Over 45 years ago, Earle H. Spaulding (
15) devised a rational approach to disinfection and sterilization of patient-care items or equipment. This classification scheme is so clear and logical that it has been retained, refined, and successfully used by infection preventionists and others when planning methods for disinfection or sterilization (
14,
16,
18,
20,
21,
22,
23). Spaulding believed that the nature of disinfection could be understood more readily if instruments and items for patient-care were divided into three categories based on the degree of risk of infection involved in the use of the items. The three categories he described were critical, semicritical, and noncritical. Although the scheme remains valid, there are some examples of disinfection studies with viruses, mycobacteria and protozoa that challenge the current definitions and expectations of high- and low-level disinfection (
24,
25). The Spaulding terminology is employed by the Centers for Disease Control and Prevention’s (CDC’s) “Guidelines for Environmental Infection Control in Healthcare Facilities” (
26) and “Guideline for Disinfection and Sterilization in Healthcare Facilities” (
20).
CRITICAL ITEMS
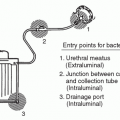
Critical items are so called because of the high risk of infection if such an item is contaminated with any microorganism, including bacterial spores. Thus, it is critical that objects that enter sterile tissue or the vascular system be sterile because any microbial contamination could result in disease transmission. This category includes surgical instruments; cardiac, intravascular and urinary catheters; implants; and ultrasound probes used in sterile body cavities. The items in this category should be purchased as sterile or be sterilized by steam sterilization if possible. If heat-sensitive, the object may be treated with ETO, hydrogen peroxide gas plasma, vaporized hydrogen peroxide, ozone, or by liquid chemical sterilants if other methods are unsuitable.
Tables 20.1 and
20.2 list several germicides categorized as chemical sterilants. These include: ≥2.4% glutaraldehyde-based formulations, 1.12% glutaraldehyde with 1.93% phenol/phenate, 3.4% glutaraldehyde with 26% isopropanol, 0.55% ortho-phthalaldehyde, 7.5% standard hydrogen peroxide, 2% improved hydrogen peroxide, 400 to 675 parts per million (ppm) hypochlorite/hypochlorous acid, 7.35% hydrogen peroxide with 0.23% peracetic acid, 0.2% peracetic acid, 8.3% hydrogen peroxide with 7.0% peracetic acid, and 1.0% hydrogen peroxide with 0.08% peracetic acid. With the exception of 0.2% peracetic acid (12 minutes at 50° to 56°C), the indicated exposure times for sterilization range from 3 to 12 hours.
27 Liquid chemical sterilants can be relied upon to produce sterility only if cleaning, which eliminate organic and inorganic material, precedes treatment and if proper guidelines as to concentration, contact time, temperature, and pH are met. Another limitation to sterilization of devices with liquid chemical sterilants is that the devices cannot be wrapped during processing in a liquid chemical sterilant, thus it is impossible to maintain sterility following processing and during storage. Furthermore, devices may require rinsing following exposure to the liquid chemical sterilant with water that generally is not sterile. Therefore, due to the inherent limitations of using liquid chemical sterilants in a nonautomated reprocessor, their use should be restricted to reprocessing critical devices that are heat-sensitive and incompatible with other sterilization methods.
SEMICRITICAL ITEMS
Semicritical items are those that come in contact with mucous membranes or nonintact skin. Respiratory therapy and anesthesia equipment, some endoscopes, laryngoscope blades, esophageal manometry probes, anorectal manometry catheters, and diaphragm fitting rings are included in this category. These medical devices should be free of all microorganisms (i.e., mycobacteria fungi, viruses, bacteria), although small numbers of bacterial spores may be present. Intact mucous membranes, such as those of the lungs or the gastrointestinal tract, generally are resistant to infection by common bacterial spores, but susceptible to other organisms such as bacteria, mycobacteria, and viruses. Semicritical items minimally require high-level disinfection using chemical disinfectants. Glutaraldehyde (with and without other active ingredients), standard hydrogen peroxide, ortho-phthalaldehyde, peracetic acid with hydrogen peroxide, improved hydrogen peroxide, and chlorine are cleared by the U.S. Food and Drug Administration (FDA) (
27) and are dependable high-level disinfectants, provided the factors influencing germicidal procedures are met. The exposure time for most high-level disinfectants varies from 8 to 45 minutes at 20° to 25°C. Outbreaks occur when ineffective disinfectants, including iodophor, alcohol, and over-diluted glutaraldehyde (
5) are used for “high-level disinfection.” When a disinfectant is selected for use with certain patient-care items, the chemical compatibility after extended use with the items to be disinfected also must be considered. For example, compatibility testing by Olympus America of the 7.5% hydrogen peroxide found cosmetic and functional changes with the tested endoscopes (Olympus, October 15, 1999, written communication). Similarly, Olympus does not endorse the use of the hydrogen peroxide with peracetic acid products due to cosmetic and functional damage (Olympus America, April 15, 1998 and September 13, 2000, written communication).
Semicritical items that will have contact with the mucous membranes of the respiratory tract or gastrointestinal tract should be rinsed with sterile water, filtered water, or tap water followed by an alcohol rinse (
20,
28,
29). An alcohol rinse and forced-air drying markedly reduces the likelihood of contamination of the instrument (e.g., endoscope), most likely by removing the wet environment favorable for bacterial growth (
29). After rinsing, items should be dried and stored in a manner that protects them from damage or contamination. There is no recommendation to use sterile or filtered water rather than tap water for rinsing semicritical equipment that will have contact with the mucous membranes of the rectum (e.g., rectal probes, anoscopes) or vagina (e.g., vaginal probes) (
20).
CLEANING
Cleaning is the removal of foreign material (e.g., soil, and organic material) from objects, and it is normally accomplished using water with detergents or enzymatic products. Thorough cleaning is required before high-level disinfection and sterilization since inorganic and organic materials that remain on the surfaces of instruments interfere with the effectiveness of these processes. Also, if the soiled materials become dried or baked onto the instruments the removal process becomes more difficult, and the disinfection or sterilization process is less effective or ineffective. Surgical instruments should be presoaked or rinsed to prevent drying of blood and to soften or remove blood from the instruments.
Instrument cleaning is done manually when the use area does not have a mechanical unit (e.g., ultrasonic cleaner, or washer-disinfector), or for fragile or difficult-to-clean instruments. If cleaning is done manually the two essential components are friction and fluidics. Using friction (e.g., rubbing/scrubbing the soiled area with a brush) is an old and dependable method. Fluidics (i.e., fluids under pressure) is used to remove soil and debris from internal channels after brushing and when the design does not allow the passage of a brush through a channel (
33). When using a washer-disinfector, care should be taken as to the method of loading instruments. Hinged instruments should be opened fully to allow adequate contact with the detergent solution. The stacking of instruments in washers should be avoided. Instruments should be disassembled as much as possible.
The most common types of mechanical or automatic cleaners include ultrasonic cleaners, washer-decontaminators, washer-disinfectors, and washer-sterilizers. Ultrasonic cleaning removes soil by a process called cavitation and implosion in which waves of acoustic energy are propagated in aqueous solutions to disrupt the bonds that hold particulate matter to surfaces. Bacterial contamination may be present in used ultrasonic cleaning solutions (and other used detergent solutions) as these solutions generally do not make antibacterial label claims (
34). While ultrasound alone does not cause significant inactivation of bacteria, sonication can act synergistically to increase the cidal efficacy of a disinfectant (
35). Users of ultrasonic cleaners should be aware that the cleaning fluid could result in endotoxin contamination of surgical instruments that could cause severe inflammatory reactions (
36). Washer-sterilizers are modified steam sterilizers that clean by filling the chamber with water and detergent through which steam is passed to provide agitation. Instruments are subsequently rinsed and subjected to a short steam sterilization cycle. Another washer-sterilizer employs rotating spray arms for a wash cycle followed by a steam sterilization cycle at 285°F (
37,
38). Washer-decontaminators/disinfectors act like a dishwasher that uses a combination of water circulation and detergents to remove soil. These units sometimes have a cycle that subjects the instruments to a heat process (e.g., 93°C for 10 minutes) (
39). Washer-disinfectors are generally computer-controlled units for cleaning, disinfecting, and drying solid and hollow surgical and medical equipment. In one study, cleaning (measured as 5- to 6-log
10 reduction) was achieved on surfaces that were adequately in contact with the water flow in the machine (
40). Detailed information on cleaning and preparation of supplies for terminal sterilization is provided by professional organizations (
41,
42) and books (
43). Studies have shown that manual and mechanical cleaning of endoscopes achieves a 4-to 6-log
10 reduction of contaminating organisms (
44,
45,
46,
47). Thus, cleaning alone is very effective in reducing the number of microorganisms present on contaminated equipment. When manual methods are compared to automated methods for cleaning reusable accessory devices used for minimally invasive surgical procedures, the automated method was more efficient and achieved a >99% reduction in soil parameters (i.e., protein, carbohydrate, hemoglobin) in both ported and nonported laparoscopic devices (
48).
The choice for instrument cleaning is neutral or near-neutral pH detergent solutions, as these solutions generally provide the best material compatibility profile and good soil removal. Enzymes, usually proteases, are sometimes added to neutral pH solutions to assist in the removal of organic material. Enzymes in these formulations attack proteins that make up a large portion of common soil (e.g., blood, pus). Cleaning solution also can contain lipases (enzymes active on fats) and amylases (enzymes active on starches). Enzymatic cleaners are not disinfectants, and proteinaceous enzymes may be inactivated by germicides. Like all chemicals, enzymes must be rinsed from the equipment, or adverse reactions (e.g., fever) could result (
49). Enzyme solutions should be used in accordance with manufacturer’s instructions. Detergent enzymes may be associated with asthma or other allergic effects in users. Neutral pH detergent solutions that contain enzymes are compatible with metals and other materials used in medical instruments and are the best choice for cleaning delicate medical instruments, especially flexible endoscopes (
46). Alkaline-based cleaning agents are used for processing medical devices as they dissolve protein and fat residues efficiently (
50); however, they may be corrosive (
46). Some data demonstrate that enzymatic cleaners are more effective cleaners than neutral detergents (
51,
52) in removing microorganisms from surfaces, but two studies found no difference in cleaning efficiency between enzymatic and alkaline-based cleaners (
50,
53). A new nonenzyme, hydrogen peroxide-based formulation (not FDA cleared) was as effective as enzymatic cleaners in removing protein, blood, carbohydrate, and endotoxin from surface test carriers (
54). In addition, this product was
able to effect a 5-log
10 reduction in microbial loads with a 3-minute exposure at room temperature (
54). Although the effectiveness of high-level disinfection and sterilization mandates effective cleaning, there are no “real-time” tests that can be employed in a clinical setting to verify cleaning. If such tests were commercially available they could be used to ensure that an adequate level of cleaning has been done (
55,
56,
57,
58). The only way to ensure adequate cleaning is to conduct a reprocessing verification test (e.g., microbiologic sampling), but this is not routinely recommended (
59). Validation of the cleaning processes in a laboratory-testing program is possible by microorganism detection, chemical detection for organic contaminants, radionuclide tagging, and chemical detection for specific ions (
57,
60). Data has been published describing the use of an artificial soil, protein, endotoxin, X-ray contrast medium, or blood to verify the manual or automated cleaning process (
40,
61,
62,
63,
64,
65) and adenosine triphosphate (ATP) bioluminescence, fluoresence and microbiologic sampling to evaluate the effectiveness of environmental surface cleaning (
66,
67,
68). Although ATP has been suggested for assessing the cleanliness of instruments, it has not been validated for this use. Minimally, all instruments should be individually inspected and be visibly clean.
Toxic anterior segment syndrome (TASS) is an acute inflammation of the anterior chamber, or segment, of the eye following cataract surgery. A variety of substances have been implicated as causes of TASS and includes impurities of autoclave steam, heat-stable endotoxin, and irritants on the surfaces of intraocular surgical instruments. General principles of cleaning and sterilizing intraocular surgical instruments have been published (
69).
DISINFECTION
A great number of disinfectants are used alone or in combinations (e.g., hydrogen peroxide with peracetic acid) in the healthcare setting. These include alcohols, chlorine and chlorine compounds, formaldehyde, glutaraldehyde, orthophthalaldehyde, hydrogen peroxide (standard), improved hydrogen peroxide, iodophors, peracetic acid, phenolics, and quaternary ammonium compounds (QUAT). Commercial formulations based on these chemicals are considered unique products and must be registered with the U.S. Environmental Protection Agency (EPA) or cleared by the FDA. In most instances, a given product is designed for a specific purpose and is to be used in a certain manner. Therefore, the label should be read carefully to ensure that the right product is selected for the intended use and applied in an efficient manner.
Disinfectants are not interchangeable, and an overview of the performance characteristics is provided (
Table 20.2), so the user has sufficient information to select an appropriate disinfectant for any item and use it in the most efficient way. It should be recognized that excessive costs may be attributed to incorrect concentrations and inappropriate disinfectants. Finally, occupational diseases among cleaning personnel have been associated with the use of several disinfectants such as formaldehyde, glutaraldehyde, chlorine and others, and precautions (e.g., gloves, proper ventilation) should be taken to minimize exposure (
70,
71,
72). Asthma and reactive airway disease may occur in sensitized individuals exposed to any airborne chemical including germicides. Clinically important asthma may occur at levels below ceiling levels regulated by the U.S. Occupational Safety and Health Administration (OSHA) or recommended by CDC’s National Institute of Occupational Safety and Health (NIOSH). The preferred method of control is to eliminate the chemical (via engineering controls, or substitution) or relocate the worker.