Febrile Neutropenia
INTRODUCTION
Immune-compromised state refers to a change of the host defense systems that confer an increased susceptibility to infection. Neutropenia remains the major defect of the defense systems predisposing to severe infections. Fever in a neutropenic patient should be considered a medical emergency as it has been demonstrated that a delay in specific therapy is associated with up to a 70% mortality rate (1). In this chapter, we present the medical approach to fever in neutropenic patients by analyzing the predisposing factors, pathogenesis, diagnosis, and treatment.
DEFINITION
Fever in a neutropenic patient is usually defined as a single temperature of >38.3°C (101.3°F), or a sustained temperature >38°C (100.4°F) for more than 1 h. It has to be considered that neutropenic patients may experience clinical deterioration in the absence of fever and that concomitant steroid treatment may also conceal a fever.
Among neutropenic patients, two factors are associated with the increased risk of infection:
• Neutrophil count. The risk increases when the neutrophil count is below 1 × 109/l. The risk of infection increases further in patients with neutrophil counts of less than 0.1 × 109/l neutrophils.
• Duration of neutropenia. A low-neutrophil count and a protracted neutropenia (0.5 × 109/l for 10 days) are major risk factors for infection. A duration of neutropenia of more than 5 weeks is associated with an incidence of infection close to 100%.
Despite this, neutropenic patients remain a heterogeneous population that needs additional parameters that help to define the real risk of infection and tailor a more specific approach for each patient in this category. The risk factors for infection associated with neutropenia include advanced age, poor performance or nutritional status, low baseline and first-cycle nadir blood cell counts, and high-dose chemotherapy. Significant predictors for death, bacteremia, and length of hospital stay include advanced age, hematologic malignancies, disease burden, high fever, and low blood pressure on admission, pneumonia, and single or multiorgan dysfunction.
PATHOGENESIS
A number of predisposing factors other than neutropenia play a role in increasing the risk of infections in neutropenic patients with fever:
• Chemotherapy
• Intravenous or implanted devices
• Hypogammaglobulinemia (i.e., chronic lymphocytic leukemia, multiple myeloma, splenectomy)
• Defects in cell-mediated immunity (ALL, NHL, HD, therapy with fludarabine or alemtuzumab)
• Glucocorticoid therapy
• Disruption of normal anatomic structures
Chemotherapy not only affects the number of neutrophils but also impairs chemotaxis and phagocytosis. Either chemotherapy or radiotherapy-associated mucositis may affect the normal mucosal barrier, predisposing to bacteremia.
The existence of an impairment in neutrophil function preceding chemotherapy as in patients with myelodysplastic syndromes or in the presence of bone marrow failure due to tumor cell invasion predisposes to severe infection or death after chemotherapy (2).
Indwelling catheters and implanted devices pose a significant risk as they can allow access of skin flora directly into blood or subcutaneous tissues or represent a foreign body that bacteria can successfully colonize and infect. Immune defects associated with specific primary cancers may further impair the defense system as in hypogammaglobulinemia associated with CLL or multiple myeloma. Splenectomy predisposes to infection with encapsulated organisms such as Pneumococcus or Meningococcus.
An increased risk of infection has been observed in patients with Hodgkin’s disease as the result of a defect in cell-mediated immunity. Patients with ALL, patients with central nervous system tumors, and patients treated with glucocorticoids are also at increased risk of infections.
ETIOLOGY OF INFECTIONS IN FEBRILE NEUTROPENIA ASSOCIATED PATHOGENS
 BACTERIA
BACTERIA
About 65% of neutropenic patients with fever have infection (Table 17-1). In this group of patients, aerobic gram-negative bacilli represented the most frequent isolates (3). In the past Pseudomonas aeruginosa was the most frequent isolate responsible for septic shock and severe pneumonia, and empirical therapy regimens were designed to include antipseudomonal antibiotics. Since the 1980s, gram-positive bacteria have become the most frequent pathogens isolated from patients with febrile neutropenia. More aggressive chemotherapeutic regimens, widespread use of indwelling catheters, and antibiotic prophylaxis have contributed to the trend toward gram-positive infections (4). Coagulase-negative staphylococci are the most common isolates (2), although drug-resistant gram-negative bacteria are causing an increasing number of infections (3).
 FUNGI
FUNGI
It has been demonstrated that up to 20% of patients with neutropenia may experience an invasive mycosis, and this risk is further increased in patients with hematologic malignancies (3) (Table 17-1). Fungi are rarely the cause of fever early during neutropenia, but invasive fungal disease is usually encountered after prolonged neutropenia while on emperic antibiotics.
Risk factors for fungal superinfection include:
• greater than 7 days of profound neutropenia.
• use of quinolones as antibacterial prophylaxis.
• presence of a central venous catheter.
• persistence of fever after 3 days of antibiotic therapy (5).
Superficial and invasive candidiasis and invasive aspergillosis represent the most common infections. Candida albicans represents the most common fungal isolate in neutropenic patients followed by C. tropicalis, C. glabrata, and C. parapsilosis. The use of fluconazole as prophylactic therapy has been associated with an increased frequency of C. krusei.
Invasive aspergillosis may be due to Aspergillus fumigatus, A. terreus, A. flavus, and A. niger. Invasive aspergillosis is associated with a mortality rate approaching 80% in bone marrow transplantation patients with febrile neutropenia (6). The two most common sites of invasive disease are the lungs and the sinuses. Prolonged fever and nodular pulmonary infiltrates resistant to antibiotic therapy often represent the only clues to the diagnosis of invasive aspergillosis. A finding of nodular lesions surrounded by a low-attenuation area (“halo sign”) may be evident at a chest CT scan. Isolation from culture or histological detection of Aspergillus establishes the definitive diagnosis.
Fusariosis, Trichosporon beigelii, Blastoschizomyces capitatus, Saccharomyces cerevisiae, and Malassenzia furfur represent other emerging fungi.
EVALUATION
The initial evaluation of a febrile and neutropenic patient should include a detailed history and physical examination. Symptoms and signs of inflammation may be minimal or even absent in patients with severe neutropenia. A thorough physical examination should be performed, with particular attention to the skin, mucus membranes, sinuses, oropharynx, lung, abdomen, perirectal area, surgical sites, and intravenous lines. In the neutropenic patient, the response to bacterial infection may be misleading, with only minimal erythema and rash, and often without signs associated with cellulitis or abscess formation. All indwelling catheters should be carefully inspected. Lines should also be assessed for any malfunction as poor flow may be a sign of an infected clot.
The examination should include inspection of the perianal area. A digital rectal examination (and rectal temperatures) should generally be avoided. Stool softeners should also be given to patients to avoid hard stools or impaction. Patients should be reassessed daily as new sites of infection can become apparent even 72 h after the initial therapy. In addition, as the neutrophil count rebounds, symptoms and signs of an infection may become evident.
LABORATORY STUDIES
A basic evaluation should include a complete blood cell count with differential measurement of serum levels of creatinine, urea nitrogen, SGOT, SGPT, bilirubin, and electrolytes. Specimens should be obtained immediately for the microbiology laboratory, including two or more blood cultures from the device lumen and from a peripheral vein. Blood cultures should be repeated for persistent fevers.
A sample of sputum may be included in the microbiologic evaluation if the patient can produce it. Culture of urine samples is indicated if signs of symptoms of urinary tract infection do exist, in the presence of urinary catheter or if urinalysis is abnormal.
Lumbar puncture is not recommended as a routine procedure but should be considered if symptoms suggest a CNS infection.
Chest radiographs should be performed even in the absence of pulmonary infection. Even more likely to yield a diagnosis of pneumonia in the neutropenic patient is the high-resolution CT scan, as it frequently reveals pneumonia even in the presence of a normal chest radiography.
If localizing signs or symptoms are present, other tests should be considered, such as skin aspiration or biopsy for culture, stool for culture, and imaging of the CNS, sinuses, and abdomen.
TREATMENT
Treatment for patients with febrile neutropenia include antimicrobial agents and granulocyte-colony stimulating factor (G-CSF). Antibiotics are always administered empirically, ideally within 2 h of recognition (7), and should include appropriate coverage for suspected or known infections (Figure 17-1).
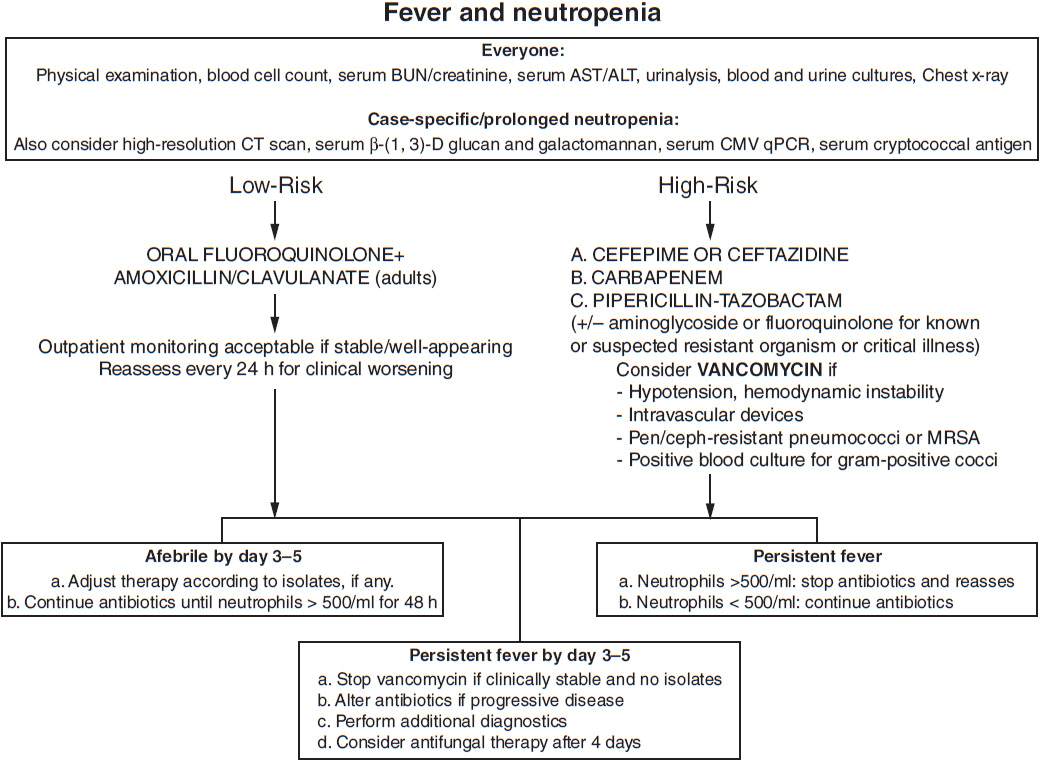
FIGURE 17-1 Practical approach to fever and neutropenia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree