Dyslipidemia in the Elderly: Special Insights to Inform the Management Strategy
Michael H. Shannon
William R. Hazzard
The progressive and dramatic aging of the American population over the last century, accompanied and driven by continuing medical and public health advances, has shifted the burden of morbidity and mortality from cardiovascular disease (CVD) to increasingly higher ages. During this time the growth of the population 65 years old and over—collectively termed “the elderly” in this treatise but an extraordinarily heterogeneous group conveniently defined by their eligibility for Social Security and Medicare benefits—has exceeded by fourfold the growth of the population of the country as a whole. Persons 85 years old and over, sometimes referred to as the “oldest old,” are a still relatively small but rapidly growing subgroup of special relevance to the topic of this chapter. In 1994 they comprised 3.5 million persons, just over 1% of the American population. However, from 1960 to 1994 this group increased 274%, compared with an increase of 100% for all persons 65 years old and over and an increase of about 45% for the total population (1). The oldest old are thus projected to be the fastest growing segment of the population into the next century, including a growing number of centenarians among them.
THEORETICAL CONSIDERATIONS
Aging: Chronological versus Physiologic
There is no clear age boundary above which an individual becomes “elderly.” A person’s chronological age has limited utility in this definition, and instead the transition to “elderly” is better marked by functional and physiologic changes that are more common with aging. The storied baseball player Satchel Paige had pitched in the Negro League for many years before joining the Cleveland Indians after Jackie Robinson had broken the color barrier in the major leagues in 1947. Paige appeared with the Indians in the 1954 World Series. A man of colorful wit and much wisdom, when asked his age (rumored to be well into the 50s), he responded, “How old would you be if you didn’t know how old you are?” (for he truly did not know the year of his birth). His candid response illustrates the utility of functional and physiologic assessments as more useful prognostic and stratification indices than simple birth dates. An individual’s ability to perform activities of daily living, such as transferring from bed to chair or toilet and feeding, may be far more important to his or her prognosis and the intensiveness of desired interventions than his or her chronological age. By the same token, many persons younger than 65 years of age are quite dependent and live in more supportive environments such as extended care and assisted living facilities, while others over the age of 90 still live independently and are able to perform all of their functional tasks without assistance.
Aging: Frailty
The concept of “frailty,” marked by increasing vulnerability to stresses such as trauma, acute illness, pharmacologic misadventures, and environmental change, is important in the assessment of older individuals. Frailty is a defining geriatric syndrome in which advancing age is accompanied by symptoms and signs of weight loss, slowness, weakness, fatigue, decreased food intake and energy expenditure, and evidence of decreased muscle mass (sarcopenia) and bone loss (osteopenia), all interweaving to produce gait and balance abnormalities and increased risk of falls, fractures, infections, loss of functional independence, and a vicious circle that threatens not only the independence but also the very survival of the individuals affected. To illustrate the gravity of this condition, many studies have cited a greater 1-year mortality after a hip fracture than after an acute myocardial infarction (MI).
Aging: Physiologic Assessment
The changes in physiology with age are also unevenly distributed among individuals and among their organ systems even at a given age. Here the various markers of cardiovascular fitness, renal clearance, and hepatic metabolism become important tools for physiologic assessment. For example, an individual may be considered to be of advanced physiologic age when he or she manifests chronic renal insufficiency, worsening pulmonary function, or decreased maximal walking distances. The use of chronological age does not routinely incorporate other laboratory markers or clinical assessments such as creatinine clearance, maximal hand grip strength, or maximal forced expiratory volume, all of which may be better predictors of CVD and other outcomes than one’s birth date.
Aging: Chronological Age
The use of chronological age for assessing the status of a given patient thus clearly has its limitations. However, in the absence of a readily calculated and usable surrogate measure of physiologic aging (and for which over a half century of rigorous research has yet to find a simple formula), chronological age remains the standard, especially for administrative or public health purposes. Age 65 was chosen in the 19th century by the German leader Bismarck as the threshold for receipt of public funds in “retirement.” However, that was at a time when only 3% of the population lived beyond this age in his nation, and hence the projected burden upon those resources was small. Nevertheless, even as advances in public health and medical knowledge were allowing average longevity to grow dramatically in the United States, most dramatically in the first half of the 20th century, the same age 65 was also chosen as the threshold for receipt of Social Security payments in the United States beginning in the 1930s and for Medicare among the Great Society programs in the 1960s. This threshold has only recently begun to be marginally increased, even as the revolutionary, progressive rise in average longevity and the burgeoning of the population of baby boomers are dramatically changing the demographics of the nation and now threaten to overwhelm public resources in providing for their economic, social, and health care needs in retirement in the 21st century.
CVD in the Elderly
Thus of particular interest in the present volume on dyslipidemia is the reality that the vast majority of morbidity and mortality in individuals over the age of 65 occurs from CVD. In the United States, more than 80% of persons dying from CVD are over the age of 65, and more than 60% of death from CVD occurs in individuals over the age of 75. Despite progress in primary prevention of CVD and cardiac interventions, CVD remains the leading cause of death in both men and women over the age of 65, as it has been throughout the last century in the United States. CVD, especially in the form of ischemic strokes, is the most important cause of disability in the elderly as well. In the Framingham Study, among ischemic stroke survivors who were ≥65 years old, assessment at 6 months demonstrated that 50% had some residual hemiparesis, 30% could not walk without assistance, 19% had aphasia, and 26% were institutionalized in an extended care facility (2).
Despite the rapid increase in percentages and numbers of older Americans over the last century and the concentration of the burden of CVD in this group, their inclusion in lipid studies has been limited and that only recently. The elegant basic science studies of human lipoprotein physiology and the equally bold lipid intervention studies of the 1970s through the early 1990s did not include significant numbers of elderly subjects. Encouragingly, however, increasing epidemiologic and interventional data are now emerging to elucidate the interactions among aging, CVD, and frailty, information that will become even more important in the upcoming decades.
Epidemiology of Lipids and CVD with Aging and in the Elderly
The median levels of total cholesterol (TC) and low-density lipoprotein cholesterol (LDL-C) rise progressively between puberty and midlife in both sexes, increasing less in females than in males until the era of the menopause, over which median LDL-C in women rises rapidly and overtakes that in men coincident with their decreases in estrogen levels, resulting in the “postmenopausal overshoot” and higher median concentrations of TC and LDL-C in postmenopausal women than in men throughout the remainder of their healthy lives (3) (Fig. 14.1).
Data from the original Framingham Study (in which only TC was measured) suggested that for individuals under the age of 50, TC was directly correlated with their cardiovascular and total 30-year mortality, lifetime risk of coronary heart
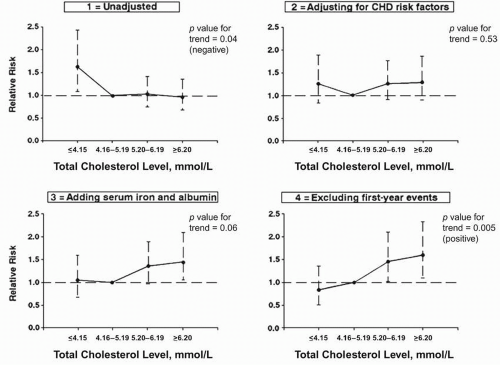
disease at age 40 years rising in parallel with cholesterol concentrations from 31% to 57% in men and from 15% to 33% in women. In contrast, individuals over the age of 50 showed no clear association between their TC and total or CVD mortality. This was thought to be confounded by the presence in that population of individuals over the age of 50 who experienced declining cholesterol levels that signified other elements of failing health (4). This paradox of lower TC being associated with greater mortality was more recently investigated in the Established Populations for Epidemiologic Studies of the Elderly (EPESE) study, a multicenter epidemiologic study with a subgroup of 4,066 men and women enrolled at age 65 or greater. Fatal coronary heart events in this study were significantly more common in participants with unadjusted TC in the lowest quartile (<160 mg/dL). However, this relationship was converted into the more expected association of higher TC with more CVD events, once adjustments were made for confounders such as visceral synthetic proteins (albumin and serum iron bound to transferrin), other cardiovascular risk factors, and first-year events (5) (Fig. 14.2). This study and other smaller supporting studies suggest that while TC retains its general predictive relationship for coronary events in the elderly-albeit with declining predictive power compared with younger groups-a falling TC may reflect visceral protein synthetic failure attributable to the inflammation of disease, impending frailty, and a high near-term risk of death.
disease at age 40 years rising in parallel with cholesterol concentrations from 31% to 57% in men and from 15% to 33% in women. In contrast, individuals over the age of 50 showed no clear association between their TC and total or CVD mortality. This was thought to be confounded by the presence in that population of individuals over the age of 50 who experienced declining cholesterol levels that signified other elements of failing health (4). This paradox of lower TC being associated with greater mortality was more recently investigated in the Established Populations for Epidemiologic Studies of the Elderly (EPESE) study, a multicenter epidemiologic study with a subgroup of 4,066 men and women enrolled at age 65 or greater. Fatal coronary heart events in this study were significantly more common in participants with unadjusted TC in the lowest quartile (<160 mg/dL). However, this relationship was converted into the more expected association of higher TC with more CVD events, once adjustments were made for confounders such as visceral synthetic proteins (albumin and serum iron bound to transferrin), other cardiovascular risk factors, and first-year events (5) (Fig. 14.2). This study and other smaller supporting studies suggest that while TC retains its general predictive relationship for coronary events in the elderly-albeit with declining predictive power compared with younger groups-a falling TC may reflect visceral protein synthetic failure attributable to the inflammation of disease, impending frailty, and a high near-term risk of death.
Thus any population of elderly persons is likely to be more heterogeneous than younger groups, containing both individuals in robust health with stable TC and those in declining
health whose TC (and LDL-C and ultimately high-density lipoprotein cholesterol [HDL-C]) levels are decreasing. This heterogeneity is further compounded by persons who have been favored by lifelong lipid levels reflecting (usually genetically determined) low levels of LDL-C (hypobetalipoproteinemia) and/or high concentrations of HDL-C, both reported decades ago as “longevity syndromes.” This phenomenon underscores the importance of measuring lipoprotein fraction as well as TC in older patients for both screening and management purposes. As noted below, however, even such measurements can be misleading, since in both populations and patients the strength of the relationship between CVD risk and TC and LDL-C progressively declines with advancing age, another paradox that defines the challenge of understanding and managing lipid levels in the elderly patient.
health whose TC (and LDL-C and ultimately high-density lipoprotein cholesterol [HDL-C]) levels are decreasing. This heterogeneity is further compounded by persons who have been favored by lifelong lipid levels reflecting (usually genetically determined) low levels of LDL-C (hypobetalipoproteinemia) and/or high concentrations of HDL-C, both reported decades ago as “longevity syndromes.” This phenomenon underscores the importance of measuring lipoprotein fraction as well as TC in older patients for both screening and management purposes. As noted below, however, even such measurements can be misleading, since in both populations and patients the strength of the relationship between CVD risk and TC and LDL-C progressively declines with advancing age, another paradox that defines the challenge of understanding and managing lipid levels in the elderly patient.
LDL and CVD in the Elderly
While multiple studies have suggested the utility of lipoprotein screening for risk assessment and primary prevention of younger and middle-aged individuals, investigations that have included the elderly fail to reveal strong associations between TC or LDL-C levels and the risk of events from CVD. In the epidemiologically robust Cardiovascular Health Study (CHS), which utilized Social Security entitlement rolls for ascertainment, 5,201 subjects at least 65 years old were recruited from four different communities, with subsequent recruitment of an additional cohort of 687 older African-American participants. During an average 7.5 years of follow-up, lipid measures proved to be relatively modest predictors of the outcomes of MI, ischemic stroke, hemorrhagic stroke, and total mortality, though there were weak associations of LDL-C and TC with MI and ischemic stroke (6). Likewise, at the upper extremes of age the focus of the Leiden 85-plus study, although CVD was the leading cause of death, the rate of death from CVD was equal among all three LDL-C tertiles (7). Thus the relationship between LDL-C and CVD events in the elderly (and perhaps especially in the “oldest old”) does not appear to hold the same strongly positive linear association seen in the premature coronary heart disease of middle-aged men.
HDL and CVD in the Elderly
By contrast, the inverse relationship between HDL-C and CVD, long noted in middle-aged individuals and notably those with the metabolic syndrome, appears to maintain its strength in aging populations. Indeed, there is broad epidemiologic evidence from studies of Okinawans, small groups of subjects in Northern Italy, and Ashkenazi Jews that suggest that higher HDL-C is a powerful longevity marker. Consistent with these findings, in the CHS the only lipid marker that was strongly (albeit inversely) associated with MI and risk of CVD was HDL-C. Moreover, in the Leiden 85-plus study, participants in the lowest tertile of HDL-C had a mortality risk of coronary artery disease of 2.0 (95% CI, 1.0 to 3.9) and a stroke risk of 2.6 (95% CI, 1.0 to 6.6). Thus the inverse relationship between HDL-C and CVD appears robust even in those over age 85.
Subclinical Vascular Disease in the Elderly
Beyond the measurement of lipoproteins, traditional risk scoring systems, such as the model developed from the Framingham Study, are less useful in assessing risk of CVD in the elderly. The straightforward use of blood pressure and TC appears less useful to predict risk in this population than more nuanced indices such as other putative biomarkers and changes in HDL-C. There are markers of subclinical vascular disease that show promise in the prediction of CVD in the elderly, especially where traditional risk factors such as LDL-C lose much of their predictive power. The utility of these subclinical vascular risk assessments exploit well-known associations in which individuals with one type of vascular disease (coronary, cerebral, peripheral) are much more likely to have latent disease in other vascular beds as well. The CHS group created a classification system for subclinical disease that included a combination of ankle/brachial blood pressure, indices of carotid artery stenosis and internal and common carotid artery wall thickness, ECG and echocardiographic abnormalities, and a positive response to the Rose questionnaire for angina pectoris (see also Chapter 6). For older men with subclinical disease defined by this combination, who were followed for a mean of 2.39 years, the increased risk ratio for total coronary heart disease was 2.0 and that for increased total mortality was 2.9. For older women with subclinical disease, the risk ratio for total coronary heart disease was 2.5, with an increased total mortality ratio of 1.7. Importantly and especially relevant to the present chapter, these associations were unchanged after adjustment for lipoprotein levels (8).
Prediction of CVD in the Elderly by Subclinical Disease
Perhaps the most important finding of CHS was that subclinical disease as so defined predicted the risk of incident events from CVD in these elderly subjects with power equal to that of a history or presence of clinical disease at entry to the study (analogous to the well-known equivalent risk of CVD in diabetics free of such disease as in nondiabetics with clinically evident CVD). Thus the issue of what constitutes primary versus secondary prevention in elderly patients becomes a semantic one; more to the point, those with subclinical CVD by this relatively simple approach are best considered to have existing CVD and treated as such according to standard guidelines. By the same token, subjects with neither clinical nor subclinical disease (about a quarter of all of those in the CHS and a third of the women) appear to remain at low risk of incident disease and should probably be managed with a validated and accepted risk formula to replace the Framingham model in the elderly, though the development of a more age-specific model would likely expedite the creation of more targeted elderly intervention programs. Taken together, the observational relationships among lipoproteins, subclinical vascular disease, and CVD events in elderly patients are clearly different from those in younger individuals. The relationship between LDL and CVD risk appears to weaken with age, while the inverse relationship of HDL with CVD appears to remain strong in the
elderly (and even among those approaching centenarian status). There is some evidence that markers of subclinical vascular disease may have better predictive power than traditional CVD risk factors, but their use in guiding aggressive primary prevention and their incorporation into a straightforward risk model has not yet been validated.
elderly (and even among those approaching centenarian status). There is some evidence that markers of subclinical vascular disease may have better predictive power than traditional CVD risk factors, but their use in guiding aggressive primary prevention and their incorporation into a straightforward risk model has not yet been validated.
LIPID INTERVENTION TRIALS IN THE ELDERLY: SECONDARY PREVENTION
The Scandinavian Simvastatin Survival Study (4S)
The majority of the early lipid-lowering intervention trials were focused on high-risk middle-aged individuals, typically those with clearly high levels of TC and LDL-C and often those with existing CVD. The first major secondary prevention study to show reduced cardiovascular endpoints with statin medications, the 4S, enrolled only a modest number of individuals between the ages of 65 and 70 (Table 14.1). While over the last 15 years there has been an effort to broaden clinical trials to enroll more individuals over the age of 65, only a small number have thus far included participants over the age of 75. Moreover, when determining relative benefits in the elderly, most trials that have included any subjects over 75 have assessed the efficacy of secondary prevention, this in a population in which the absolute rate of events is much greater attributable to their higher age per se than to their TC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree