26.1
Introduction
Falls are one of the most common health concerns facing older adults today. About one-third of community-dwelling persons over the age of 65 years and nearly one-half of institutionalized persons will fall each year . Many of these individuals will experience a recurrent fall within the following year . The risk of falling and experiencing an injury associated with a fall increases with age . Thus falls and fall-related injuries are likely to become even more consequential as the population over the age of 65 continues to grow.
In 2017 the Centers for Disease Control estimated that 3 million fall-related injuries were treated in emergency rooms in the United States, and one out of four persons treated in the emergency room for a fall-related injury was hospitalized . The majority of falls result in no injury or soft-tissue injuries, while about 5% of falls result in a fracture . Hip fractures, in particular, are closely associated with falls . Fractures of the distal forearm, pelvis, proximal humerus, ankle, and elbow are frequently due to falls as well . Fractures of the foot, face, and tibia/fibula are less commonly associated with falls .
The total cost of fall-related injuries is substantial. In 2015 the total cost of nonfatal falls in the United States exceeded $31 billion . Osteoporotic fractures cost $14 billion annually, with much of this expense directed at hip fractures .
Complications from fall-related injuries are frequent and may lead to death. In fact in 2015 in the United States, it was estimated that five older adults died every hour due to a fall-related injury with a direct cost of $638 million . The rate of deaths from falls has risen by 3%/year between 2007 and 2016 , with the greatest rise seen in individuals over the age of 85 years. If falls continue to rise at the current rates, seven fall-related deaths would be expected every hour by the year 2030 . Death from fall-related injuries increases with advancing age and number of comorbidities . Certain fall-related injuries, such as hip fractures, are associated with a high mortality within the first 3–6 months, particularly in men .
Even among persons not experiencing a fall-related injury, falls are associated with greater functional decline and a restriction of activities . Fear of falling is common among older adults who have experienced a fall, and it has been associated with depression and mobility impairment . As a result, fallers are more likely to become institutionalized even without experiencing an injury .
26.2
Risk factors for falls
The majority of falls are not the result of a single cause, but instead due to multiple interactions between an individual and the environment . Intrinsic characteristics may predispose an individual to fall, but environmental factors or acute illnesses are often the precipitating cause of the fall. Examples of precipitating events include pneumonia, a newly initiated drug, a recent hospitalization, or an unsafe walking surface . In such cases the individual is no longer able to compensate for the added stressor due to physiologic impairments and comorbidities that predispose to the fall.
26.2.1
Age-related risk factors for falls
The incidence of falls increases steadily with age until at least 80 years . In addition to the increasing number of comorbidities found more commonly with aging, this age-related increase in falls likely relates to normal physiologic changes associated with aging. Examples of physiologic changes found in repeat fallers include impaired proprioception, poor visual contrast sensitivity, impaired ankle dorsiflexion, decreased reaction time, and increased body sway . It is likely that these age-related changes in balance and muscle activation predispose older adults to fall.
Normally, balance is coordinated by input from the visual, proprioceptive, and vestibular systems. With normal aging, there is diminished input from each of these three systems. Depth perception, contrast sensitivity, dark adaptation, and accommodation all decrease with age . Poor visual acuity is associated with both an increase in falls and hip fractures . Sensorimotor variability in foot placement and loss of proprioception with normal aging contributes to an increased risk of falls . Finally, healthy elderly persons experience a loss of vestibular ganglion cells, myelinated nerve fibers, and sensory cells of the semicircular canals impairing vestibular function . These multiple insults to the maintenance of balance are clearly related to the increased risk of falling with advanced age.
In addition to age-related changes in balance, there are marked changes in muscle composition and muscle function with age. With aging, there is a decrease in muscle mass and an increase in muscle fat infiltration resulting in a loss of maximum strength . Fat infiltration of the muscle may be of particular importance as increased amounts have been associated with a 60% relative increased risk of hip fracture in older men and women . Decreased total skeletal muscle mass, as assessed by D 3 -creatine dilution, has been reported to be associated with an increased risk of injurious falls and the development of mobility limitations independent of age, comorbidities, cognitive function, and physical activity, in a cohort of older men . In addition to changes in muscle composition, normal aging is associated with changes in muscle function. Older individuals tend to activate proximal muscles, such as the quadriceps, before more distal muscles, such as the tibialis anterior, in response to perturbations of the support surfaces . This strategy may not be an efficient way to maintain postural stability. Elderly persons are also more likely to contract antagonistic muscles leading to a delay in postural compensation . Finally, balance recovery during a postural disturbance may be compromised by an age-related decline in the ability to rapidly develop joint torque using muscles of the lower extremities .
Changes in blood pressure regulation may impact falls in elderly persons as well. Baroreflex sensitivity and vascular compliance diminish with both normal aging and with hypertension . As nearly 75% of the US population over the age of 60 is hypertensive , the ability to regulate blood pressure may be significantly impaired in older adults. As a result, older persons are at risk of orthostatic hypotension during periods of decreased cardiac preload and tachycardia . Age-related changes in total body water and in the renin–angiotensin system also contribute to impairments in blood pressure regulation . As a result, stressors producing transient drops in blood pressure may lead to falls through impaired postural control or cerebral hypoperfusion in association with syncope .
26.2.2
Comorbidities associated with falls
A number of chronic diseases are more common with advancing age and are associated with falls. For instance, Parkinson’s disease is a common problem in the elderly and is associated with an increased risk of falling . Parkinson’s disease likely causes falls through a number of mechanisms, including increased rigidity of the lower musculature, inability to correct sway trajectory secondary to bradykinesia, hypotensive drug effects, and in some cases, cognitive impairment. Stroke is another neurological condition that has been consistently demonstrated to be an independent risk factor for falls . Stroke may increase fall risk through deleterious effects on visuospatial orientation, balance and mobility, dizziness, or depression . Dementia, regardless of etiology, is also a strong predictor of falls because it impairs judgment, orientation, and even gait . Not surprisingly, then, the incidence of hip fracture is greater in older adults with impaired cognition .
Osteoarthritis is another chronic medical condition that has been demonstrated to increase the risk of falls, irrespective of surgical interventions . Osteoarthritis of the hip or knee may increase falls by impairing a person’s leg strength, ability to maneuver around objects, or by causing pain. Postural stability may also be compromised due to the tendency to avoid full-weight bearing on the affected limb.
Chronic pain at any site, and especially more severe and polyarticular pain, has been associated with an increased rate of falls independent of arthritis severity and medication use . Similarly, foot pain has been associated with an increased risk of falls in community-dwelling older adults . It is postulated that pain may affect falls through its effects on gait, strength, and speed, or it may act as a cognitive distractor impairing an individual’s ability to maintain postural control.
Orthostatic hypotension by itself has not been consistently associated with falls . However, among persons with uncontrolled hypertension, orthostatic hypotension is an independent risk factor for falls . The risk of falling increases as the number of comorbidities increases . One community-based observational study found that 19% of persons with one risk factor and 78% of persons with four risk factors experienced a fall within 1 year . Frailty, a state of decreased physiologic reserve commonly observed in older adults with multiple comorbidities, is another independent risk factor for falls .
26.2.3
Medications associated with falls
The use of multiple prescription drugs is strongly associated with recurrent falls . Individual classes of medications, in particular psychotropic and cardiac medications, have been associated with an increased risk of falling as well.
Observational studies have shown that benzodiazepines, antidepressants, sedative hypnotics, anticonvulsants (phenytoin and phenobarbital), and neuroleptics are all associated with an increased risk of falls . The risk of falls among users of tricyclic antidepressants versus the newer selective serotonin-reuptake inhibitors (SSRIs) appears to be similar . There appears to be no difference in the risk of falls among users of typical versus atypical antipsychotics , among users of short-acting versus long-acting benzodiazepines , or among nonbenzodiazepine hypnotics ( Z -drugs) and benzodiazepines . As one might expect, the risk of falls increases in persons taking more than one psychotropic medication .
Cardiac medications have also been implicated as risk factors for falls in some, but not all studies. A community-based cohort study found that antihypertensive medications increased the risk of injurious falls among older adults, particularly those with a history of falls . Other observational studies found no association or a protective association between antihypertensive mediations and falls . Loop diuretics have also been associated with a small but statistically significant elevated risk of falls . These drugs may affect falls by exacerbating orthostatic hypotension or by causing urinary urgency and frequency that could cause a fall while hurrying to the toilet. Digoxin and type 1a antiarrhythmic drug usage have been associated with a mild increase in falls in some studies, possibly due to orthostatic drug effects or the underlying arrhythmia or heart failure . Analgesic medications are another class of drugs that may be associated with falls. A metaanalysis found a mild increase in risk of falls among patients using NSAIDs, opioids, and antiepileptics . Opioids and antiepileptics may contribute to fall risk through sedative effects, whereas NSAIDs could contribute to falls risk through side effects such as fluid retention or vertigo. It is challenging to separate the effects of these drugs on falls independent of the underlying medical condition.
Medication changes may result in a particularly vulnerable period of time with respect to fall and injurious fall risk. Two small studies of nursing home residents found a three- to fivefold increased risk of falls within 3 days of initiating a drug that affects the central nervous system . A new prescription or increased dose of a non-SSRI antidepressant was associated with a fivefold increased risk of falls within 2 days of drug initiation, with a decreasing risk of falls in the subsequent days . Among benzodiazepine users, risk of falls and hip fracture is highest in the 1–2 weeks following drug initiation . Fracture risk may also be elevated in the weeks following initiation of a short-acting opioid analgesic or antihypertensive medication .
26.2.4
External risk factors for falls
Around 10% of falls occur in persons with no identifiable risk factors for falling, suggesting that environmental risk factors are an important cause of falls . In fact, Tinetti et al. found that 44% of falls among community-dwellers were associated with environmental hazards . In addition, a home hazards assessment by a trained occupational therapist has been shown to be beneficial in reducing future falls in community-dwelling older adults at increased risk for falls . As this intervention decreased both indoor and outdoor falls, the mechanism of falls reduction is likely broader than simply modifying the structural safety of the home environment . This again suggests that falls are rarely the consequence of a single factor, but instead they are often the result of many interactions between individuals and their environment.
It is important to note that risk factors for indoor and outdoor falls differ. A community-based study of older adults demonstrated that indoor falls tend to occur in older women with poor health characteristics, while outdoor falls occur in younger, more physically active men .
26.3
Risk factors for injurious falls
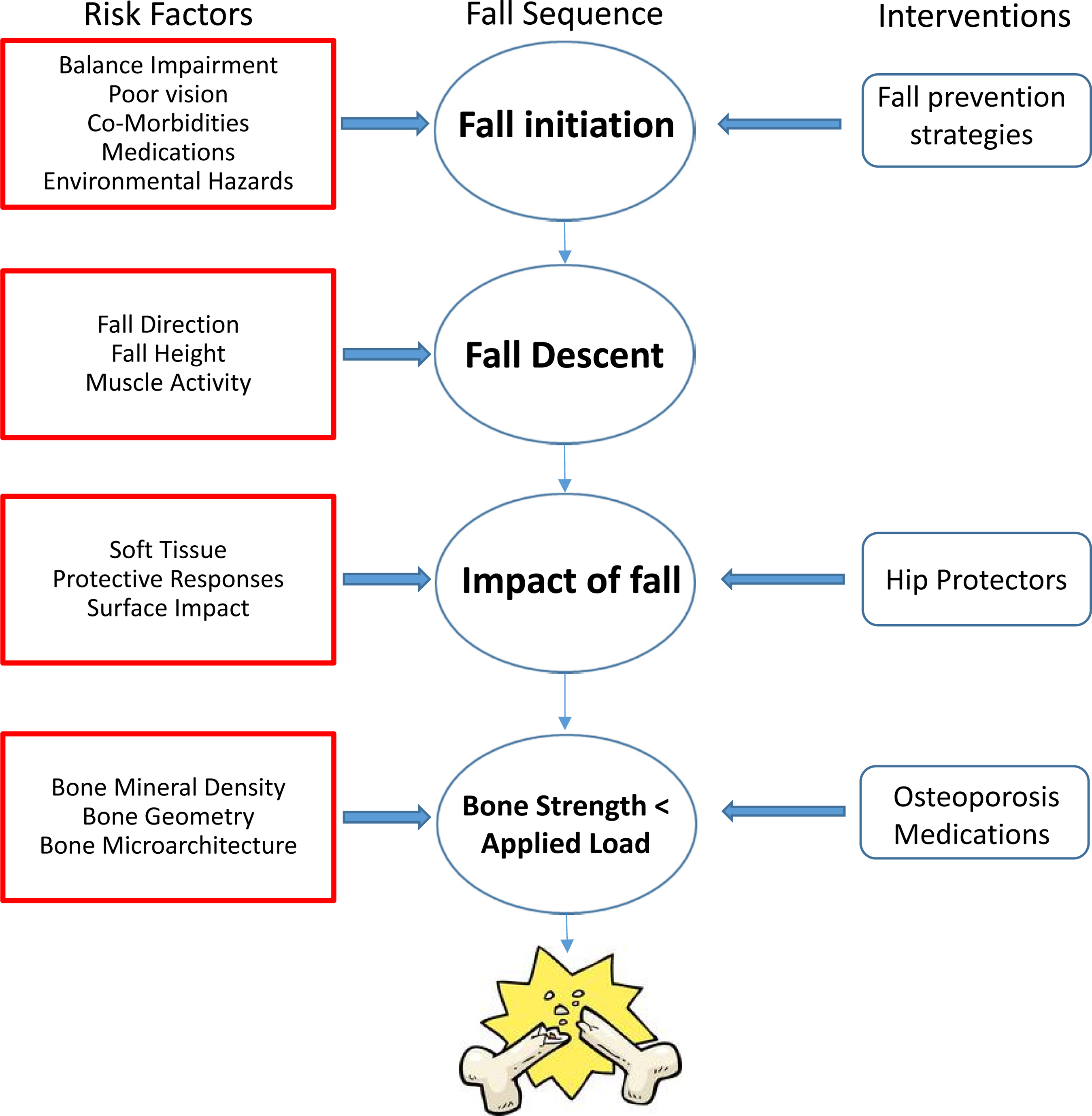
Similar to falls, injurious falls are typically multifactorial in origin. In addition to the typical risk factors for falls, both the nature of the fall descent and the fall impact influence the risk of injurious outcomes. Fractures comprise more than half of all serious fall injuries , and so bone strength is important: fractures do not occur unless the force applied to a bone exceeds the overall bone strength. Other fall-related injuries include hematomas, lacerations, and intracranial hemorrhage. Fig. 26.1 summarizes the interactions between fall initiation, descent, and impact, and as their relationship with bone strength and injury.
26.3.1
Factors involved in fall initiation
Few studies attempt to distinguish risk factors for injurious falls from noninjurious falls, and most of these studies do not distinguish between fractures and other serious injuries. However, studies suggest that the risk factors for injurious falls are similar to the risk factors for noninjurious falls . Cognitive impairment, multiple comorbidities, gait and balance abnormalities, and a recent history of fracture have all been associated with injurious falls in observational studies One prospective study looking specifically for risk factors associated with fall-associated fractures in community-dwelling individuals found that the fear of falling, lower extremity weakness, and poor visual acuity were predictive of fractures, whereas limited social participation actually protected against fall-associated fractures .
Risk factors for falls and hip fracture in postmenopausal women are similar. Physical findings, including an inability to rise from a chair without using one’s arms, poor depth perception, and poor visual contrast sensitivity, have all been associated with an increased risk of falls and hip fracture independent of bone mineral density (BMD) . In addition, psychotropic medications may increase the risk of fracture by impairing safety awareness or the ability to maintain balance. Alcohol has been postulated to increase the risk of injurious falls, but observational studies have not consistently shown this association . Nevertheless, heavy alcohol use (defined as greater than 1 oz/day) has been associated with an increased risk of hip fracture . It is prudent to council older adults with a history of falls about excess alcohol consumption.
Environmental hazards impact the risk of injurious falls. The routine use of bed rails or physical restraints in the nursing home and hospital has been associated with an increased risk of fall-associated injuries . A cluster-randomized trial in the hospital setting found no difference in falls rates after implementing bed alarms . In fact, a time series conducted in two poststroke and brain injury rehabilitation units suggested that removal of physical restraints may be associated with a decreased rate of falls . Falls were also decreased in the nursing home setting with an intervention that led to a decrease in the use of restrictive bedside rails .
Fractures may also be influenced by the timing and location of a fall. The majority of hip fractures in the community occurs during a fall at home in the absence of environmental hazards . Among community-dwellers, injurious falls are more likely to occur in the early morning or at night . Fall-related injuries in the institutionalized setting depend on the ambulation status of the resident . Nonambulatory residents are more likely to experience injurious falls associated with the use of equipment, while transferring, and from the height of a bed or chair. Ambulatory nursing home residents are at greatest risk of injurious falls during the night.
Finally, injurious falls may be influenced by the choice of footwear. A small laboratory study testing balance in older men using various shoe types found that shoes with thin, hard soles were associated with the best balance . However, a nested case–control study of men and women found that athletic shoes were associated with the lowest risk of falling, and shoes with increased heel height and decreased surface area between the sole and the floor were associated with a higher risk of falls . Slip-on shoes, sandals, and walking barefoot or in socks have been associated with an increased risk of falls with injury .
26.3.2
Factors involved in fall descent
Certain intrinsic characteristics place fallers at a higher risk of injury during fall descent. For instance, taller height has been demonstrated to be predictive of hip fracture independent of BMD in women and men . This may reflect the greater distance that taller women fall before striking the ground, which would allow for a greater force on impact .
The factor-of-risk is a biomechanical ratio of the estimated force on the hip during a sideways fall to femoral strength . As the factor-of-risk exceeds 1, one would expect a hip fracture to occur with a sideways fall. In men and women a one standard deviation increase in the peak or attenuated factor-of-risk has been associated with an increased risk of hip fracture .
The type of injury sustained is also related to the direction of the fall. Persons experiencing a hip fracture are more likely to report falling sideways , whereas wrist fractures are more strongly associated with forward or backward falls with an outstretched arm . Simulated fall experiments in healthy volunteers confirm that during lateral or posterolateral falls, the greater trochanter and lateral aspect of the leg is struck directly . Despite the observation that lateral falls are more closely associated with hip fractures, this simulation study showed that falling posteriorly or directly on the buttocks was associated with a greater force of impact on the greater trochanter than lateral or posterolateral falls. The explanation for the discordance in fractures may relate to the greater amount of soft tissue involved in posterior falls, which absorbs some of the impact from the trochanter .
26.3.3
Factors involved with fall impact
Increased soft tissue may potentially protect against injuries sustained during a fall. Soft-tissue stiffness and its dampening property decreases with age . In women, but not in men, decreased soft-tissue thickness has been associated with an increased risk of hip fracture . Women with both a lower and higher body mass index (BMI) have a greater risk of hip fracture as compared with women of normal weight with only some of this relationship explained by BMD . Weight loss has similarly been shown to be predictive of hip fracture in several studies irrespective of baseline weight . This may relate to a loss of BMD seen with both unintentional and intentional weight loss, but the loss of soft-tissue protection is perhaps a factor in the increased risk of fracture as well.
During a fall the surface of impact may relate to the risk of fracture. Nevitt et al. showed that falls on stairs or steps are more likely to result in injury . Decreasing surface stiffness through installation of foam mats in playgrounds or in nursing homes attenuates the initial maximum force experienced during a fall. Certain brands of foam flooring may reduce the estimated femoral impact force by 50% without altering gait and balance performance . This may prevent wrist fractures from standing height or less, but it is unlikely to affect fracture rates associated with falls from greater heights . A review of several small studies and abstracts of compliant flooring suggest that while falls may occur more commonly on compliant or carpeted floors, the risk of injury may be less .
Similarly, hip protectors are postulated to reduce the risk of hip fracture by decreasing the force on the greater trochanter associated with a lateral fall. A Cochrane metaanalysis found a marginal reduction in the risk of hip fractures among nursing home residents assigned to a hip protector (relative risk (RR) 0.81; 95% confidence intervals (CI) 0.66, 0.99), and no reduction in the risk of hip fracture among community-dwellers (RR 1.14; 95% CI 0.83, 1.57) .
The positive finding in nursing home residents should be interpreted with caution. Individual studies that found hip protectors to be beneficial in preventing hip fractures frequently randomized groups of residents to the intervention of hip protectors based on setting (i.e., nursing home ward). These methods may introduce bias in that the nursing home staff or residents selected to participate in the “treatment” units or facilities may differ from study participants from the control units. In the Cochrane metaanalysis, there was no longer a statistically significant reduction in the risk of hip fracture in the nursing home setting after excluding five trials that utilized a cluster randomization strategy (RR 0.93; 95% CI 0.74, 1.18) .
Other difficulties with interpreting hip protector trials include high rates of noncompliance. Studies report noncompliance rates with hip protectors to be anywhere from 30% to 76%, with discomfort, poor fit, and cognitive impairment being cited as the most common reasons for nonadherence . Not all brands of hip protectors have been tested in the laboratory or in clinical trials; therefore the brand of hip protector used may also influence study results . A simulation study estimated the attenuated force during a sideways fall provided by 26 different brands of commercially available hip protectors, and they found marked differences among products (range: 2.5%–40% force attenuation) . In this study, hip protectors with lower stiffness attenuated the greatest force.
Lastly, a faller’s instinctive ability to protect himself or herself during a fall may affect the risk of injurious falls. Compared with younger females, older women are slower at successfully moving their hands outward to protect themselves during a fall . This may be particularly relevant during lateral falls, where even among younger women the average time needed to successfully break a lateral fall was greater than during a forward fall. Cognitive impairment, visual impairment, arthritis, and psychotropic medications may further diminish one’s ability to catch oneself from a fall. Syncopal falls also prevent the fallers from actively protecting themselves.
26.3.4
Characteristics of bone associated with fracture
Fractures associated with falls occur when the force applied to a bone is greater than the overall bone strength. The strength of a bone is a function of its mineralization, turnover rate, geometry, and microarchitecture. Areal BMD measured by dual-energy X-ray absorptiometry is a composite measure of the overall size and mineral density of bone that has been shown to be predictive of fractures at a number of skeletal sites . While BMD is an important determinant of fall-associated fractures, BMD alone does not accurately estimate the absolute risk of fracture. Longitudinal studies in both men and women have found that BMD alone explains less than one-half of all nonvertebral fractures . Both age and a prior history of fracture are important contributors to the predictive value of BMD in determining absolute fracture risk . Many persons with moderate BMD remain at risk for fracture because they have fall risk factors. For example, the Study of Osteoporotic Fractures found that among women with total hip BMD T-score >−2.5, a history of a fall in the previous year increased the risk of hip fracture by 64% . Interestingly, this study also found the incidence of falls among women with and without osteoporosis as defined by low BMD and a history of hip fracture to be similar. This again highlights the limitations of using BMD alone to predict fracture risk.
Bone geometry and microarchitecture is also important in determining its overall strength. New imaging technologies allow for better visualization of the absolute number and width of bone trabeculae. Microarchitectural changes in trabecular number, size, and distribution have been shown to be predictors of bone fragility independent of BMD . With advanced age, there is an increase in cortical porosity and a decrease in cortical thickness, particularly among postmenopausal women. These unfavorable bone microarchitectural changes increase the risk of fracture independent of BMD or fracture risk models, such as fracture risk assessment tool (FRAX) .
26.4
Falls-prevention strategies
Although few data exist on the efficacy of falls-prevention strategies in reducing fractures, it is likely that such strategies are effective, as most nonvertebral fractures are associated with falls . The American Geriatrics Society (AGS) and British Geriatrics Society (BGS) have provided a summary of recommendations for falls prevention . The Centers for Disease Control Stopping Elderly Accidents, Deaths, and Injuries (STEADI) initiative is based on the AGS/BGS recommendations, and it encourages patients and providers to routinely consider falls-prevention strategies in an effort to avoid injury . Fig. 26.2 summarizes a reasonable approach to screening for falls in the community-dwelling population from the STEADI initiative. This includes asking about whether the patient has fallen in the past year, whether they are afraid of falling, and whether they feel unsteady while standing or walking.
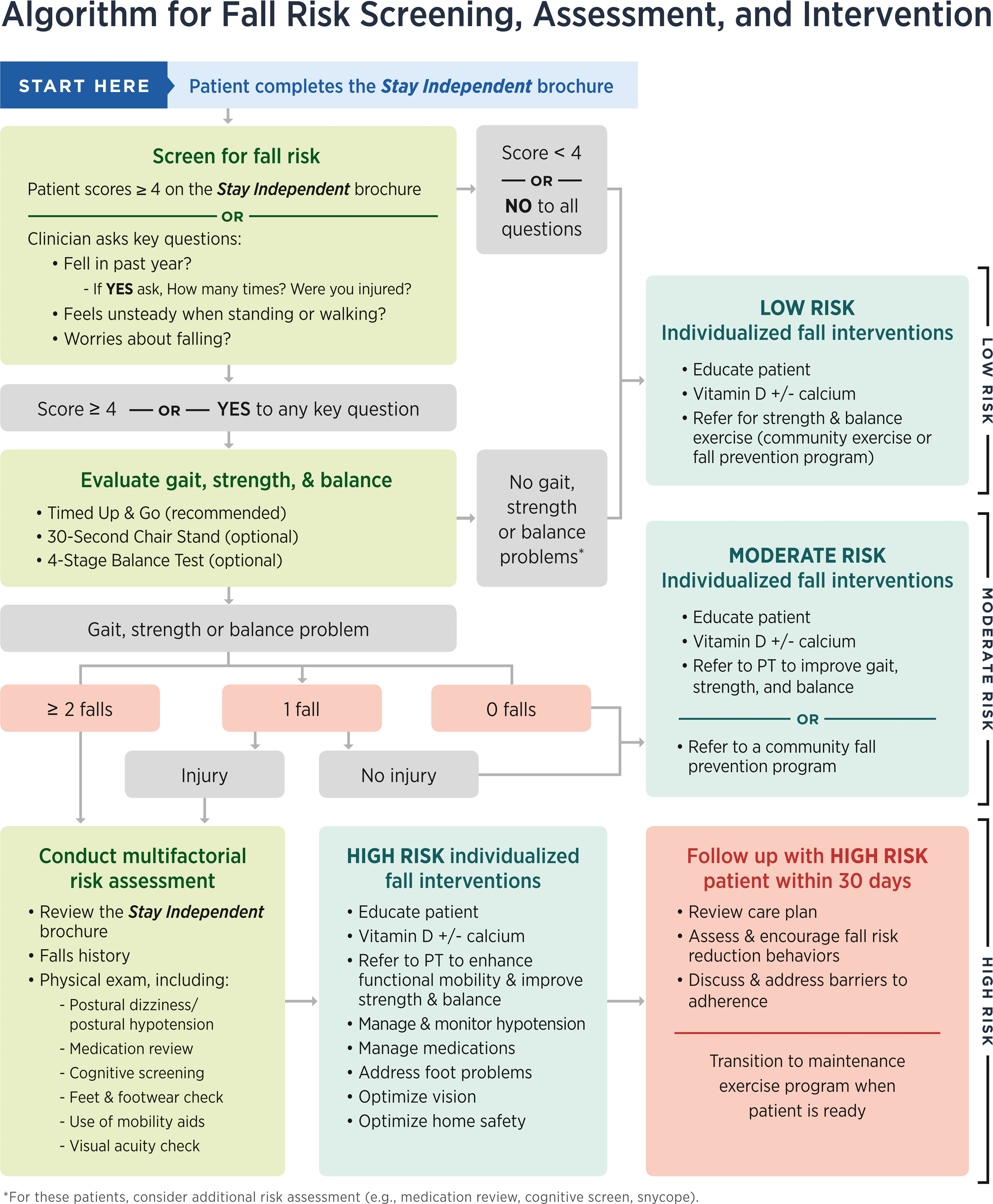
If patients have had a recent fall or are worried about falling and balance, clinicians are reminded to observe gait using a validated test. The “get-up-and-go” test is probably the most commonly used assessment in clinical practice. It consists of observing an individual stand up from a chair without their arms, walk across a room (about 3 m), turn around, walk back, and sit down without using their arms . This test may be graded on a 5-point scale or timed and has been demonstrated to be predictive of falls . The 30-second chair stand is another integrative clinical test of balance and strength. Alternatively, the Berg Balance Test is another test of integrated musculoskeletal function. The Berg test includes 14 items of balance, including timed tandem stance, semitandem stance, and the ability of a person to retrieve an object from the floor. Berg scores ≤40–48 have been associated with an increased risk of falls . Lastly, the performance-oriented mobility assessment (POMA) tests balance and gait through a number of items, including ability to sit and stand from an armless chair, ability to maintain standing balance when pulled by an examiner, and the ability to walk normally and maneuver obstacles . The Berg Balance Test and POMA are infrequently used in clinical settings, but they are used in research studies as an integrated measure of neuromuscular support. Individuals with any evidence of gait abnormalities and recurrent falls should have a multifactorial assessment of modifiable falls risk factors.
Because falls are typically multifactorial in origin, strategies for successfully reducing falls should address both intrinsic risk factors and environmental factors . A metaanalysis of falls reduction measures in the community setting found exercise and multifactorial interventions to be effective in reducing falls . Exercise programs utilizing more than one type of exercise (e.g., gait training, balance, and strengthening) were effective in reducing the risk of injurious falls among 21 trials (RR for falls 0.81, 95% CI, 0.73–0.90). A separate metaanalysis found that Tai-Chi exercise programs reduced the relative risk of falls and injurious falls by nearly 50% . For homebound older adults, programs, such as the Otago Exercise Program, that include in-home physical therapy and require fewer one-on-one sessions over the course of a year have been shown to reduce the rate of falls . Multifactorial interventions reduced the risk of falls significantly among 26 studies, but there was much heterogeneity among trials .
Home environment assessments with environmental modification performed by a health-care professional reduced the risk of falling among older adults at high risk for falls but not among adults at low risk for falls . One trial evaluating a placebo-controlled withdrawal of psychotropic medications found a significant reduction in falls . Other trials of deprescribing have been underpowered or have had variable success with implementation and falls reduction in the nursing home setting . Cardiac pacing may be effective in reducing falls in individuals with suspected cardioinhibitory carotid sinus hypersensitivity . Cataract surgery for the first eye , but not the second eye , was effective in reducing the rate of falls.
Footwear interventions may also be effective in reducing falls in the community setting. One small trial (109 participants) demonstrated a reduction in falls among older adults wearing a nonslip shoe covering during icy conditions (RR 0.42; CI 95%, 0.22–0.78) . A multifaceted podiatry intervention consisting of foot orthoses, advice on footwear, subsidy for footwear, and foot and ankle exercises reduced the risk of falls over 12 months in community-dwellers as compared with usual care .
Despite the success of falls prevention in these standardized clinical trials, the pragmatic implementation of falls prevention across healthcare systems has proved challenging. In a cluster-randomized trial that included 86 primary care practices across 10 healthcare systems, a multifactorial intervention delivered by trained nurses was not effective in reducing the rate of injurious falls (HR 0.92, 95% CI 0.80, 1.06) . Adherence to some recommendations was low in this study: only 29% of patients with a high risk medication identified and only 50% of patients with an environmental hazard identified were willing to address these risk factors. It is critical that providers work with patients on their readiness to accept falls prevention interventions.
The association between vitamin D supplementation and falls is complex. In community-dwellers, metaanalyses of modest vitamin D supplementation found no beneficial effect on falls or fractures . High-dose vitamin D supplementation (50,000 IU annually) has been associated with an increased risk of falls and fractures . However, in nursing home residents, vitamin D supplementation more consistently decreased the rate of falls (4512 participants, four studies, Incidence Rate Ratio (IRR) 0.72, 95% CI 0.55, 0.95) . These seemingly discrepant results in nursing home residents may be explained because the majority of nursing home residents are vitamin D deficient, often with levels below 20 ng/mL. The AGS panel review of data regarding vitamin D stated that many older adults will need supplementation with at least 1000 IU daily in order to achieve sufficient serum 25-hydroxyvitamin D levels for fall and fracture prevention . Given its efficacy in nursing home residents and its low risk for harms, it is reasonable to supplement vitamin D in frail, older adults, particularly those with known osteoporosis, in an effort to prevent injurious falls.
Interventions that were not successful in reducing falls in the community setting based on one trial include cognitive behavioral therapy and nutritional supplementation . Assessment and correction of visual impairment and education were not effective in reducing fall risk in a few studies.
In nursing homes or other residential care centers, the prevalence of risk factors for falls and the rate of falls and fractures are much higher than in the community setting. In fact, nearly 10% of all hip fractures in the United States occur in the nursing home setting . Perhaps, not surprisingly then, clinical judgment has been demonstrated to be superior to performance tests, such as the timed get-up-and-go test, in predicting falls . To date, fall intervention trials in the nursing home setting have been met with limited success. A Cochrane review suggests that among 17 trials, there was no clear effect of exercise interventions on the risk of falls . Similarly, the effect of multifactorial interventions on the risk of falls was mixed in 10 studies. Standardized effective measures to prevent falls in the nursing home setting are needed.
26.5
Methodologic approaches to analyzing falls
Falls are a common and recurrent outcome. This poses unique methodologic consideration when choosing a statistical method to study falls. Traditional statistical analyses of events, such as logistic regression or Cox proportional hazards regression, consider only the first fall, which fails to account for recurrent outcomes. Further, the assumptions of traditional Poisson regression are likely to be violated in falls studies because falls are rarely normally distributed (i.e., many persons will have no falls and a few persons will have a high number of falls). It is important to consider the competing risk of death when studying falls and fractures in older adults with multimorbidity. If the competing risk of mortality exceeds the event rate and when follow-up time is long, substantial bias can occur when competing risks are ignored .
Several accepted statistical methods to analyze recurrent events such as falls exist. Negative binomial regression is based on a Poisson model, but it allows for overdispersion of the outcome . It is relatively easy to interpret, as it compares the rate of falls between groups. Negative binomial regression accounts for each individual’s time spent in the study, and therefore, it is a good option when follow-up is variable. In contrast, in the Anderson–Gill and marginal structural models, participants are included regardless of whether follow-up is complete and beyond the first event of interest (i.e., fall) . The Anderson–Gill Cox model is least affected by differential rates of falls among participants who drop out of a study as compared with participants who remain in a study . Thus this model may be appropriate when the drop-out rate in a study is high. When falls are measured at discrete time intervals (e.g., quarterly by self-report), it is possible to use marginal structural models such as generalized estimating equations to model falls with time-varying confounders.
The decision whether or not to include prior history of falls in a model depends on the research question. When identifying risk factors for falls, it is important to include the prior history of falls, whenever possible, given the strong relationship with future falls. However, when modeling rates of falls, it may unnecessarily lead to an over adjustment, particularly in high-risk populations such as the nursing home.
Despite widespread availability of most of these methods, a review of 83 randomized control trials of falls prevention found that only 31% utilized a statistical method to analyze recurrent events . It is important that future studies of falls prevention use appropriate statistical methods to analyze recurrent events so that comparisons can be made between studies.
26.6
Summary and implications
Clearly, there is a strong association between falls and osteoporotic fractures. Although most falls result in minor injuries, 5% of falls result in a fracture. Hip fractures, in particular, are closely associated with falls. As a result, falls lead to an increased morbidity, mortality, and use of institutionalization with its associated costs.
Many elderly persons are at high risk of falling secondary to perturbations in balance, strength, and vision, and due to the increasing comorbidities of advancing age. Acute illnesses, medication changes, and environmental factors are often the inciting events that precipitate a fall in these high-risk individuals. Persons with multiple risk factors are at the highest risk of falling.
Although few studies have addressed risk factors for injurious falls separately from noninjurious falls, most data suggest that these risk factors are similar. In addition, intrinsic characteristics of the faller such as taller height, lower BMI, a family history of hip fracture, and the ability of the faller to protect himself or herself influence the risk of fall-associated fractures. Bone strength, as determined by both BMD and bone geometry, is important in predicting fracture risk. As newer technologies such as quantitative computed tomography (QCT) and high-resolution peripheral QCT or MRI continue to emerge, a more accurate measure of bone microarchitecture may also be possible in clinical practice. Finally, environmental factors, including the timing and direction of the fall, surface of the floor, use of assisted devices, and even footwear, may impact the risk of injurious falls.
All physicians should regularly ask older adults about falls and fear of falling. Falls-prevention strategies shown to be effective in reducing falls in the community setting include exercises for improving strength and balance performed in a group setting or individually, Tai-Chi, multifactorial interventions, a home hazards assessment for persons at high risk for falls, removal of psychotropic medications, and certain footwear and podiatry-based interventions. In the nursing home setting, only vitamin D supplementation has been consistently shown to prevent falls. Although there are no data to support these interventions’ work to reduce the incidence of fragility fractures, there is good reason to believe that they will.
Several accepted statistical methods to analyze recurrent events such as falls exist, including negative binomial regression. It is important that future studies of falls prevention use appropriate statistical methods to analyze recurrent events so that comparisons can be made between studies.
As the population over the age of 65 years continues to grow, osteoporotic fractures will likely become an even greater problem. Currently, much effort is being applied to finding cost-effective criteria for the initiation of pharmacological treatment in persons at high risk of fracture; however, less emphasis has been placed on the importance of initiating nonpharmacologic falls-prevention strategies in an effort to decrease fractures in this same high-risk population. New health-care delivery models that successfully implement falls-prevention strategies are desperately needed. Future research to prevent injurious falls in community-dwellers should not only concentrate on improving bone density and strength but also on implementing evidence-based falls-prevention strategies. In the nursing home, only vitamin D supplementation has proven efficacy in reducing falls, and it is critical that new falls-prevention strategies are developed.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree