grup and Linda M. Luxon
Introduction
Man has developed a sophisticated system for maintaining balance, which requires the integration and modulation of visual, vestibular and proprioceptive information within the central nervous system (CNS) (Figure 87.1). Pathology of any one of the three sensory inputs or of the central vestibular pathways may give rise to disequilibrium, as may many pathological processes that affect directly or indirectly the systems essential for perfect balance (Table 87.1). Dizziness is a frequent complaint in elderly people and the prevalence of balance problems at age 70 years has been reported in 36% of women and 29% of men, increasing with advanced age to 45–51% at ages 88–90 years.1 Dizziness and vestibular abnormalities are reported to be a major risk factor predisposing to falls among the elderly2 and the significance of this lies in the high morbidity and mortality associated with falls in this age group. In addition, fear of falling may constitute an independent risk factor for disability, leading older people to restrict their daily living activity unnecessarily.3 However, with the correct diagnosis, many vestibular disorders are treatable, leading to improved quality of life. Therefore, for the geriatrician, an understanding of the pathophysiology of the vestibular system and its central connections is particularly important if the common complaint of disequilibrium is to be managed successfully.
Figure 87.1 Mechanisms subserving balance in man. Reproduced from Savundra and Luxon,4 Copyright 1997, with permission from Elsevier.
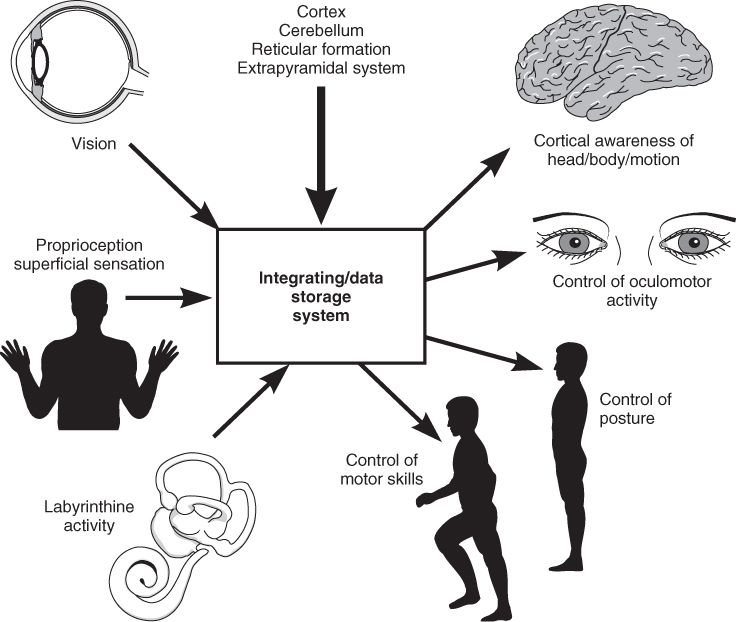
Table 87.1 Causes of dizziness in the elderly.
| General medical | |
| Haematological | Anaemia |
| Polycythaemia | |
| Hyperviscosity syndromes | |
| Cardiovascular | Postural hypotension |
| Carotid sinus syndrome | |
| Dysrhythmias | |
| Mechanical dysfunction | |
| Shock | |
| Metabolic/endocrine | Hypo- and hyperglycaemia |
| Thyroid disease | |
| Chronic renal failure | |
| Alcohol | |
| Neurological | |
| Supratentorial | Trauma |
| Neoplasia | |
| Epilepsy | |
| Cerebrovascular disease | |
| Syncope | |
| Psychogenic | |
| Infratentorial | Vertebrobasilar insufficiency |
| Subclavian steal syndrome | |
| Wallenberg’s syndrome | |
| Anterior inferior cerebellar artery syndrome | |
| Degenerative disorders including neuropathy | |
| Tumour, including those of the vestibulocochlear nerves | |
| Infective disorders | Ramsay–Hunt |
| Neurosyphilis | |
| Tuberculosis | |
| Foramen magnum abnormalities | |
| Cerebellar degeneration | |
| Basal ganglion disease | |
| Multiple sclerosis | |
| Otological | |
| Drug-induced/ototoxic | |
| Degenerative (e.g. positional vertigo) | |
| Posttraumatic syndrome | |
| Infection | |
| Vascular | |
| Tumours | |
| Menière’s syndrome | |
| Otosclerosis and Paget’s disease | |
| Autoimmune disorders | |
| Others | |
| Migraine | |
| Multisensory dizziness syndrome |
Vestibular Anatomy
The inner ear is a minute, complex, fluid-filled structure surrounded by a bony labyrinth located deep in the temporal bone. The cochlea corresponds to the acoustic end-organ, whereas the vestibular end-organs consist of the three semicircular canals, the saccule and the utricle. The semicircular canals are called the horizontal (or lateral), the posterior and the superior canal. The two ends of all semicircular canals open into the vestibule, near the utricle. One end of each semicircular canal has a dilated portion, called the ampulla, containing the sensory epithelium, that is, the hair cells. The utricle and the saccule correspond to the otolith organs and both contain a small area of sensory epithelium, called maculae. All vestibular sensory epithelium is covered with a gelatinous mass, which, in the saccule and the utricle, contains calcium carbonate-rich crystals termed otoconia. A force parallel to the surface of the sensory epithelium provides the maximum stimulus. The semicircular canals with their ampullary tissue sense angular acceleration, whereas the saccule and the utricle sense linear acceleration. The planes of the two otolith organs lie approximately at right-angles to each other. The utricular macula is oriented roughly horizontally and the saccular macula is roughly vertical. Accordingly, the saccule is well equipped to sense vertical head acceleration and the constant pull of gravity, whereas the utricle senses linear head motion in the horizontal plane. The utricle also plays an important role in signalling the spatial upright when the head is tilted with regard to gravity. The ampullae in the semicircular canals are insensitive to the static gravitational vector or position of the head in space. However, when an appropriate angular force is introduced, the fluid in the semicircular canal is displaced along the lumen of the canal leading to changed activity in the sensory epithelium of the ampullae.
Physiology and Ageing of the Vestibular Apparatus
In a normal subject holding the head in the anatomical position, the sensory epithelium in each ear generates resting neural activity, which passes via the VIIIth cranial nerve and the vestibular nuclei within the brainstem to the cortex.
Head movements result in linear and/or angular accelerations, which stimulate the vestibular sensory epithelium and modulate the neural activity in an equal but opposite manner in each ear. Hence an asymmetry of information is generated, which passes into the CNS. This asymmetric vestibular input allows cortical awareness of head position in space and provides the stimulus for compensatory eye and body movement.4
Pathology involving the peripheral labyrinth, VIIIth cranial nerve or central vestibular connections may result in an asymmetry of vestibular information, which is ‘misinterpreted’ by the brain and perceived as vertigo and instability. The incidence of vertigo has been reported to rise with advancing age, in parallel with the incidence of hearing loss.5 Histopathological age-related changes reported in the human vestibular sensory organs include progressive hair-cell degeneration, otoconial degeneration in the otolith organs and decreasing number of vestibular nerve fibres.6 In addition, age-dependent changes in both caloric and rotation test responses have been demonstrated.5, 7 However, vestibular symptoms result from an asymmetry of afferent information arising within the vestibular apparatus and degenerative changes tend to occur symmetrically. It is therefore unlikely that disequilibrium in the elderly is solely consequent upon vestibular degenerative changes and is more probably multifactorial in origin.8 Accordingly, dizziness in the elderly is often the result of central pathology and/or sensory deficits: visual impairment (not correctable); neuropathy; vestibular deficits; cervical spondylosis; and orthopaedic disorders, interfering with joint mechanoreceptors.
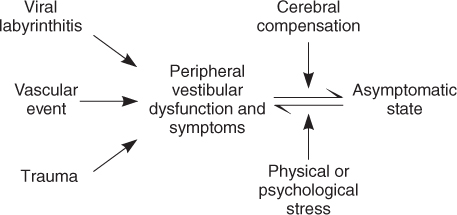
Following an acute unilateral vestibular upset, the patient experiences vertigo, but usually the symptoms are relatively short lived and resolve in 6–12 weeks, as a result of processes collectively known as cerebral compensation. Functional recovery depends on the degree of vestibular loss and cerebral compensation. The restoration of perfect balance involves reduction or abolition of the asymmetry in postural and ocular motor tone and recalibration of the gain of dynamic vestibular reflexes, in order to ensure symmetrical compensatory vestibulospinal and vestibulo-ocular reflex action during movement of the head and body. However, in some patients recovery does not occur. The persisting symptoms are usually less dramatic and the vertigo may not be rotational, but may consist of more vague symptoms of floating, rocking or a sense of depersonalization. Such symptoms may be continuous, but may also present as episodic attacks of disequilibrium frequently triggered by an intercurrent illness or a psychological upset such as bereavement (Figure 87.2). It is well established that vestibular compensation is dependent on a variety of brainstem, cerebellar and cortical structures, together with sensory inputs including vision, somatosensory afferents and remaining labyrinthine input, which are involved in the normal perception of space, body posture and locomotion. The causes of failure of compensation or intermittent decompensation are not clear, but cerebellar damage, impairment of proprioception, visual impairment, mild cerebral dysfunction and psychological disorders have all been cited as possible contributing factors. Thus, the age-dependent changes in sensory inputs and CNS function noted above would suggest that central compensation for vestibular deficits in the elderly is likely to be less efficient.
Figure 87.2 Diagram to illustrate normal sequence of events leading to recovery from a peripheral vestibular abnormality and factors relevant in decompensation.
Clinical Aspects and Diagnostic Strategy
Vertigo, defined as ‘an hallucination of movement’, is a cardinal manifestation of a disordered vestibular system, whereas dizziness is a lay term, defined in the Concise Oxford Dictionary as ‘a feeling of being in a whirl or in a daze or as if about to fall’, associated commonly with a multiplicity of general medical disorders. This semantic distinction is rarely volunteered by the elderly patient, who more frequently complains of feeling faint, swimmy or lightheaded. Hence, for practical purposes, all complaints of disorientation are considered most easily within a single diagnostic approach.
History
In the history, the character, time course and associated symptoms of the dizziness/vertigo are valuable pointers in elucidating the underlying diagnosis.
Character of Dizziness
Classically, the vertigo/dizziness of peripheral labyrinthine origin is manifested as acute, unprecipitated, short-lived attacks of rotational disequilibrium, associated with nausea and vomiting and more rarely diarrhoea, while the vertigo/dizziness of central vestibular origin is described as a more insidious, protracted sense of instability. Exceptions to the former include epilepsy and vertebrobasilar artery ischaemia, and exceptions to the latter include uncompensated peripheral vestibular disorders, bilateral vestibular failure and psychogenic disequilibrium. Additional common symptoms with peripheral vestibular dysfunction are a sensation of being pulled downward or sideways or of the room tilting and a sensation of swimming, floating and lightheadedness. However, if a clear description of subjective or objective motion is given, the suspicion of vestibular pathology is raised, whereas symptoms of lightheadedness, swimminess or faintness are more likely to be attributable to a general medical/neurological disorder.
Time Course
Acute rotational vertigo of less than 1 min duration is most commonly associated with the diagnosis of benign positional vertigo of paroxysmal type (see the following text), whereas acute rotational vertigo of less than 1 h duration may suggest the diagnosis of vertebrobasilar insufficiency. Vertigo of several hours’ duration (less than 24 h) is most commonly associated with migraine and Menière’s disease (see the following text). Acute rotational vertigo of several days’ duration, with gradual resolution of symptoms, points to a viral or vascular vestibular neuritis, although persistence of such symptoms in the elderly patient may indicate poor compensation from a peripheral vestibular insult or a fixed neurological deficit as a result of a vascular event within the brainstem. Apart from the duration of the vertigo, the time course of the episodes is also of diagnostic value. A single acute episode with gradual resolution over days or weeks would point to a peripheral vestibular pathology, such as a viral neuritis or an ischaemic event. In the elderly patient, cerebral plasticity is reduced, as noted previously, hence compensation from such a single insult may be protracted and intercurrent illness may result in an exacerbation of symptoms (decompensation). Repeated short episodes with complete and rapid recovery in between would suggest migraine, Menière’s disease or, most commonly, benign positional vertigo. It should be emphasized that in these conditions, the episodes also tend to occur in clusters, with intervals of months or even years of freedom.
Associated Symptoms
Within the labyrinth and VIIIth cranial nerve, the vestibular and cochlear elements are in close anatomical proximity. Hence pathology in these sites gives rise commonly to both cochlear and vestibular symptoms. Frequently, the elderly patient will not volunteer a complaint of tinnitus or hearing loss, as they attribute the symptoms to their age, and it is therefore important to enquire specifically. Within the CNS, the vestibular and auditory pathways diverge and vestibular symptoms of brainstem or cerebellar origin are rarely associated with cochlear symptoms, but commonly associated with neurological symptoms and signs. Loss of vestibular function leads to impaired gaze stabilization during fast head movements, that is, oscillopsia.9 Typically, the patients complain of blurred vision or bouncing images while walking or riding in a car. The vestibular system is sensitive to fast, high-frequency head movements (1–10 Hz) and cortical–optokinetic reflexes are too slow to compensate for this functional loss above 2–3 Hz. Many patients with vestibular dysfunction report a worsening or triggering of dizziness with certain visual stimuli, such as rapidly changing images, fast-moving traffic, crowds and striped material. This symptom is called visual vertigo.9 In addition, anxiety disorders, depression and panic attacks have been described in association with peripheral vestibular disease, and it is likely that in some patients vestibular dysfunction may play an important role in the aetiology of these disorders.3
Examination
A detailed medical examination is essential with special reference to the fundi, visual fields and acuity, a general neurological examination and examination of the cardiovascular and peripheral vascular systems. On the basis of a comprehensive history and a thorough examination, the diagnosis of many neurological and general medical disorders will be excluded. The diagnosis of vestibular disorders giving rise to vertigo/dizziness is based on a neuro-otological examination, which may be divided into the following:
- an examination of the external ear and otoscopy (to exclude infection, mass or perforated ear drum) together with clinical tests of auditory acuity/whispered voice tests and tuning-fork tests
- an assessment of vestibulo-ocular function
- an assessment of vestibulospinal function, as part of the overall balance.
Otological Examination
In all patients with vertigo, particularly in ethnic minorities, immigrants and immunosuppressed patients, it is essential to exclude active, chronic middle-ear disease with labyrinthine erosion. A labyrinthine fistula should be suspected in all patients with vertigo and previous surgery for middle ear disease. Clinical tests of auditory function, including tuning-fork tests (Rinne and Weber test), are important when attempting to localize pathology, since the presence of an auditory deficit may suggest an underlying labyrinthine or VIIIth nerve pathology.
Vestibulo-Ocular Examination
A detailed account of vestibular physiology and pathophysiology is beyond the scope of this chapter, but a clear understanding of these subjects is essential if an informed assessment of vestibular function and vestibular investigations are to be made.10 As has been outlined earlier, an asymmetry of vestibular activity may result from unilateral peripheral vestibular, VIIIth nerve or brainstem pathology. This asymmetry is ‘monitored’ by the brain and, via the pathways subserving the vestibulo-ocular reflex, results in a slow vestibular-induced drift of the eyes in the same direction as the peripheral labyrinthine lesion. For reasons that are not fully understood, this slow drift is interrupted by rapid saccadic eye movements, which are generated within the brainstem in the opposite direction. This combination of slow and fast eye movements is known as spontaneous vestibular nystagmus and is characteristic of acute peripheral vestibular lesions. Initially, the nystagmus present with fixation but is more prominent without fixation. As a general rule, nystagmus with fixation (nystagmus seen on routine neurological examination) disappears within 1–2 weeks after the acute lesion. By contrast, spontaneous nystagmus can be observed without optic fixation, using Frenzel’s glasses, for as long as 5–10 years after the acute episode. Spontaneous vestibular nystagmus will usually beat away from the affected side, unless the lesion is irritative (infection or tumour). By definition, for clinical purposes, the direction of the nystagmus is defined by the fast phase. Thus, a right peripheral vestibular lesion gives rise to horizontal left beating nystagmus, which obeys Alexander’s law. This states that the nystagmus is always in one direction irrespective of direction of gaze and that the intensity of the nystagmus is greatest when the eyes are deviated in the direction of the fast phase. For purposes of accurate review, nystagmus should be described in the following terms: primary nystagmus describes nystagmus which is beating in the same direction as gaze deviation; secondary nystagmus describes nystagmus in the midposition of gaze; and tertiary nystagmus describes nystagmus which is beating in the opposite direction to the direction of gaze (e.g. to the right, when the eyes are deviated to the left). Bidirectional nystagmus (e.g. first-degree nystagmus to the right on looking to the right and first-degree nystagmus to the left on looking to the left), vertical nystagmus (i.e. upbeat nystagmus and/or downbeat nystagmus) and dysconjugate nystagmus (a differing nystagmic response in each eye) indicate CNS disease, requiring further investigation. Clinically, spontaneous nystagmus should be sought in every patient complaining of dizziness/vertigo. The eyes should be examined in the midposition of gaze, with eyes 30° to the right and 30° to the left. Care must be taken that this angle is not exceeded, otherwise physiological end-point nystagmus may be observed and this may be confused with pathological nystagmus. In addition, vertical nystagmus with the eyes 30° upwards and 30° downwards should be sought.
The head thrust test is a quick and simple clinical test used to assess failure of the vestibulo-ocular reflex (Figure 87.3).11 The head thrust test is positive for the side that causes the corrective saccades, indicating a vestibular hypofunction on the same side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








