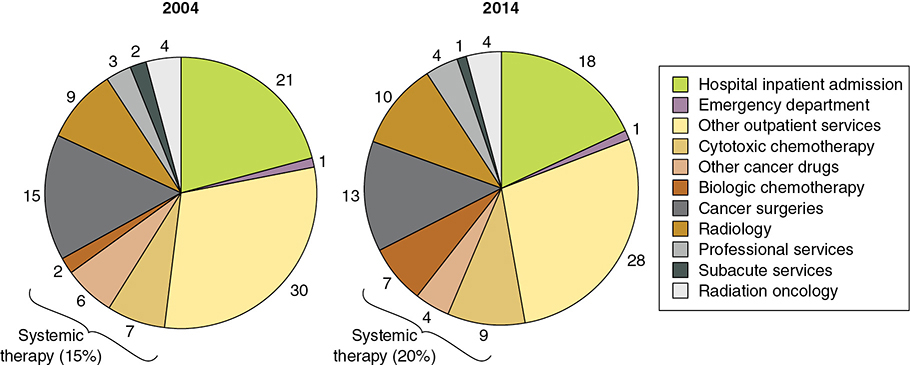
Kathy was diagnosed with advanced adenocarcinoma of the left upper lobe metastatic to the bones in January 2016. Within 5 weeks ofer diagnosis, she had low-dose lung computed tomography (CT), a second chest CT scan to confirm the findings, pulmonary function tests, a lung needle biopsy, a positron emission tomography (PET)/CT scan, several blood tests, and next-generation sequencing searching for actionable genetic alterations and was seen by a medical oncologist. Kathy was deemed not a candidate for targeted therapy or immunotherapy up front and began chemotherapy in March 2016. Response to chemotherapy was evaluated with serial CT scans. In May, Kathy was found to have progression of her disease during an emergency room visit and started second-line immunotherapy in June at her doctor’s office. The immunotherapy resulted in stable disease and maintained her quality of life, so Kathy continued the treatment and monitoring through the end of the year. Kathy bought an individual health insurance plan, which started in January 2016, through her state’s marketplace. The premium for her plan was $537 per month, but she qualified for tax credits, which helped reduce these costs. Kathy ended up paying $272 per month in premiums. Kathy’s highest costs were in January ($3,678) and February ($3,716), when she had multiple diagnostic tests and paid 40% percent co-insurance for imaging tests and scans, in addition to premiums. She met her maximum out-of-pocket limit in February; after that, no cost sharing was required as long as she paid her premiums and received all her care in network. At the end of her plan year, Kathy had paid a total of $3,264 in premiums and $6,850 in cost sharing for her cancer care. The total health care costs for Kathy’s lung cancer treatment in 2016 were $210,067. Kathy’s insurance plan paid the vast majority of these costs—$203,217. (Adapted from an American Cancer Society Cancer Action Network Report: Singleterry J. The Cost of Cancer: Addressing Patient Costs.1) Learning Objectives: 1. What are the financial consequences of the improvement in therapies and lung cancer outcomes? 2. What are the factors driving the rising cost of lung cancer care? 3. What is the impact of rising costs on patients and society? 4. What are the instruments and strategies used to evaluate the value of any given lung cancer therapy? 5. What are the current efforts to address these rising costs of lung cancer care? Lung cancer is the leading cause of cancer-related mortality worldwide.2,3 The development of new therapies for lung cancer (targeted therapies and immunotherapy), along with an increase in prevention efforts, has resulted in a reduction in the incidence and mortality of lung cancer in some populations (eg, men in Northern Europe and North America). In other groups, however, the incidence and mortality in women have reportedly increased (women in a large part of Europe, South America, and Asia).4,5 The increase in clinical effectiveness from these new therapies has been accompanied by an increase in the economic burden of cancer care, which in turn could limit patient access to these therapies. Inadequate access to cancer care could have a substantially negative impact on cancer outcomes for those affected individuals.6,7 Given the increase in the cost of lung cancer care, the challenge for health care providers and health systems is to deliver high-quality cancer care while utilizing the limited economic resources efficiently. It has been estimated that in 2017, the United States spent $13.9 billion on lung cancer care, a significant increase from 2010 ($12.1 billion) and 2013 ($12.9 billion).8 Any discussion regarding the economic impact of lung cancer care must consider the total cost of care (the cost paid by health insurance companies/managed care organizations, employers, patients, and taxpayer-funded programs such as Medicare). Unfortunately, the information available regarding cancer care expenditure and total cost of cancer care is scarce. For instance, the number of articles available in PubMed related to health care expenditure, total cost of care, cost effectiveness, cost analysis, and economics of lung cancer care represent a small fraction (0.74%) of the total number of published lung cancer articles.9 Furthermore, given the variability among health systems, regulatory agencies, and economic models among countries, attempting a discussion of the economics of lung cancer that would apply to all settings around the globe seems unrealistic. This discussion uses the US society and health system as a framework. The total cost of cancer care has different components.10 Direct costs include inpatient care (hospital admissions), emergency room visits, ambulatory care (doctor’s visits), radiation, chemotherapy infusions, radiology, and more. These are the most readily measurable. Indirect costs include lost income, child care, mental services, transportation, caregiving costs, and so on. Intangible costs are related to pain, suffering, and grief. All these components of the total cost of care are influenced by multiple factors, such as type of insurance (directly linked to patient out-of-pocket expenses), geographic location, affiliation of health care provided, type of cancer, and more.3 There is limited information available regarding the fraction of the total cost that each of these components represents. In the United States, a large-scale survey of individuals, medical providers, and employers conducted yearly since 1996 by the US Department of Health and Human Services has estimated the health care use and expenditure for treating cancer among the US adult civilian population.11 These estimates have shown variation on the percentage of the cost for each component reported throughout the years (Figure 5-1).11,12 Similar efforts from private entities have also shown variation in the distribution of the health expenditures on cancer care throughout time. For instance, an analysis of claims from a large database containing clinical and health expenditure data from Medicare, Medicaid, and privately insured patients13 and a sample of 5% of Medicare patients found that health care expenditures for actively treated cancer patients varied between 2004 and 2014, as shown in Figure 5-2.14 Both sources suggested a greater relative increase in the expenditure on ambulatory services and cancer-directed therapy compared to the other components of the total cost. Figure 5-1. Percentage distribution of expenditure for cancer treatment, by type of service. (Agency for Health Care Research and Quality Total expenses and percent distribution selected conditions by source of payment: United States, 2014. Medical Expenditure Panel Survey Household Component Data. 2014. https://meps.ahrq.gov/mepsweb/data_stats/quick_tables_results.jsp?Action=Search&SearchMethod=1&component=1&subcomponent=0&tableSeries=2&year=-1). Figure 5-2. Expenditures by type of treatment. (Adapted from Finch KM, Pelizzari PM, Pyenson B. Cost drivers of cancer care: a retrospective analysis of Medicare and commercially insured population claim data 2004-2014. 2016, April 14. https://www.milliman.com/en/insight/cost-drivers-of-cancer-care-a-retrospective-analysis-of-medicare-and-commercially-insured.) The total expenditure on cancer care for a single person varies through the course of the disease and is dependent on multiple factors (age at diagnosis, insurance status, insurance carrier, stage at diagnosis, comorbidities).15 The average spending per patient increases just prior to diagnosis and spikes immediately following diagnosis.15 The average annualized net costs of cancer care are highest in the last year of life, approximately 30% of the total cost.8 The total expenditure also varies according to the specific cancer diagnosis. A study of the cost to breast, colon, and lung cancer patients and their health plans based on claims from a large database found that spending per patient increased from under $1,000 per month until 2 to 3 months prior to diagnosis, to as high as $25,000 in the period of 2011 to 2014 during the month of diagnosis.16 In this report, lung cancer was found to have the highest per month spending levels postdiagnosis and throughout the disease course. These findings need to be considered in the context of the subsequent Food and Drug Administration (FDA) approval of immunotherapy drugs for lung cancer, the first of which occurred after the period reported in this study (March 2015).17 Immunotherapy agents are expected to be a significant component of expenditures of lung cancer care due to their costs.18 Moreover, variations in the cost of cancer care across US regions without consistent differences in survival outcomes have been reported. A landmark study showed that high-cost regions had 30% to 40% more inpatient hospitalizations, 70% to 120% more intensive care unit days, and 12% less hospice use without a difference in outcomes compared to lower cost regions.19 The increased health care expenditure on cancer care can have negative consequences in patients and in the society as a whole20: • The abandonment rate (patient-directed discontinuation) of oral cancer therapy drug has been reported to be around 10% in a nationally representative pharmacy claims database. Higher cost sharing (higher out-of-pocket expenses) and lower income resulted in significantly higher rates of abandonment.21 • Recipients of low-income subsidies (financial aid) for patients with Medicare Part D coverage have shown higher adherence to oral cancer therapy compared to those patients who did not qualify for the subsidies, despite the former being of a lower socioeconomic status than the latter.22 • In a large claims database analysis, increasing out-of-pockets expenses were associated with decreasing adherence to erlotinib therapy in patient with non–small cell lung cancer (NSCLC) receiving this medication.23 In a Medicare population sample, it was estimated that an increase of $10 in out-of-pocket expenses per month would result in a 14% increase in the likelihood of discontinuation or delay of therapy with erlotinib in patients with NSCLC receiving this medication.24 • A diagnosis of cancer has been associated with a 2.65 times increased risk of bankruptcy.25 It has been suggested that bankruptcy can in turn have adverse health-related consequences, such as increased mortality, for bankrupted patients compared to those cancer patients who do not file for bankruptcy.26 • The lost earnings due to cancer death in the United States were estimated to amount to $94.4 billion in 2015, with the highest loss being in the southern and midwestern states.27 Most of the information available and the current discussion on cost of lung cancer care is centered on cancer drug pricing. The likely reasons are multiple. There is a reported increase in the percentage of outpatient cost as a fraction of the total health care expenditures.11,14 Managed care organizations (private insurance payers) in the United States have recently reported that drug and drug administration represent 26% of the total health care expenditures. They also reported an average of 12% increase in pharmacy benefit cancer drug spending and between 2016 and 2017 an average of 14% increase in medical benefit cancer drug spending.28 These findings have likely shaped the perception of the most pressing issues for key stakeholders in cancer care. For instance, when managed care organizations, specialty pharmacies, oncologists, oncology practice managers, and employers in the United States were presented with 14 cancer care issues and asked to rank the top 5 in a large survey, control of cancer specialty drug costs was consistently selected as one of the 3 most pressing 2016 challenges facing cancer care.29 There are several factors that are implicated in the acceleration of these rising costs7: • Increase in the rate of introduction of new and expensive FDA-approved drugs • Slower pace of conversion to generics/biosimilar items and the parallel increase in cost of these generic drugs • The introduction of expensive drugs for conditions that affect large segments of the population, as opposed to rare conditions as in the past The last is particularly relevant for lung cancer, for which the current standard treatment for metastatic NSCLC,30,31 locally advanced NSCLC,32 and extensive-stage small cell lung cancer33 now includes immunotherapy in the treatment backbone. Together, these groups represent approximately 65% of all the newly diagnosed cases,34 which in 2018 was estimated at 234,030 cases.35 There are other factors driving escalating costs that are intrinsically related to the complexity of the pharmaceutical market. This is particularly true for the US market, in which the flow of pharmaceutical products from manufacturers to patients evolved separately from the financing mechanisms for those products.36 Understanding the distribution of drugs and the financing systems provides a vehicle for understanding the complexity of the rise in the cost of cancer therapies (Figure 5-3). Figure 5-3. Conceptual model of connections between pharmaceuticals, services, costs, and payments. Rx, prescription; Pharmacy, all types of pharmacies, including hospital and mail-order. (Adapted from Congressional Budget Office (CBO). Prescription drug pricing in the private sector. https://www.cbo.gov/publication/18275. January 2007). Cancer drugs in the United States are delivered from manufacturers to patients through intermediaries: Drug distributors purchase them from manufacturers and then ship them to retailers, where patients obtain their drugs. Financing of the drugs is done through payers, whether public (Medicare) or private (private health insurance carriers, out-of-pocket expenses), as well as through pharmacy benefit managers (PBMs). The vast majority of private health insurance is obtained through employer-based insurance, with most insurances offering drug benefits programs. Many of these payers outsource the management of their drug benefits to PBMs.36 The factors attributed to the rising costs in lung cancer care that are related to the pharmaceutical market are abundant. It is beyond the scope of this synopsis to provide a detailed and comprehensive discussion of these factors. The following factors are widely perceived as some of the main drivers of the rising costs: • In the United States, drug manufacturers are allowed to set the price of their products. In most developed nations with national health systems, drug prices are negotiated or even rejected based on the analysis of its benefit in relation to its cost.37 In the United Kingdom, for instance, evaluation of a new drug requires that the drug pass a cost-utility threshold (usually between £20,000 and £30,000, or $25,000 and $40,000 per quality-adjusted life-year [QALY]) gained before it is recommended for coverage at a national level.38 • It has been estimated that drug prices decline to approximately 52% of brand-name drug prices with two generic manufacturers making the product, 33% with five manufacturers, and 21% with eight manufacturers.39 However, the process of entry of generic drugs to the market has been deemed excessively slow and plagued with multiple hurdles.40 • Market exclusivity of a drug (protection from competition) is granted by the US government through two mechanisms: initial FDA approval (5-7 years for new small molecules41 and 12 years for new biologics
5
ECONOMICS OF LUNG CANCER
COST OF LUNG CANCER THERAPIES
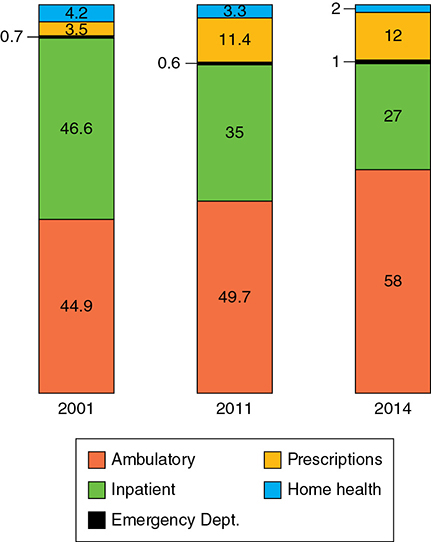
Impact on Patient and Society
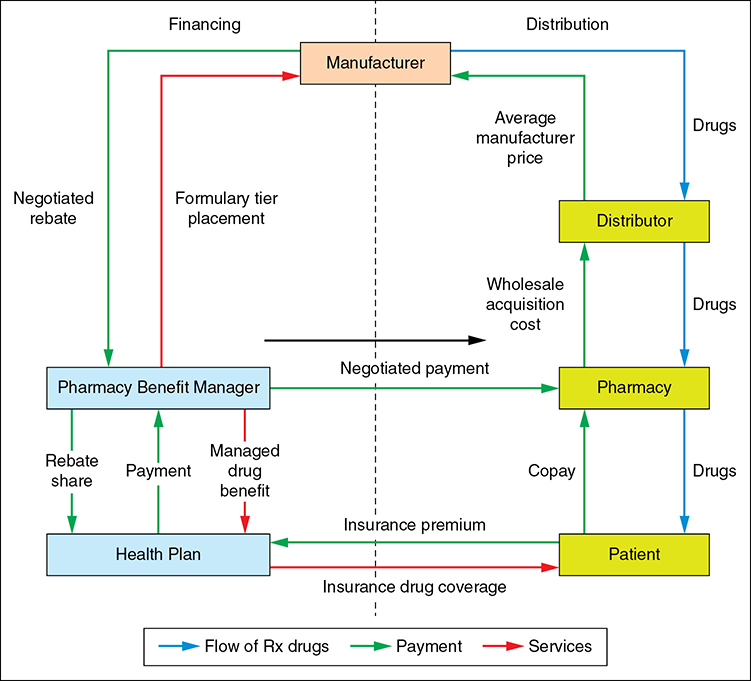
Causes of Rising Cancer Costs
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree