Follicular carcinoma has compact, dark-staining, round nuclei that are more uniform in shape, size, and location than
the nuclei of papillary carcinoma and are difficult or impossible to identify as carcinoma by FNA.11,46
the nuclei of papillary carcinoma and are difficult or impossible to identify as carcinoma by FNA.11,46
Hürthle Cell Carcinoma.
Oxyphilic cells, termed Hürthle or Askanazy cells, which contain increased amounts of acidophilic cytoplasm with numerous mitochondria on electron microscopy, may constitute most or all of a follicular carcinoma. Some consider Hürthle cell neoplasms to be a distinct clinicopathologic entity; others consider them to be variants of follicular thyroid cancer.26 Regardless of their classification, Hürthle cell carcinomas have a less favorable prognosis than nonoxyphilic follicular carcinomas, although they initially may not appear less differentiated or more invasive.11
Classification.
Follicular carcinoma can be classified as minimally or highly invasive. Minimally invasive tumors show just enough evidence—slight penetration of the tumor capsule—to make a diagnosis of carcinoma. Others contain multiple foci of vascular and capsular penetration but are fairly discrete masses. Highly invasive tumors have satellite nodules.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree