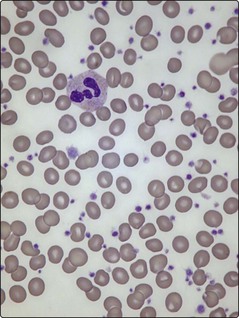
33 Platelet counts can be as high as 2000 × 109/L and usually exceed 450 × 109/L (the normal range is 150–400 × 109/L) (Fig 33.1). In practice, there is no single test to specifically identify ET – diagnosis is often a process of exclusion. As thrombocytosis may accompany a wide range of disorders including infections, inflammatory conditions, malignancy and iron deficiency, a thorough history and examination is mandatory. The lack of a measurable ‘acute phase response’ (i.e. normal erythrocyte sedimentation rate, plasma viscosity and fibrinogen) increases the likelihood of ET as opposed to a ‘reactive’ thrombocytosis. Even where there is an acquired JAK2 gene mutation, other myeloproliferative disorders must be excluded. Bone marrow examination is worthwhile to exclude chronic myeloid leukaemia (absence of Philadelphia chromosome), myelofibrosis or myelodysplasia, and to check iron stores. Patients with polycythaemia vera may have thrombocytosis, while patients with ET can have an increased red cell mass. In practice such patients are better diagnosed as having myeloproliferative neoplasms rather than forced into either category. Only about 5% of all raised platelet counts are due to ET, but persistence of the count above 1000, particularly with coexistence of thrombosis or haemorrhage, makes it the likely diagnosis. Abnormal platelet function tests suggest ET rather than a reactive thrombocytosis.
Essential thrombocythaemia and myelofibrosis
Essential thrombocythaemia
Diagnosis
Essential thrombocythaemia and myelofibrosis