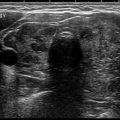
Fig. 6.1
Needle placement into the solid portion of a partially cystic thyroid nodule during FNA
Setup
The setup for FNA includes preparation of the ultrasound probe for use. There are several options for ensuring a clean and sterile probe. Sterile probe covers are commercially available and widely used, as are soaking systems designed for probe sterilization. Additional probe preparation procedures include cleaning with high-level disinfectant wipes which remain in contact with the probes for 3 min resulting in a sterilization level acceptable for ultrasound guidance. This process is shown in Fig. 6.2. Skin preparation includes washing the neck with chlorhexidine gluconate, iodine, or alcohol-based products, many of which are available in single-use packaging as seen in Fig. 6.3. Sterile draping also assists in keeping the field sterile.

Fig. 6.2
Ultrasound probe wrapped with a high-level disinfecting wipe in preparation for FNA

Fig. 6.3
Skin preparation for thyroid nodule FNA
Technique
FNA may be performed with or without local anesthesia. The type of FNA obtained may have a role in determining utility of anesthesia. If only a single suction-assisted pass is being performed, many institutions do not use local anesthesia. However, local anesthesia results in the increase of the patients’ comfort level and decrease of anxiety during the procedure [3]. Local anesthesia may be achieved with topical lidocaine cream, injected lidocaine, or lidocaine buffered with 8.4% sodium bicarbonate. Topical lidocaine requires application 30 min prior to the procedure and results in excellent anesthesia of the dermis. Injected lidocaine is performed immediately prior to FNA and allows for anesthesia of the dermis with a skin wheal and deeper anesthesia through the overlying strap musculature and into the perithyroidal soft tissues as seen in Fig. 6.4. Optimal anesthesia requires a 1 min wait time with lidocaine and 2 min wait time with buffered lidocaine. Buffering of lidocaine increases the pH of the solution and decreases pain associated with subcutaneous infiltration. Buffered lidocaine is available prepackaged, prepared in the hospital pharmacy, or mixed in the room with 10 parts 1% lidocaine and 1 part 8.4% sodium bicarbonate. Multiple studies from the emergency medicine, anesthesia, surgery, and dermatology literature have demonstrated less pain associated with percutaneous procedures with buffered lidocaine [3–6]. The speed at which the lidocaine is injected is thought to have an effect on patient pain with initial infiltration. However, Krause et al. found that while there was a decrease in perceived patient pain with slower infiltration, it was not statistically significant [7]. Complications with local anesthesia are uncommon. The topical preparations have been shown to irritate skin and cause pruritus. Allergies to lidocaine are reported and patients should be should be questioned about known drug allergies prior to biopsy.
Fig. 6.4
Local anesthesia administered prior to FNA
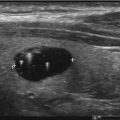
Ultrasound-guided FNA is usually performed using a long-axis technique with the needle lined up at the center of the short axis of the ultrasound probe as seen in Fig. 6.5. This long-axis technique allows for complete visualization of the needle from the dermis to thyroid nodule shown in Fig. 6.6. Targeting of the nodules may be performed with needle guides or with a freehand technique. Many vendors have a needle-directing device which can be attached directly to the ultrasound probe to assist in needle guidance. Although the freehand ultrasound guidance technique requires skilled eye-hand coordination, it allows for intra-nodule needle tip redirection to more solid and less vascular portions of the nodules to increase adequacy of aspirations. The needle size selected for FNAs ranges from 23 to 27 gauge; however the 25 g needle is the most often utilized. FNAs may be suction assisted or capillary technique, which is sometimes referred to as fine-needle capillary sampling or FNC. Slide preparation from capillary sampling is performed by direct smear onto slides that are immediately fixed in alcohol and sent to the pathology department for staining and interpretation. If suction is used, the samples are usually placed into liquid preservative which is made into thin prep slides or spun down into cell blocks for interpretation in the pathology department. The capillary technique has been shown to yield fewer nondiagnostic samples [8]. This is felt to be secondary to the negative pressure from aspirations causing more tissue damage and bleeding. Core needle biopsy (CNB) is also an option for pathologic diagnosis; however it has higher rates of bleeding complications and pain. Therefore, CNB is typically reserved for repeat biopsy after a nondiagnostic FNA.