Cutaneous tumors
Nonmelanomas
312
Melanomas
86
Basal cell carcinomas
282
Superficial spreading melanoma
84
Squamous cell carcinomas
26
Nodular melanoma
2
Cutaneous lymphomas
2
Merkel cell carcinomas
1
Kaposi’s sarcoma
1
Risk Factors
In all races UV radiation is the major risk factor for the onset of nonmelanoma cutaneous tumors (BCC and SCC), which appear in fact predominantly in photo-exposed areas, in almost 90 % of cases in the head and neck. Other possible risk factors are radiodermatitis, burns scars, ulcers, chronic infections and immunosuppression, genetic diseases with albinism and xeroderma pigmentosum, or chronic diseases like systemic lupus erythematosus [2].
Melanomas
Epidemiology
In the USA more than 60,000 new cases of melanoma are registered every year, and melanomas represent the sixth most frequent neoplasia in men and the seventh in women [2]; the increase in the incidence of melanomas both in the USA and in Europe is estimated at between 3 and 7 % annually among the Caucasian population (less among blacks) and represents one of the tumors with the highest mortality rates and at an age more than a decade lower than that of other solid tumors (breast, colon, lung, and prostate cancers) [14]. This increase in incidence is considered to be due to a greater awareness among the population thanks to prevention campaigns and so to a more likely early diagnosis with the result that there is no parallel increase in mortality. A detailed analysis of melanoma cases registered in the 20-year period 1988–2006, subdivided according to thickness (four different groups: <1, 1.01–2, 2.01–4, >4 mm), shows that all four categories record a significant increase in incidence, with a greater increase in cases of thin melanomas in women and of thick melanomas in men [15].
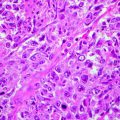
Two principal types of registrable melanomas have been identified with two different etiopathogenetic mechanisms: the most common melanoma, which has a superficial diffusion arising de novo or on a preexisting melanocytic nevus and develops as a melanoma in situ with a subsequent horizontal growth and only in much later phases a vertical growth with a progressive metastatic potential; and a second type of melanoma, arising de novo, which has a rapid vertical growth (Breslow index of thickness at diagnosis >1), an immediately aggressive biological behavior, a high metastatic potential, and an unfavorable prognosis [16], the pathogenetic mechanism of which is not yet well known. Thin melanomas with a slow evolution, instead, seem to be connected to exposure to ultraviolet radiation, both UVA and UVB, with a variable risk factor in terms of accumulated doses of radiation, type of exposure (intermittent or continuous), and sunburn [17]. Additionally, the use of tanning lamps, which became widespread in the 1980s, has caused an increase in the risk of the development of melanoma in relation to the accumulated dose of ultraviolet radiation. In fact, a recent study by the University of Minnesota has revealed an increase in this risk by a factor of 1.74 in subjects who are habitual users of UV tanning lamps compared to nonusers, with a close correlation between the increase in risk and the total dose of UV radiation (in terms of the total hours of exposure and number of sessions) [18] without overlooking the age of the subjects who are tanning lamp users. In fact, the International Agency for Research on Cancer has considered tanning lamps as carcinogenic – causing all types of cutaneous tumors – highlighting how the risk of developing a melanoma is increased by 75 % in subjects who regularly use tanning lamps up to the age of 30 [19].
It is obvious how the close correlation between environmental UV radiation and the development of melanoma influences directly the incidence in terms of ethnicity and latitude and indirectly the onset sites and the differences between genders [20].
From analyzing the cases of melanomas in relation to solar exposure and latitude, it would seem that intermittent exposure, for the most part recreational, leading with a greater probability to solar burns of various grades, represents an important risk factor at all latitudes. Instead, chronic exposure, for the most part occupational, representing a risk in terms of total doses of radiation absorbed, would seem to have a greater influence on the risk of developing melanomas at low latitudes, considering also the type of skin of the resident populations [21]. In Norway the incidence of melanomas in the last 50 years has shown a notable increase, with a difference of about two to three times between the south and north. The area of the body most seriously affected turns out to be the trunk in both sexes. These data would suggest that at these low altitudes the predominant risk factor is the phototype, which is to be correlated more to recreational solar exposure than to chronic exposure during the entire lifetime. Similar considerations can be made about the rest of Europe, with the only difference that in the south of Europe, there seems to be a difference in the site of onset also with respect to gender: the trunk appears to be the predominant site for men and the legs for women [22].
This same prevalence for the trunk in men and the legs in women in terms of the site of onset of the melanoma is similarly recorded in other parts of the world: Asia, Latin America, the USA, and Canada [20, 23–25].
These observations have suggested that the difference in the onset site of the melanoma between the two sexes can be in some way connected to sexual hormones. It is interesting to note that the melanomas of the trunk frequently present mutations of the BRAF gene, closely associated to a polymorphism of MC1R, the expression of which is modulated by the sexual hormones [26]. It is true that other differences between men and women could explain the difference in the anatomic site of the melanoma: clothing, lifestyle, occupations, solar exposure, and the different degrees of attention to preventive behaviors between the sexes [27]. The different habits of life explain indeed the different incidence of melanomas in the Middle East, where an incidence among men almost two times greater than that of women is recorded, probably because women are more protected by their covering clothing and by their limited presence in the open air, both for work and leisure [28].
A separate category is represented by the colored population of Africa, in which melanomas are extremely rare, for the most part in the acroposthion, and have an unfavorable prognosis, often due to the lateness of diagnosis. The sites most affected are those less rich in protective melanin: the subungual exostoses and the palmoplantar areas. Risk factors additional to the intense doses of UV radiation are immunosuppression (also from HIV), chronic diseases, and genetic diseases, like albinism, in which the protective constitutional conditions are less than those typical of that race [29].
Melanomas of the Mucosas
The melanoma of the mucosa is a rare form of melanoma distinct from the cutaneous form by reason of its biological behavior and pathogenesis. It accounts for 1.3–1.4 % of all melanomas, appears most frequently in colored races, and is located predominantly (up to 50 % of cases) in the head and neck area [30]. It shows an onset at a later age compared to cutaneous melanomas and often, considering that this site is richly vascularized, is already metastatic at the time of diagnosis, with the result that it has a very unfavorable prognosis [31].
The risk factors are to a very limited degree ascribable to UV radiation and recognize instead other mechanisms linked to potential tumor promoters like tobacco. Thirty percent of melanomas of the oral cavity develop on the melanoses, and it is well known that cigarettes cause an increase in the melanocytes [32]. Survival to 5 years varies from 12 to 34 % according to the location of the first lesion and obviously to its thickness at the time of diagnosis [31].
Melanomas at Pediatric Age
Melanomas at pediatric age, understood as the period from the uterus to the age of 21, are rare, but not insignificant, and are however increasing, although with some differences in the various age ranges (congenital/neonatal melanomas 3.8 %, infant melanomas 23 %, adolescent melanomas 73.2 %) [33]. On average the pediatric melanoma represents 1–4 % of all cases of melanoma and 1–3 % of neoplasias at pediatric age [34]. In the last few decades, this incidence has shown an increase of 3 % per year, from 1973 to 2001, with a slight prevalence in females, fortunately with an improvement in survival of 4 % per year [35], possibly thanks to a more widespread primary prevention and a more effective secondary prevention.
In melanomas of the pediatric age, a predominant role seems to be played by genetic conditions of susceptibility with mainly endogenous risk factors, such as the total number of nevi, the presence of congenital nevi of average or large dimensions (transformation risk from 2 to 10 %), a light phototype, and the presence of freckles and burns from solar exposure in childhood [36], the latter an exogenous risk factor but with some predisposition. Other predisposing factors are congenital diseases with an alteration in the reparative capacity of the DNA after UV radiation damage (e.g., xeroderma pigmentosum), which show an increase of 2,000 times in the risk of developing melanomas in pediatric age and immunosuppression conditions (iatrogenic, infective, and hematological disorders) with an increase in risk of three to six times [34].
Melanomas: Mortality
Despite a significant increase in the incidence of melanomas in the last few decades, a comparable increased trend of mortality has not been registered. The number of deaths due to melanomas appears stable or only slightly increased, and an improvement in survival rates has been universally recorded [37]. Such a divergence would seem to be due principally to an improvement in early diagnosis, thanks to campaigns of primary and secondary prevention, and to the optimization of surgical techniques with the support of a more effective adjuvant therapy [38]. The prognosis of the melanoma is directly proportional to the thickness of the original lesion: in fact, the initial stages of the melanoma are fully manageable surgically with a survival rate at 5 years which reaches 95 %. In contrast, for more advanced forms of the melanoma, with a metastatic condition, the prognosis is unfavorable on account of the aggressive biological behavior of the disease and the poor response to the systemic therapies currently available [39].
From these findings we conclude that early diagnosis is the only effective weapon to reduce the mortality rate of this neoplasia.
Prevention
By prevention we mean the implementation of the most suitable measures to prevent the appearance of something damaging. The prevention of melanomas is therefore realized through “primary prevention,” aimed at the identification of risk factors, endogenous and exogenous, and at the containment of these factors and/or their effects, combined with “secondary prevention,” aimed at reducing the number of deaths due to melanomas, principally through early diagnosis, given that this seems to be the key factor for the reduction in the mortality of this neoplasia.
Risk Factors
Traditionally, the risk factors identified for melanomas are divided into endogenous and exogenous factors. In the first group we include phototype; the total number of nevi – the risk of the transformation of each single nevus is estimated at around 1 out of 200,000 per year [40] – a variable percentage between 22 and 50 % of diagnosed melanomas show histologically an origin associated with nevi [41] and a specific genetic susceptibility; in the second group we include first and foremost natural and artificial ultraviolet radiation, to which we can then add other risk factors such as socioeconomic condition, habits of behavior, and occupational activity.
Endogenous Risk Factors
The exact pathogenesis of melanomas remains as yet not completely clear, but an important role seems to be ascribable to a polymorphism of certain genes involved in the determination of the color of the skin and hair, in the case of sporadic melanomas, and of certain other genes, in the case of familial melanomas. We can subdivide the endogenous risk factors into two groups: “traditional,” among which we include phototype, the total number of nevi above 50, and the presence of atypical nevi and freckles; and “new” risk factors, identified thanks to the development of cellular and molecular investigation techniques, definable in terms of genetic susceptibility to the development of melanomas.
In a variable percentage of the cases of melanomas, in fact, we can find a positive familial anamnesis for the same disease: the prevalence varies from 1.3 % in studies conducted in the north of Europe to almost 16 % in studies conducted in Australia. This confirms that there exists a great variability in the family history of melanomas, probably because environmental risk factors are decisive in terms of the onset of the disease even if on a predisposing phenotypical and genotypical base [42].
It is clear that melanoma originate from the combination of a series of genetic and epigenetic events: for the onset, progression, and metastatic diffusion of the neoplasia, numerous irreversible changes must take place within the genome – mutations, deletions, and an amplification of the target gene – but also a complete series of epigenetic phenomena, that is, modifications in gene expression, without an alteration of the DNA (DNA methylation or histone deacetylation) seem to be decisive [43]. Currently four genes have been identified associated with a condition of susceptibility to genetically determined melanomas: CDKN2A, an oncosuppressor important in the control of the entry of the cell into the cellular cycle, CDK4, ARF, and BRAF [44]. Another three loci seem to be involved: a locus on chromosome 1p22 [45], a locus on chromosome 9q21 [46], and, more recently identified, the locus 20q11.22 [47].
Other susceptibility genes, but with a lower penetrance, involved in the melanogenesis and in particular in the definition of the relationship between the eumelanin and pheomelanin and therefore in the determination of the color of the skin and hair, are MC1R, αMSH, OCA2, ASIP, TYR, and TYRPT1 [48–50]. Such genes, in that they are involved in melanogenesis, are therefore directly and/or indirectly responsible for the determination of another endogenous risk factor, the most important, the phototype. The variability of cutaneous pigmentation depends not only on the dimension, shape, and distribution of the melanosomes in the epidermis but also on the quantity of eumelanin and pheomelanin produced by the melanocytes and their relationship. The incidence of melanoma, in fact, shows a wide variability according to race in terms above all of the color of the skin in that this represents the greater or lesser capacity of the individual to cope with damage due to ultraviolet radiation (UVA and UVB), with a factor of protection 13 times greater for blacks as opposed to whites [51]. In addition, genetic or epigenetic phenomena responsible for alterations in the functions of such genes and their products can contribute to render the skin still more sensitive to UV-induced damage of the DNA and so predispose the subject to the development of melanoma and nonmelanoma cutaneous tumors [52].
This supposed genetic susceptibility, which puts blood relations potentially more at risk of developing melanomas compared to the general population, implies in the affected subject a relatively greater risk of developing a secondary melanoma. Unfortunately, these molecular alterations have not to date produced useful data relating to the possible plasma and/or tissue biomarkers of the disease and/or their progression [53].
Exogenous Risk Factors
The direct pathogenetic role of ultraviolet radiation (UV) is by now universally recognized for nonmelanoma cutaneous tumors (BCC and SCC) and strongly probable for cutaneous melanomas. The UV radiation spectrum is subdivided on the basis of wavelength (λ): UVA radiation accounts for about 94 % (λ: 320–400 nm), UVB about 5 % (λ: 280–320 nm), and UVC about 1 % (λ < 280 nm). The Earth is not at risk from UVC radiation because this is normally absorbed by the ozone layer and therefore does not reach the surface, but, instead, it is extensively affected by the other types, the energy of which is absorbed by the cellular proteins and the DNA, sometimes with mutagenic effects [54].
At the cutaneous level, the UVA penetrates deeply and is not absorbed directly by the DNA of the keratinocytes but can damage the cells through oxidative stress. The UVB radiation, instead, is absorbed by the epidermis and can cause direct damage to the DNA with the formation of dimers, thymine, cytosine, and other potentially carcinogenic photoproducts. Some forms of melanoma, connected to some well-known genetic alterations, could recognize analogous pathogenetic mechanisms at the level of the DNA of the melanocytes [55]. Knowledge of the genetics of the melanocytes and of melanogenesis together with data relating to the interactions of UV radiation with the DNA demonstrates how intense solar exposure with the aggravating factor of burns, even at a young age, can in fact result in the development of melanomas. It has been suggested that two different mechanisms of interaction between UV radiation and melanomas exist that involve different genes: a total of intermittent intense solar exposure would promote the development of melanomas on the trunk (a zone not daily photoexposed) in young patients with numerous nevi; and chronic photo exposure would promote the development of melanoma in photo-damaged areas at an advanced age in subjects with a history of photo-induced cutaneous carcinomas [56].
In the same way as solar radiation, the artificial ultraviolet radiation of tanning lamps increases the risk of the induction of melanoma and in general of cutaneous tumors.
Primary Prevention
Primary prevention has as its objective the reduction of damage due to ultraviolet radiation and therefore focuses on the organization of education campaigns to make the population aware of the need to use sun protection products of a suitable protection factor in accordance with phototype, applied in the correct quantity and with the correct frequency; to wear hats and sunglasses; to take photo-protective supplements; to abstain from direct solar exposure in the midday period to avoid sunburn and to permit the melanocytes to activate themselves in the synthesis of new protective melanin; and to avoid intermittent intense exposure in favor of a gradual progressive and safe solar exposure [57]. In parallel, the use of tanning lamps and tanning beds is discouraged [58].
Secondary Prevention
The objective of secondary prevention is the early diagnosis of the disease that, in the case of melanoma, turns out to be the only potentially successful weapon, bearing in mind the poor response to the therapies currently available.
The first objective of this prevention is certainly the identification of subjects at risk. Potential risk factors include the following: a personal history of melanomas (the risk of secondary melanomas is 5–8 %); a positive familial anamnesis of melanomas (two or more affected family members within the second degree of relationship); the number of nevi (the risk progressively increasing in accordance with the number of nevi – see Table 2.2); the presence and/or history of dysplastic nevi (the risk increasing by 6.3 times for more than 6 atypical/dysplastic nevi); a light skin (risk 4 times); blue eyes and red hair (risk 2 times); a personal history of cutaneous carcinomas (risk 2–3 times); sunburns and excessive sun/UV lamp exposure (risk 2–3 times); males as opposed to females; age (the risk of the development of melanomas increases with age); and new pigmented lesions appearing after 50 years of age [59].
Table 2.2
Index of the increase in the risk of developing cutaneous melanomas
Total number of nevi | Increased risk of melanoma (number of times) |
|---|---|
11–25 | 1.6 |
26–50 | 4.4 |
51–100 | 5.4 |
>100 | 9.8 |
1–5 atypical nevi | 3.8 |
More than 6 atypical nevi | 6.3 |
Different strategies have been proposed to improve the early diagnosis of melanomas including campaigns of education of the population for cutaneous self-exploration, the awareness raising of general practitioners about routine examinations of the entire integument also on the occasion of consultations for different reasons, mass screening campaigns, and the development of noninvasive technologies auxiliary to clinical diagnosis. Large-scale statistical investigations have demonstrated the probable utility of mass screening: the data are however insufficient to confirm unequivocally the benefits of such an effort [60–63].
The patient certainly plays a fundamental role in the diagnosis of melanomas: more than 70 % of melanomas are “suspected” by the patient himself/herself or by friends or family members. In recent years, thanks also to better information (in the mass media, newspapers, magazines, etc.), people have shown an improvement in the early recourse to the doctor. Today, the appearance of a mark in evolution or the presence of a change in a nevus, present for some time, is rightly interpreted by the inexpert patient as warning signs. Therefore, the efforts made since the 1980s, the years in which the ABCD criterion was introduced (a useful acronym to remember the warning signs of a cutaneous pigmented lesion: Asymmetry, Border, Color, Dimension) [64], in the education and awareness raising of the population in terms of self-diagnosis, a noninvasive and inexpensive procedure, have been bearing fruit [65, 66]. In the case of nodular melanomas with lesions characteristically with a rapid growth – estimated at around 0.4 mm per month – it is frequently (41 % of times) the patient himself/herself who notices the lesion, but unfortunately at an already advanced stage of development (a thickness >2 mm), with negative repercussions in terms of prognosis [67]. The “evolution” of the cutaneous lesion is therefore very important but it is not included in the ABCD rules, unless the acronym is widened to ABCDE, where the E refers to the tendency of the lesion to Evolve in time [68]. In particular, for nodular lesions with a rapid growth, the acronym EFG has been introduced, respecting better the clinical characteristics of such a melanoma: E for “Elevated,” F for “Firm,” and G for “Growing” (a compact nodule that grows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree