CHAPTER 6 Diet and the Lifecycle
By the end of this chapter you should be able to:
• outline the changing characteristics of growth and maturation from birth to adult that alter nutrient requirements
• understand the immaturity of the digestive tract and organs during infancy, and the implications for diet
• discuss the composition of maternal milk and compare with alternatives
• describe the weaning process and advantages and risks of complementary foods
• have an informed opinion about the application of ‘healthy eating’ beliefs
• be aware of the social and psychological factors that affect food intake and nutrition during adolescence
• describe the physiological changes during pregnancy
• describe the impact of nutrition before and during pregnancy on maternal, infant and long-term health
• outline the promotion of successful lactation
• describe problems associated with breast feeding
• describe the physiological and pathological changes of ageing relevant to nutrition
• discuss important aspects of macro- and micronutrient intakes in older people
• discuss the role of nutrition in the development, susceptibility to and outcome of common chronic disabling diseases in the elderly
• understand current important public health messages to maintain and improve nutritional status in elderly people.
6.1 INTRODUCTION TO INFANCY, CHILDHOOD AND ADOLESCENCE
Growth has specific nutritional needs but is not a steady process, proceeding rapidly in early life, slowing in middle childhood and accelerating at puberty before linear growth ceases. With increasing age also come the physical and psychomotor maturation which influence activity and body composition and, through feeding skills and food choices, dietary intakes. Percentage body weight that is fat (% BF) increases rapidly to a peak between 6 and 12 months, followed by a period of natural ‘slimming’ until around 5 years, then by a second phase of relatively rapid fat deposition (the adiposity rebound) which continues in girls until growth ceases. In boys the adiposity rebound ceases with the rapid lean tissue deposition of late puberty.
6.2 NUTRITIONAL ASSESSMENT IN CHILDHOOD
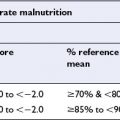
Body weight for age (WFA) is frequently used as an indicator of nutritional status but weight is heavily influenced by height. Childhood nutritional assessment (see also chapter 12) commonly uses either weight-for-height (WFH) independent of age, or WFA in relation to height-for-age (HFA). Reference standards for growth and development do not distinguish the abnormal from the extremes of normal. Scores of <−2 or >+2 SD, or <3rd and >97th centiles, are often used as cut-off points for ‘normality’. Velocity of growth may be more informative than size attained.
6.3 DEVELOPMENT AND MATURATION
Physical maturation
The typical age for onset of the secondary sexual development characteristic of puberty is considered to be between 8 and 13 years in girls and 9 and 13.5 years in boys with similar mean age (11.5 years) in both sexes. In girls the growth spurt always occurs early in the progression of puberty with most rapid growth in height on average 0.7 years after the first signs of puberty and before menarche. Growth acceleration in boys occurs later in the pubertal process, with most rapid growth occurring on average 1.5 years after the first signs of puberty, and continues longer than in girls. Peak bone mass is achieved two years after cessation of growth (mean: girls 16 years; boys 18 years). Pubertal changes in body size and composition lead to greater differences in nutrient requirements between males and females than were present in earlier childhood. In adolescent girls the nutritional needs of pregnancy and lactation may have to be added to those of growth and menstruation. In adolescent boys increased lean body mass leads to greater nutritional demands per kg body weight (see Appendix 2).
Psychomotor maturation relevant to feeding
The period of infancy (birth to 12 months) is one of almost total dependency on others for the provision of warmth, food, shelter and emotional needs. As children become more independent, they can make their wishes understood and learn to use food to manipulate those around them. Once at school, children also take their cues for food preferences from their friends and may be heavily influenced by advertising pressures. In adolescence, peer fashions can lead to haphazard eating and bizarre diets with risk of compromising the good quality diets needed to meet the demands of growth and maturation, and may be used to express independence of the family. Adolescents living away from home for the first time may lack the cooking skills required for a good diet. Lifestyles adopted in the adolescent years can continue into adult life. Adolescents (and, increasingly, younger children) may demonstrate psychiatric instability through anorexia nervosa or bulimia. These two conditions have profound, even fatal, effects (see chapter 8).
Immunological development
Food allergy and intolerance and the maturation of the immune system in relation to dietary components are discussed in chapter 10. Infants are born with unchallenged and immature immune systems. Gastrointestinal resistance to invasion by foreign proteins relies in part on protective substances such as immunoglobulins (eg IgA and IgM) and enzymes which destroy histamine and active substances in the gut. Low levels of secretory IgA (sIgA) and lack of specifically sensitized immunoglobulins make young infants more at risk of sensitization to foreign proteins which cross the mucosal barrier.
6.4 NUTRITION IN INFANCY
Breast milk
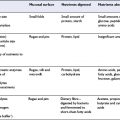
The composition of human milk is variable. The first milk, colostrum, is low in volume and high in proteins, especially immunoglobulin A, as well as vitamin A and zinc. As the volumes of milk secreted increase, milk composition modifies to ‘transitional’ and then ‘mature’ milk. Table 6.1 outlines the biochemical composition of colostrum, human milk, modern infant formula and cow’s milk. Volumes of milk produced and precise composition of breast milk vary between women, over time and by time of day. Human milk contains cells (macrophages, lymphocytes, neutrophils) and humoral components, eg sIgA, which protect infants against infection in the first months of life. Lactobacillus and Bifidobacterium spp promote lactic and acetic acid production from lactose, which discourages growth in the large bowel of potential pathogens such as E. coli and Shigella spp.
Table 6.1 Energy and selected nutrients/100 ml of colostrum, mature human milk, infant formula, and cow milk
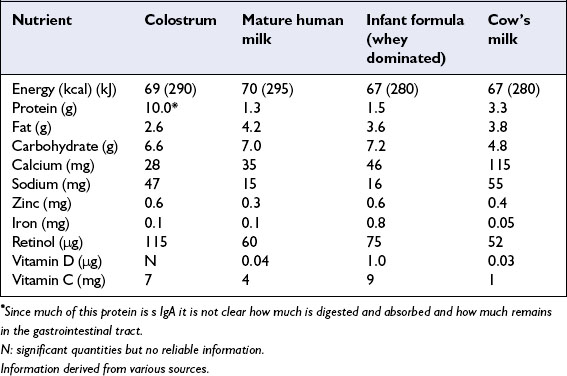
Lactose, the main carbohydrate in milk, accounts for approximately 40% of total milk energy and facilitates calcium absorption. Human milk protein is 30–40% casein and 60–70% whey. Whey proteins include lactalbumin, sIgA, lactoferrin and lysozymes, whereas casein is a mixture of proteins bound with calcium. Human milk casein forms smaller micelles with looser structure than the casein of cow’s milk, which facilitates digestion. Nutrient binding proteins in milk such as lactoferrin (which binds iron) facilitate absorption of some specific nutrients. The quantities of fat in human and cow’s milk are similar, but human milk fat is higher in unsaturated fat, particularly the essential fatty acids linoleic and α-linolenic acids, and also contains the long chain polyunsaturated fatty acids arachidonic, eicosapentaenoic and docosahexaenoic acids (22:6ω3), which are important for neurological development (see chapter 4).
The fats in human milk are more readily digested and absorbed than those of cow’s milk. Most infant formulas now contain mainly vegetable oils with rather different proportions of fatty acids than those found in human milk fat, which partly depends on maternal dietary fatty acid content. Human milk has a high level of cholesterol and of carnitine, which is involved in mitochondrial oxidation of fatty acids. Premature infants and those undergoing very rapid (catch-up) growth may be unable to synthesize carnitine at a sufficiently rapid rate to meet demand.
Formula feeding
All infant formulas are now highly modified from their base of cow’s milk or soya protein (Table 6.1). Many formulas are available and differ according to content, eg long chain polyunsaturated fatty acids, taurine, carnitine. Since the 1970s a series of government reports have made recommendations on the composition and promotion of infant formula. In 1991 an EC directive on the composition, labelling and marketing of infant and follow-on formulas was incorporated into the UK Infant Formula and Follow-on Formula Regulations. New EU regulations came into force in January 2008 but in the UK the labelling legislation will not be in force until 2010.
Specialized infant formulas
• Follow-on formulas, intended for infants over six months who are receiving complementary foods.
• Formulas for LBW infants which aim to meet the enhanced nutrient needs of very LBW and pre term (PT) infants.
• Hypoallergenic formulas for infants with strong family history of atopy and/or already diagnosed atopic disorders.
• Vegan formulas which are usually soya protein based formulas with vegetable fats.
• Other formulas– there are many very specific formulas developed to meet the needs of infants with inborn errors of metabolism and other specific illnesses.
6.5 THE TRANSITION TO MIXED FEEDING: WEANING OR COMPLEMENTARY FEEDING
Definitions
Weaning, also known as complementary feeding, has been defined as ‘The process of expanding the diet to include foods and drinks other than breast milk or infant formula’. Since the term ‘weaning’ is also used to indicate complete cessation of breastfeeding, WHO recommends that the terms ‘weaning’ and ‘weaning foods’ are avoided. The term complementary feeding is used here to embrace the use of all foods and liquids other than breast milk or infant formula.
Home-prepared versus commercial complementary foods
About 40% of home prepared complementary foods have an energy content lower than breast milk and are lower in fat, iron and vitamin D and higher in sodium than commercially prepared infant foods. UK legislation specifies a range of nutritional contents for commercially produced infant foods. Thus infants receiving commercial complementary foods may have more balanced nutrient intakes than those fed home prepared foods. If only commercial fruit, vegetable and pudding products are offered as complementary foods, energy needs are unlikely to be met as the foods displace breast milk and formula in the diet but are usually less energy dense.
6.6 NUTRITION IN CHILDHOOD AND ADOLESCENCE
Digestion and absorption in preschool children enable them to consume the same foods as adults but nutrient needs and feeding skills are different. Children’s small stomachs limit the amounts of food taken at any one meal. They should therefore be fed three meals a day and perhaps two between-meal snacks, with one snack or meal close to bedtime. Recommendations for adults to consume <35% dietary energy from fat do not apply to young children. The transition from >50% dietary energy derived from fat provided by exclusive breast feeding to <35% energy derived from fat should spread over the first five years of life. Similarly adult recommendations for fibre intake should not apply in early childhood since high fibre content lowers food energy density and phytates reduce absorption of micronutrients. Diets with <30% energy derived from fat are quite common amongst preschool children who consume large quantities of ‘juice’ and sweets instead of meals of varied content. They are likely to lead to failure to thrive if prolonged. Persuading children to eat family meals is not always easy. Children are often reluctant to eat green leafy vegetables, partly due to inexperience with chewing.
Nutritional problems in children and adolescents
Obesity
Childhood obesity (see also chapter 8) is of major public health concern. Psychological distress and the physical handicap of being obese contribute to underachievement at school. Type II diabetes mellitus (previously considered only an adult disease) shows an increased prevalence in children and adolescents in Western Europe (including the UK) and North America. The vast majority of obese children have no recognizable underlying medical cause for their obesity. Around 80% of obese children have one obese parent and 20–40% have both parents obese.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree