DIFFERENTIAL DIAGNOSIS OF HYPOOSMOLALITY
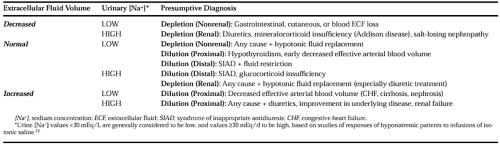
The diagnostic approach to patients with hypoosmolality includes a careful history-taking (especially with regard to medications); clinical assessment of ECF volume status; a complete neurologic evaluation; measurement of serum electrolytes, glucose, blood urea nitrogen and creatinine; calculated or direct measurements of plasma osmolality, or both; and simultaneous measurement of urinary electrolytes and osmolality. Because of the multiplicity of disorders that can cause hypoosmolality and the fact that many involve more than one pathologic mechanism, a definitive diagnosis is not always possible at the time of presentation. Nonetheless, a relatively simple evaluation with a careful interpretation of laboratory results provides a sufficient categorization of the underlying cause in most cases to allow appropriate decisions regarding initial therapy. Table 27-2 summarizes a method for the differential diagnosis of hypoosmolality based on the commonly used parameters of ECF volume status and spot urine sodium concentration (urine osmolality generally is elevated to varying degrees in most of these disorders and, therefore, is of limited value in differential diagnosis).
DECREASED EXTRACELLULAR FLUID VOLUME (HYPOVOLEMIA)
The presence of clinically detectable hypovolemia always implies total body solute depletion. If the urine [Na+] is low, a nonrenal cause of solute depletion should be sought. If the urine [Na+] is high despite hypoosmolality, renal causes of solute depletion are likely responsible, most commonly attributable to diuretic therapy. In such cases the possibility of adrenal insufficiency must always be considered as well, especially in the presence of hyperkalemia, hypoglycemia, or clinical signs of Addison disease or hypopituitarism (see Chap. 17 and Chap. 76). Finally, in hypovolemic patients not receiving diuretics and without evidence of adrenal insufficiency, salt-wasting nephropathy is possible (e.g., polycystic kidney disease, chronic interstitial nephritis), and usually requires further, more extensive evaluation of renal function for definitive diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree