A thorough working knowledge of the diagnosis and treatment of life-threatening electrolyte abnormalities in cancer patients, especially hyponatremia, hypoglycemia, and hypercalcemia, is essential to the successful practice of emergency medicine. Although most minor abnormalities have no specific treatment, severe clinical manifestations of several notable electrolytes occur with significant frequency in the setting of malignancy. The treatment of life-threatening electrolyte abnormalities is reviewed here. Promising future treatments directed at the underlying physiology are also introduced.
Electrolyte abnormalities are perhaps the most common laboratory finding in patients with malignancies who present to the emergency department. Although most minor abnormalities have no specific treatment, severe clinical manifestations of several notable electrolytes occur with significant frequency in the setting of malignancy. If improperly treated, abnormalities of serum sodium, glucose, calcium, magnesium, and phosphorus may have serious consequences. A review of the most serious electrolyte abnormalities associated with malignancy follows.
Hyponatremia
Hyponatremia is a common electrolyte disorder, reported to occur in 3.8% of emergency department patients. Among the population of emergency department patients with underlying malignancy, hyponatremia occurs most commonly with small cell lung cancers. Hyponatremia has been reported with other malignancies, including primary and metastatic malignancies of the brain, pancreatic adenocarcinoma, and prostate cancer. Hyponatremia has also been reported in association with treatment with chemotherapeutic agents, particularly cisplatin and carboplatin. Regardless of the associated malignancy, hyponatremia can present as either an incidental finding or with life-threatening severity. Correction of hyponatremia requires an understanding of both the rapidity with which the hyponatremia has developed as well as the potential complications of treatment.
Pathophysiology
Syndrome of inappropriate antidiuretic hormone
Hyponatremia associated with malignancy is most commonly caused by the syndrome of inappropriate antidiuretic hormone (SIADH) secretion. Ectopic secretion of arginine vasopressin (AVP) by tumor cells appears to play a significant role in the development of hyponatremia. Small cell lung cancer is particularly notorious for elevated levels of circulating AVP despite serum hypotonicity. Other hormones have been implicated in the pathogenesis of hyponatremia of malignancy, including atrial natriuretic peptide, but their ultimate contribution to hyponatremia remains somewhat unclear.
Elevated levels of AVP in patients with malignancy cause hyponatremia primarily due to inappropriate retention of free water at the collecting-duct level despite relative serum hypotonicity. Normally in the setting of hypotonicity, the secretion of AVP is suppressed. In malignancy, the release of AVP by tumor cells does not respond to changes in serum tonicity, and, as a result, AVP remains present in the circulation and results in cyclic AMP-mediated insertion of water channels in the collecting ducts (aquaporin 2). The absorption of free water at the collecting-duct level results in worsening hypotonicity and inappropriately concentrated urine. Clinically, the result is hyponatremia in an apparently euvolemic patient.
Renal salt wasting
Hyponatremia of malignancy has also been reported as a complication of chemotherapy. Both cisplatin and carboplatin have been reported to cause hyponatremia. The mechanism for hyponatremia associated with chemotherapeutic drugs is believed to be renal salt wasting syndrome (RSWS). In this disease process, damage to the renal tubules with subsequent inability to retain sodium is thought to result in increased sodium loss. Clinically, the patient will appear hyponatremic with euvolemia; however, the treatment of RSWS is sodium supplementation rather than water restriction. An elevated spot urine sodium level may suggest RSWS. In SIADH, urinary excretion of sodium is usually normal or decreased. Definitive diagnosis of RSWS, however, can only be made after measurement of daily sodium intake and excretion. RSWS is diagnosed when daily sodium intake is less than urinary excretion. In extremis, however, treatment of hyponatremia due to RSWS is identical to the treatment of hyponatremia due to SIADH.
Clinical Manifestations
The clinical presentation of hyponatremia is largely related to the acuity with which the sodium has declined and has less direct correlation with the actual measured sodium. Levels of decline greater than 0.5 mEq/L/h appear to be more likely to result in serious sequelae, but considerable variation exists between individuals. Most symptomatic individuals will have serum sodium less than 120 mEq/L; however, symptoms have been reported with sodium levels of 129 mEq/L or less.
The brain appears to be the organ most sensitive to changes in the serum sodium level. If the rate of sodium decline outstrips the adaptive capabilities of the brain, symptoms of hyponatremia develop. When the rate of sodium decline is slower, the brain will adapt by expelling potassium and other osmotically active substances (osmolytes) to maintain normal cell volume. These osmolytes include amino acids, myoinositol, creatine, and creatine phosphate. If, however, the rate of sodium decline exceeds the rate at which the brain can expel osmolytes, water shifts intracellularly down the osmotic gradient and results in cerebral edema.
In the setting of acute hyponatremia, the manifestations of the resultant cerebral edema may be severe and commonly include nausea, vomiting, headaches, seizures, coma, and respiratory arrest as the brain progressively swells. Increased intracranial pressure may eventually result in death due to herniation if hyponatremia is not treated.
If hyponatremia develops more slowly, the symptoms may be less severe but present nonetheless. In the patient with chronic hyponatremia, brain cells have had more time to expel osmolytes and maintain near-normal cell volumes. Patients with chronic hyponatremia appear to be at very low risk of life-threatening cerebral edema and present with more subtle symptoms of brain dysfunction. If the level of hyponatremia becomes severe (<120), seizures and altered mental status may still be present, and the sodium will require judicious correction.
In the emergency department, frequently, it will not be possible to determine the acuity of the hyponatremia. In the vast majority of out-of-hospital acquired cases of severe hyponatremia, the hyponatremia is chronic, and particular attention must be paid to the treatment of these patients, as they appear to be at much higher risk of treatment-related severe complications, particularly osmotic demyelination syndrome (ODS). Rapidly correcting the sodium of a patient with chronic hyponatremia and minimal symptoms can be disastrous, so the decision to aggressively treat the hyponatremia should be made with a careful assessment of the risks and benefits of therapy.
Osmotic demyelination syndrome
The most feared complication of the treatment of hyponatremia is the ODS, previously known as central pontine myelinolysis. ODS was first reported in 1959 as a consequence of the treatment of a severely hyponatremic alcoholic patient. Histologically, ODS is characterized by the destruction of oligodendrocytes and myelin in the central portion of the pons as well as the basal ganglia and cerebellum. The clinical presentation of patients who develop ODS as a consequence of treatment of hyponatremia includes quadriparesis or quadriplegia, pseudobulbar palsy, and altered mental status. In the worst cases, patients develop the “locked-in syndrome,” coma, and death days after treatment for hyponatremia.
The pathophysiology of ODS is complex but appears to be related to brain cell shrinkage and concentrated ion damage during rapid changes in serum tonicity. As described previously, the response to chronic hyponatremia is the release of organic osmolytes from neurons. This adaptive response is protective in the setting of longstanding hyponatremia. During acute correction, however, susceptible areas of the brain appear to be less able to reaccumulate these essential osmolytes. In humans, areas less able to react to osmotic stress appear to be the neurons of the central pons, basal ganglia, and areas of the cerebellum, resulting in the potentially devastating constellation of neurologic findings seen in ODS.
ODS appears to be related to both the severity and the chronicity of hyponatremia. Chronic severe hyponatremia presents the greatest risk for development of ODS with rapid correction of the serum sodium. Most cases of ODS have been reported in patients with chronic hyponatremia of less than 120 mEq/L. In the setting of malnutrition, however, ODS has been reported with higher serum sodium levels, a fact of significance in the treatment of hyponatremic cancer patients who are also at risk for malnutrition due to cachexia.
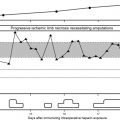
The development of ODS also appears to be directly related to the rate of rise of the serum sodium. Rates greater than 12 mEq/L/24 h are strongly associated with the development of ODS. Others have reported ODS occurring with rates of correction as low as 8 mEq/L/24 h, and the most recent consensus guidelines recommend limiting correction of the serum sodium to 8 mEq/L/24 h to avoid ODS.
Treatment
Rapidly correcting the sodium of a patient with chronic hyponatremia and minimal symptoms can be disastrous, so the decision to aggressively treat the hyponatremia should be made with a careful assessment of the risks and benefits of therapy. In the emergency department, patients with altered mental status, seizures, respiratory depression, or coma require emergent correction of hyponatremia. If symptoms are milder, the risk of rapid correction of hyponatremia causing ODS generally outweighs the benefits, and these patients should be treated with simple fluid restriction.
If the decision is made to correct hyponatremia emergently, the current treatment of choice is 3% saline infusion. Numerous formulas have been described for the calculation of free water excess, sodium deficit, and so on, but these formulas are cumbersome to use and not entirely reliable. A simpler approach is to infuse 1 cm 3 /kg body weight of 3% NS per hour, which will result in an increase of 1 mEq/L serum sodium per hour. Rates as high as 2 to 4 cm 3 /kg/h can be tolerated in the short term when symptoms require, but in any case, treatment should be halted once one of three end points is reached: resolution of symptoms, serum sodium of 120 mEq/L is reached, or the daily limit of 8 mEq/L correction is reached. Of course, hourly monitoring of the serum sodium is mandatory to prevent overcorrection.
In the event overcorrection does occur, relowering of the serum sodium through the infusion of D5W has the potential to reduce the risk of ODS and should be considered.
If the patient experiences seizures, standard antiepileptic treatment should be used in addition to correction of the hyponatremia with hypertonic saline. Patients at risk for volume overload or with a history of congestive heart failure may be given 20 to 40 mg of furosemide to enhance diuresis.
Disposition
Admission is warranted for any patient with significant symptoms due to hyponatremia. In the patient without symptoms, admission for fluid restriction and further evaluation is generally warranted if the serum sodium is at or less than 125 mEq/L, because symptoms most commonly develop below this level. In the intermediate range (126–130 mEq/L), disposition should be based on the availability of expeditious follow-up care.
Future Directions
A new class of medications, arginine vasopressin receptor (AVPR) antagonists (vaptans), has recently been approved for clinical use and holds significant promise for future treatment of hyponatremia. This is particularly true in cases of malignancy-associated SIADH, as the mechanism of action of these drugs would seem to be perfectly designed to counteract the effects of tumor-associated elevation of circulating AVP at the renal collecting-duct level. By interacting directly with the vasopressin receptor, AVPR antagonists cause an almost pure aquaresis by inhibiting the insertion of aquaporin 2 channels into the collecting duct and, thereby, result in a relative increase in serum sodium at the expense of free water diuresis.
Several studies have demonstrated the usefulness of AVPR antagonists in euvolemic and hypervolemic hyponatremia. The only AVPR antagonist currently approved for use is conivaptan, which has been approved for use in hospitalized patients with euvolemic hyponatremia due to SIADH, adrenal insufficiency, and hypothyroidism. Conivaptan is given as an intravenous (IV) bolus of 20 mg over 30 minutes and then by continuous infusion of 20 to 40 mg over the next 24 hours. Side effects due to conivaptan have reportedly been mild and most commonly include orthostatic dizziness, headache, and nausea. Apart from a higher level of orthostatic dizziness in the treated patients, other side effects are comparable to those with placebo.
The average increase in serum sodium in patients receiving vaptans in clinical trials has been 8 mEq/L, well within the safety range recommended for correction of hyponatremia to prevent ODS. Nine percent of patients had excessive rates of correction of sodium, but no cases of ODS have been reported thus far.
No clinical trials have specifically addressed the use of vaptans for the treatment of severely symptomatic hyponatremia, either alone or as an adjunct to the use of hypertonic saline. Therefore, the use of vaptans in the emergency department, although enticing, cannot be currently recommended for the treatment of symptomatic hyponatremia related to malignancy.
Osmotic demyelination syndrome
The most feared complication of the treatment of hyponatremia is the ODS, previously known as central pontine myelinolysis. ODS was first reported in 1959 as a consequence of the treatment of a severely hyponatremic alcoholic patient. Histologically, ODS is characterized by the destruction of oligodendrocytes and myelin in the central portion of the pons as well as the basal ganglia and cerebellum. The clinical presentation of patients who develop ODS as a consequence of treatment of hyponatremia includes quadriparesis or quadriplegia, pseudobulbar palsy, and altered mental status. In the worst cases, patients develop the “locked-in syndrome,” coma, and death days after treatment for hyponatremia.
The pathophysiology of ODS is complex but appears to be related to brain cell shrinkage and concentrated ion damage during rapid changes in serum tonicity. As described previously, the response to chronic hyponatremia is the release of organic osmolytes from neurons. This adaptive response is protective in the setting of longstanding hyponatremia. During acute correction, however, susceptible areas of the brain appear to be less able to reaccumulate these essential osmolytes. In humans, areas less able to react to osmotic stress appear to be the neurons of the central pons, basal ganglia, and areas of the cerebellum, resulting in the potentially devastating constellation of neurologic findings seen in ODS.
ODS appears to be related to both the severity and the chronicity of hyponatremia. Chronic severe hyponatremia presents the greatest risk for development of ODS with rapid correction of the serum sodium. Most cases of ODS have been reported in patients with chronic hyponatremia of less than 120 mEq/L. In the setting of malnutrition, however, ODS has been reported with higher serum sodium levels, a fact of significance in the treatment of hyponatremic cancer patients who are also at risk for malnutrition due to cachexia.
The development of ODS also appears to be directly related to the rate of rise of the serum sodium. Rates greater than 12 mEq/L/24 h are strongly associated with the development of ODS. Others have reported ODS occurring with rates of correction as low as 8 mEq/L/24 h, and the most recent consensus guidelines recommend limiting correction of the serum sodium to 8 mEq/L/24 h to avoid ODS.
Treatment
Rapidly correcting the sodium of a patient with chronic hyponatremia and minimal symptoms can be disastrous, so the decision to aggressively treat the hyponatremia should be made with a careful assessment of the risks and benefits of therapy. In the emergency department, patients with altered mental status, seizures, respiratory depression, or coma require emergent correction of hyponatremia. If symptoms are milder, the risk of rapid correction of hyponatremia causing ODS generally outweighs the benefits, and these patients should be treated with simple fluid restriction.
If the decision is made to correct hyponatremia emergently, the current treatment of choice is 3% saline infusion. Numerous formulas have been described for the calculation of free water excess, sodium deficit, and so on, but these formulas are cumbersome to use and not entirely reliable. A simpler approach is to infuse 1 cm 3 /kg body weight of 3% NS per hour, which will result in an increase of 1 mEq/L serum sodium per hour. Rates as high as 2 to 4 cm 3 /kg/h can be tolerated in the short term when symptoms require, but in any case, treatment should be halted once one of three end points is reached: resolution of symptoms, serum sodium of 120 mEq/L is reached, or the daily limit of 8 mEq/L correction is reached. Of course, hourly monitoring of the serum sodium is mandatory to prevent overcorrection.
In the event overcorrection does occur, relowering of the serum sodium through the infusion of D5W has the potential to reduce the risk of ODS and should be considered.
If the patient experiences seizures, standard antiepileptic treatment should be used in addition to correction of the hyponatremia with hypertonic saline. Patients at risk for volume overload or with a history of congestive heart failure may be given 20 to 40 mg of furosemide to enhance diuresis.
Disposition
Admission is warranted for any patient with significant symptoms due to hyponatremia. In the patient without symptoms, admission for fluid restriction and further evaluation is generally warranted if the serum sodium is at or less than 125 mEq/L, because symptoms most commonly develop below this level. In the intermediate range (126–130 mEq/L), disposition should be based on the availability of expeditious follow-up care.
Future Directions
A new class of medications, arginine vasopressin receptor (AVPR) antagonists (vaptans), has recently been approved for clinical use and holds significant promise for future treatment of hyponatremia. This is particularly true in cases of malignancy-associated SIADH, as the mechanism of action of these drugs would seem to be perfectly designed to counteract the effects of tumor-associated elevation of circulating AVP at the renal collecting-duct level. By interacting directly with the vasopressin receptor, AVPR antagonists cause an almost pure aquaresis by inhibiting the insertion of aquaporin 2 channels into the collecting duct and, thereby, result in a relative increase in serum sodium at the expense of free water diuresis.
Several studies have demonstrated the usefulness of AVPR antagonists in euvolemic and hypervolemic hyponatremia. The only AVPR antagonist currently approved for use is conivaptan, which has been approved for use in hospitalized patients with euvolemic hyponatremia due to SIADH, adrenal insufficiency, and hypothyroidism. Conivaptan is given as an intravenous (IV) bolus of 20 mg over 30 minutes and then by continuous infusion of 20 to 40 mg over the next 24 hours. Side effects due to conivaptan have reportedly been mild and most commonly include orthostatic dizziness, headache, and nausea. Apart from a higher level of orthostatic dizziness in the treated patients, other side effects are comparable to those with placebo.
The average increase in serum sodium in patients receiving vaptans in clinical trials has been 8 mEq/L, well within the safety range recommended for correction of hyponatremia to prevent ODS. Nine percent of patients had excessive rates of correction of sodium, but no cases of ODS have been reported thus far.
No clinical trials have specifically addressed the use of vaptans for the treatment of severely symptomatic hyponatremia, either alone or as an adjunct to the use of hypertonic saline. Therefore, the use of vaptans in the emergency department, although enticing, cannot be currently recommended for the treatment of symptomatic hyponatremia related to malignancy.
Hypoglycemia of malignancy
Tumor-associated hypoglycemia is a relatively rare complication of malignancy. Hypoglycemia of malignancy has been described in association with 3 main etiologies. The most common cause is nonislet cell tumor hypoglycemia (NICTH). Second, but perhaps more well known, is hypoglycemia due to insulin secretion by islet cell tumors of the pancreas. Finally, end-stage metastatic carcinoma of nearly any source that has heavily infiltrated the liver or adrenal glands may cause hypoglycemia. In the emergency department, the diagnosis and treatment of tumor-associated hypoglycemia requires careful evaluation for other possible causes of hypoglycemia. When other causes have been excluded, treatment of tumor-associated hypoglycemia may be curative or palliative.
Pathophysiology
Perhaps the most well known cause of tumor-associated hypoglycemia is the insulinoma of the pancreas. Insulinoma is a well-known but relatively rare tumor, occurring with an incidence of 1 to 4 per million people. About 90% of insulinomas are benign, and surgical treatment is curative. Insulinomas almost exclusively occur in the pancreas and represent deregulated production of insulin by beta cell tumors.
In the case of NICTH, hypoglycemia is associated with a variety of tumors, including those of mesenchymal, epithelial, and hematopoietic origin. The most common tumors among these tend to be fibrosarcomas, mesotheliomas, leiomyosarcomas, hepatomas, lung cancers, as well as gastric and pancreatic exocrine tumors. NICTH appears to be caused by the secretion of insulin-like growth factor II, a circulating hormone normally synthesized in the liver, which is capable of activating insulin receptors and resulting in hypoglycemia.
In the final instance, that of metastatic malignancy infiltrating the liver or adrenal glands, hypoglycemia is thought to occur either due to simple tissue destruction or due to as yet not fully identified secondary mechanisms, including secretion of tumor necrosis factor alpha, interleukins 1 and 6, or other mechanisms. Research in animals tends to favor the latter explanation, as all of these compounds have been shown to cause profound hypoglycemia.
Clinical Manifestations
Tumor-associated hypoglycemia presents no differently from hypoglycemia due to other mechanisms and should be suspected in any cancer patient with altered level of consciousness, obtundation, or bizarre behavior.
Given the rarity of this disorder, however, a dedicated search for other causes of hypoglycemia should be undertaken before ascribing the symptoms and glucose level to tumor origin. If the patient is diabetic, effort must be taken to evaluate oral intake as well as medication regimen. A complete evaluation for infection or other organ dysfunction may also be warranted, because sepsis, renal failure, and liver failure are all well known, and more common, causes of hypoglycemia in the acutely ill emergency department patient. In the absence of diabetes, infection, or organ dysfunction, evaluation for surreptitious use of insulin or other hypoglycemic agents should also be undertaken, because that is likely the most common cause of hypoglycemia in nondiabetics.
When the patient is not known to have cancer, the diagnosis of tumor-associated hypoglycemia may be particularly difficult. Patients who are ultimately diagnosed with tumor-associated hypoglycemia have frequently suffered from long-standing bouts of recurrent fasting hypoglycemia without an identifiable cause. Admission for further evaluation of any patient with recurrent hypoglycemia with no identifiable cause is warranted, as evaluation of insulin, C-peptide and insulin-like growth factor I and II levels may be very helpful in elucidating the cause and expediting the further workup of suspected tumor-associated hypoglycemia.
Treatment
Once hypoglycemia has been identified, the initial treatment is with glucose and glucose-containing solutions via standard regimens, followed by feeding once consciousness is normalized.
After the acute episode, treatment is directed at either curative or palliative measures. In the case of insulinomas and nonmetastatic tumors causing NICTH, surgical excision may be curative. If operative treatment is not possible due to coexisting disease, invasive disease, and/or metastatic disease, treatment in concert with an endocrinologist may provide relief from symptomatic hypoglycemia. Depending on the tumor, regimens composed of prednisone with or without somatostatin analogs appear to be effective in eliminating the occurrence of symptomatic hypoglycemia.
Disposition
As discussed above, admission is warranted for any patient with hypoglycemia that is recurrent or for which no readily reversible cause can be found (eg, diabetic who has skipped a meal). This is particularly true of those in whom a diagnosis of tumor-associated hypoglycemia has not been made as expedited workup and surgical treatment may be curative.
In the case of a patient with known insulinoma, NICTH, or metastatic malignancy, the ultimate disposition decision should be made in concert with the patient, the patient’s oncologist, and likely in consultation with an endocrinologist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree