DIAGNOSIS
Part of “CHAPTER 75 – CUSHING SYNDROME“
STANDARD DIAGNOSTIC EVALUATION
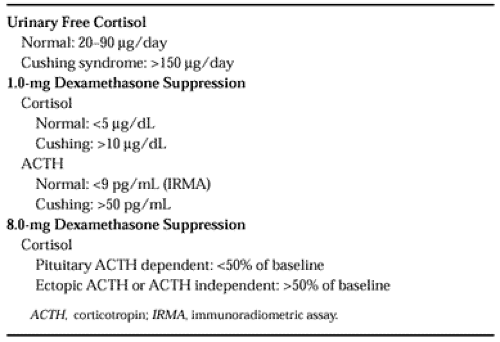
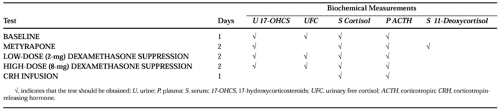
A biochemical evaluation of Cushing syndrome is necessary for confirming the clinical diagnosis and for determining the presence of the syndrome in patients with an equivocal clinical presentation.35 Preliminary testing includes the measurement of urinary free cortisol and of the ability to suppress serum cortisol levels with a low dose of dexamethasone (Table 75-2). In patients with Cushing syndrome, the urinary free cortisol usually exceeds 90 μg per day. Serum cortisol levels obtained 9 hours after the oral administration of 1 mg of dexamethasone at 23:00 hours fail to decrease below 10 μg/dL, and plasma ACTH levels (assessed by immunoradiometric assay) fail to decrease to <9 pg/mL.36 In patients without Cushing syndrome, cortisol levels are suppressed below 5 μg/dL. In patients whose levels fall between these two values, additional studies are required for confirmation of the diagnosis. After the preliminary diagnosis has been determined, a definitive diagnosis may require more extensive testing (Table 75-3). This includes the measurement of serum cortisol and plasma ACTH levels at various times of the day to determine the absence of a circadian rhythm.
Patients with Cushing syndrome, regardless of cause or type, have high baseline urinary free cortisol and serum cortisol levels and lack normal circadian changes in level. Occasionally, the early morning cortisol levels may be indistinguishable from normal, but levels obtained between 22:00 hours and midnight are clearly higher than in normal persons. This testing, however, requires that the patient be hospitalized for blood drawing. A more convenient procedure is the measurement of salivary cortisol at 08:00 and 22:00 hours or midnight in a collection that can be obtained by the patient at home. Salivary cortisol testing measures free cortisol and results correlate well with plasma cortisol levels. Patients with Cushing syndrome have high evening salivary cortisol levels.37 In borderline or confusing cases, loss of circadian rhythm may be key to establishing the differential diagnosis between Cushing syndrome and normal cortisol secretion. The pituitary response to dexamethasone is measured to detect abnormal feedback regulation of ACTH and cortisol secretion. Dexamethasone is given in doses of 0.5 mg every 6 hours for 8 doses, followed by 2 mg every 6 hours for 8 doses.
The response of plasma ACTH levels to dexamethasone depends on the type of Cushing syndrome. When an immunoradiometric assay is used (normal levels, 9–52 pg/mL), baseline levels are normal or high (50–100 pg/mL) in ACTH-dependent types and low (<9 pg/mL) in ACTH-independent types. Although ACTH levels are frequently at the upper limit of normal in patients with pituitary causes, they range from 200 to 1000 pg/mL in patients with the ectopic ACTH syndrome. The lack of normal suppression of cortisol with low doses of dexamethasone is found in all types of Cushing syndrome, but most patients with pituitary ACTH-dependent Cushing syndrome (i.e., Cushing disease) shown suppression with high doses of dexamethasone to values below 50% of the baseline levels (Table 75-4). Fewer than 10% of patients with ectopic ACTH syndrome respond in this manner. In patients with ACTH-dependent Cushing syndrome, high ACTH levels and lack of response to dexamethasone should strongly raise the possibility of ectopic ACTH syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree