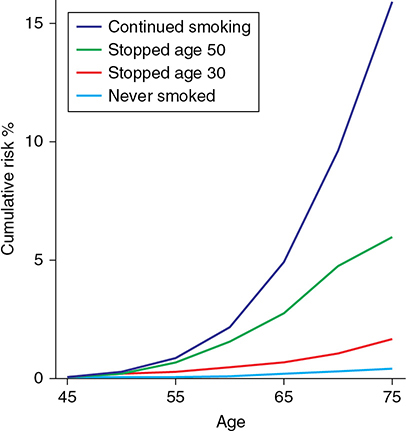
A 40-year-old African American male with a past medical history of hypertension and myocardial infarction and a 15 pack-year tobacco history presents for a routine health management visit. He has two first-degree relatives with non–small cell lung cancer. He is asymptomatic and has quit smoking, but he requests information on any chemopreventive measures he could utilize to avoid the development of lung cancer. What chemoprevention strategies should be offered to this patient? Learning Objectives: 1. What are the lifestyle modifications that reduce lung cancer risk? 2. What are the preventable causes of lung cancer? 3. What are the historical chemoprevention strategies that have been utilized in thoracic malignancies? 4. What strategies have improved the prevention of lung cancer? 5. What are the future standards for chemoprevention in thoracic malignancies? Effective cancer prevention strategies are aimed at reducing the incidence and mortality of that cancer. Primary prevention such as smoking cessation and early screening are covered in other chapters, while lifestyle modification is reviewed here, as well as strategies utilized in both the primary and secondary settings to prevent thoracic cancer. Primary prevention involves interventions in genetic, environmental, biologic, and physical factors that cause cancer. Secondary prevention incorporates strategies to detect cancers in asymptomatic carriers so the treatment can be introduced more promptly. Tertiary prevention refers to prevention of cancers in disease survivors, such as tobacco cessation in lung cancer survivors. Chemoprevention is the use of natural or synthetic compounds to prevent carcinogenesis and the development of cancer. The single most important lifestyle modification for the reduction of lung cancer risk is cessation of smoking. Tobacco carcinogenesis and treatment are presented in Chapter 3. All histologic subtypes of lung cancer are caused by cigarette smoking, and cigarettes and tobacco users can benefit at any time by quitting smoking. While lung cancer risk decreases the longer someone is abstinent from smoking, even at greater than 40 years, the risk of former tobacco smokers fails to return to the risk of never-smokers.1,2 In fact, continued smoking to older age is associated with an exponential increase in the risk of lung cancer compared to people who stop prior to 50. The cumulative risk of death from lung cancer in males who smoke to age 75 is 16%, compared to those who stop by age 50 (6%), and it is even lower if smoking stops by age 30 (2%). This lends credence to targeting youth for smoking cessation and never smoking campaigns by public health officials (Figure 9-1). Figure 9-1. Smoking cessation and lifetime risk of lung cancer. (Reproduced with permission from Vineis P, Alavanja M, Buffler P, et al. Tobacco and cancer: recent epidemiological evidence. J Natl Cancer Inst. 2004;96(2):99-106. ePub 2004/01/22. Copyright © Oxford University Press.) Secondhand smoke exposure has been recognized for over 20 years as a cause of lung cancer among non-smokers. In particular, non-smokers who live with a smoker have up to a 30% increased risk of lung cancer.4 Children are at highest risk in this scenario because of the developmental effects of tobacco smoke on lung tissue and their smaller lung size per dose of smoke. Local laws to create smoke-free environments have reduced the risk of secondhand smoke exposure in occupations such as the hotel, restaurant, and entertainment industries.5,6 From a global health perspective, adoption of smoke-free laws is one of the best lifestyle modifications that a community can do to improve the health of its citizens. Diets high in fruits and vegetables have been extensively evaluated as cancer risk reducers, and in 2007, the World Cancer Research Fund (WCRF) recognized a level of evidence of “probable” benefit for fruit consumption and decreased lung cancer risk, with lesser evidence that vegetable consumption is beneficial.7 Because fruits and vegetables are a major source of antioxidant micronutrients and theoretically can provide detoxification of carcinogens, extensive research has been undertaken concerning the protective effect of antioxidants such as carotenoids in lung cancer. To date, no antioxidant studies have shown a positive benefit in the prevention of lung cancer. It is well recognized that lifestyle changes to increase aerobic exercise are protective against the development of cancer, as well as improving health during cancer therapy. Data suggest a 13%-30% decrease in lung cancer risk with moderate-to-high levels of physical activity.8 Clearly, aerobic exercise should be recommended for all people, including those with current or past lung cancer diagnosis. Conversely, a low body mass index (BMI) increases the risk of lung cancer, but this may be related to other lifestyle choices and comorbidities—smoking, alcohol intake, and poor physical fitness—which lead to low BMI. In general, it is accepted to recommend increased physical activity to all cancer patients. As stated, the primary risk factor for development of lung cancer is smoking; however, other health conditions also increase lung cancer risk. Persons with chronic obstructive pulmonary disease (COPD) have a 2- to 4-fold higher incidence of lung cancer than those who do not have COPD, when controlling for cigarette smoke.9 Pulmonary fibrosis is also a risk factor for lung cancer. Aside from smoking, radon exposure and asbestos exposure and other less common risk factors for lung cancer include mediastinal or chest wall irradiation (most commonly seen in Hodgkin’s lymphoma and breast cancers) and occupational carcinogen exposure (eg, to chromium, arsenic, uranium, nitrogen mustard gas, nickel dust, and polycyclic aromatic hydrocarbons). Persons with COPD and pulmonary fibrosis have higher rates of lung cancer, whether mechanistically related to similar underlying pathophysiology or due to common exposures (tobacco smoke, polycyclic aromatic hydrocarbons, occupational exposure). In fact, persons with chronic obstructive pulmonary disease (COPD) (GOLD class III or IV) have a significantly higher rate of lung cancer development than those without COPD, when controlling for tobacco smoke exposure.9,10 Part of the risk attributed to airflow obstruction appears to be derived from the presence of radiographic emphysema, which is an important independent risk factor for lung cancer in smokers and never-smokers.9 Idiopathic pulmonary fibrosis (IPF) also carries a higher risk of lung cancer, ranging from 4.4% to 48%,11 and is higher in males and people of older age, with a smoking history, and associated emphysema. Squamous cell carcinoma is the most frequent histology, and IPF is correlated with shorter survival compared to those without IPF.11,12 Connective tissue disease–associated interstitial lung disease (CTD-ILD) is also a risk factor for lung cancer, where approximately 9% of patients develop lung cancer, especially those who have associated emphysema.10 Computed tomographic (CT) screening of these high-risk groups is becoming more accepted, regardless of smoking history. Aggressive treatment of underlying causes of emphysema and pulmonary fibrosis may help abrogate risk. Mediastinal, breast13,14 and chest wall radiation treatments for other malignancies, such as Hodgkin disease,14 increase the risk of lung cancer. Modern radiation techniques attempt to avoid exposing normal lung tissue to ionizing radiation, but small areas of lung remain in the radiation field in some cases. Scrupulous physics planning and normal tissue protection are critical for radiation of the lung. Lung cancers often develop in the periphery of the lung in these cancer survivors and can occur many years after radiation exposure. While survival is similar to non–radiation-induced lung cancers, smoking cessation is important for primary prevention, and CT screening can help diagnose these cancers earlier. Studies of individuals with HIV infection have observed higher rates of lung cancer, albeit almost exclusively in smoking populations, which confounds confirmation of the true risk of HIV infection and pulmonary malignancies. It is generally accepted that HIV adds a relative risk between 2.5 and 3.5 to other risk factors such as smoking.15,16 As antiretroviral therapy successfully extends life in people with HIV, lung cancer risk, which increases with age, is expected to increase in the HIV-positive population. Lung cancer is now the third most frequent malignancy associated with HIV, highlighting its global importance in this vulnerable population and the need for rigorous CT screening in smokers with HIV. Additionally, aggressive antiretroviral therapy and maintenance of undetectable viral load has potential benefit in cancer prevention, although this has not been confirmed in controlled trials. Excessive alcohol abuse has been associated with many forms of cancer, and the American Society of Clinical Oncology (ASCO) recommends limiting alcohol intake to reduce overall cancer risk17; however, lung cancer risk reduction related to alcohol is less well understood. While heavy alcohol drinking has been statistically associated with increased lung cancer risk,18 a study of alcohol consumption in never-smokers was not linked to increased risk,19 raising the question of tobacco smoke confounding the finding in smokers.16,17 Marijuana use has not been proven to be associated with an increase in lung cancer rates because of limited studies and the difficulty of the coadministration of tobacco in most subjects who used daily marijuana.20 With the widespread legalization of medicinal and recreational marijuana and its expected increased use, it is anticipated that the risk of lung cancer from marijuana exposure will increase. Additionally, a different pattern of lung cancer (histologic and mutational) may emerge. Drugs of abuse, such as cocaine, heroin, and narcotics, have been associated with lung cancer, but less definitively than tobacco. Epidemiologic studies of familial aggregation of lung cancer have suggested a genetic susceptibility in some families. Germline polymorphisms in genes such as cytochrome p450 1A1 and glutathione S transferases Mu-1 and Theta-1, which detoxify tobacco-based carcinogens, have been proposed as possible additive risk factors for lung cancer development in smokers. However, the data are conflicting and not generalizable at the present time. Thus, germline screening cannot identify subjects for increased surveillance or aggressive prevention measures currently. While next-generation sequencing studies have identified multiple potential therapeutic targets for treatment of lung cancer, no common early mutations or germline defects have been discovered that could be applied to chemoprevention. Additionally, there is currently no accepted germline screening for lung cancer, outside of known familial cancer syndromes such as Li Fraumeni, Peutz-Jeager syndrome, and Lynch syndrome. Thus, smoking cessation remains the mainstay of prevention for lung cancer, and chemoprevention for lung cancer is still considered experimental. Occupational and environmental toxins have been associated with the development of multiple types of cancer, and lung cancer is the most common cancer associated with occupational exposures. Low–to-moderate levels of many trace elements, including arsenic, cadmium, chromium, and nickel, have been associated with increased incidence of lung cancer in the United States and in developing countries. Well-recognized occupations with higher rates of lung cancer include those that expose the lung to tar and soot (coke oven workers); trace elements or heavy metals such as arsenic, chromium, and nickel (mining); and radiation associated with uranium and radon (mining). Additionally, epidemiologists have identified carcinogens that case a higher rate of lung cancer in populations with groundwater exposure, air particulate exposure, and ingestion of toxic substances. Occupational Safety and Health Administration (OSHA) standards provide excellent primary prevention strategies for occupation-related risk reduction for lung cancer. Radon is a naturally occurring, chemically inert gas that develops as a decay product of uranium 238 and radium 226. Radon exposure occurs in occupations such as uranium mining and other underground mining (uranium miners)21 and in homes via soil and groundwater accumulation. It is thought that between 2% and 10% of lung cancers may be caused by exposure to residential radon. Additionally, the risk of lung cancer in underground miners increases to up to 10 times that of non-smoking miners. The United States Environmental Protection Agency recognizes greater than or equal to 4.0 pCi/L as a level at which corrective measures to reduce radon exposure should be taken; however, no minimum level of radon has been clearly established as safe. The relationship appears to be linear,22 with the alpha particles of radon thought to damage respiratory epithelium and work alone or synergistically with cigarette smoke.23 Radon testing in the home is recommended as radon remediation represents an important primary prevention of lung cancer. Asbestos exposure is directly linked to lung cancer development in multiple industries, including construction, shipping, and others. Asbestos fibers are found in the pulmonary parenchyma of lung cancer patients and may contribute to lung cancer development directly or indirectly through stimulation of inflammation.24 Asbestos and smoking act synergistically to increase lung cancer risk.25 Patients with longer exposure times or with associated pulmonary fibrosis are at higher risk of developing lung cancer.24,26 While the risk of lung cancer is dose dependent, workers exposed to amphibole fibers have a higher risk than those exposed to chrysotile fibers.26 Prevention of inhalation has been largely effective in reducing fiber exposure, but mesothelioma still occurs despite prevention efforts in the workplace. Many other occupational exposures have been associated with lung cancer. These include exposures to bis-chloromethyl ether, chromium, formaldehyde, ionizing radiation, nickel, polycyclic aromatic hydrocarbons, hard metal dust, and vinyl chloride. As risk reduction strategies in the workplace have changed, some of these exposures have been successfully abrogated. For example, improvement in industrial processes that have eliminated or reduced exposures to chloromethyl ethers and nickel compounds has reduced the risk of lung cancer in some occupations.27 However, this is not true globally, and continued efforts are needed to decrease occupational exposures worldwide. Given that many of these occupational exposures are synergistic with tobacco smoking, for many workers, the work site may be an important area for intervention in smoking cessation, which still remains the most common cause of lung cancer. Protections for industrial health workers not only should take into account exposure from elemental risks, but also should assess smoking and other airborne health risks when setting occupational exposure standards. Urban air pollution is caused by combustion of fossil fuels, leading to polycyclic aromatic hydrocarbons and metals released into the air as well as particulate matter such as sulfur dioxide and nitrogen dioxide. Air pollution can differ across countries, but has been associated with an increased risk of lung cancer of up to 40% in large urban areas of the United States,28 as well as other countries known for higher rates of air pollution.16,29 Additionally, occupational exposure to diesel and exhaust fumes is associated with a higher risk of lung cancer in smokers and non-smokers.30 Air pollution, including exposure to fine particulates, nitrogen dioxide, and ozone, are all linked to higher lung cancer rates. community and international efforts to reduce the causes of these environmental toxins are critical to the reduction in lung cancer risk in future generations. Indoor air pollution through coal burning,31 and other solid fuel burning for cooking, as well as indoor wood smoke exposure are associated with lung cancer, most commonly in developing countries. It is estimated that interventions to decrease solid fuel cooking and indoor air pollution exposure would significantly decrease lung cancer risk in these populations.16 In addition to tobacco smoke exposure, many other compounds and promoters of carcinogenesis are known to affect lung cancer patients. Chemoprevention uses vitamins, anti-inflammatory agents, hormonal antagonists, antioxidants, and differentiating agents to prevent cancer. Phase III randomized placebo-controlled clinical trials designed to confirm the utility of chemopreventive agents in lung cancer have not yielded positive results, despite excellent preclinical rationale. Several large phase 3 trials have examined the utility of chemopreventive agents in preventing the development of lung cancer. The Alpha-Tocopherol, Beta Carotene, Cancer Prevention Trial (ATBC) enrolled Finnish male smokers between the ages of 50 and 69 to receive alpha-tocopherol, beta-carotene, both, or placebo in a randomized 2 × 2 factorial design. Unfortunately, there was an increase in lung cancer incidence and mortality at 6 years in participants receiving beta-carotene. Additionally, there was no protective effect on lung cancer mortality in patients receiving both drugs or alpha-tocopherol alone. Similarly, the Beta-Carotene and Retinol Efficacy Trial (CARET) trial enrolled 17,000 smokers and workers in high-risk occupations related to asbestos. These participants were randomly assigned to receive beta-carotene, retinol, both, or placebo in a 2 × 2 factorial design. Again, an increase in lung cancer incidence (28%) and in lung cancer–related mortality (17%) were seen in those receiving beta-carotene and retinol or both drugs failed to protect against lung cancer development.
9
PREVENTION OF LUNG CANCER
LIFESTYLE MODIFICATION
Smoking
Secondhand Smoke
Physical Activity and Diet
HIGHER RISK HEALTH CONDITIONS
Chronic Lung Disease
Previous Radiation Therapy
HIV Infection
Alcohol, Marijuana, and Other Drugs of Abuse
Genetic Susceptibility
ENVIRONMENTAL AND OCCUPATIONAL EXPOSURES
Radon
Asbestos
Other Environmental Toxins
Air Pollution, Fossil Fuels, and Particulate Matter
CHEMOPREVENTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree