Lymphoma Cytogenetics
Keywords
• Lymphoma • Cytogenetics • Fluorescence in situ hybridization • Microarray • Diagnosis • Disease progression • Prognosis
The historical significance of lymphoma cytogenetics is accentuated by the fact that a distinct chromosomal abnormality, “14q+”, was first identified and associated with Burkitt lymphoma.1 This triggered numerous investigations in search of specific chromosomal abnormalities in various malignancies. However, the maximum success came from chromosome studies in hematologic malignancies because they readily lent themselves to cytogenetic analysis. The characterization of t(8;14)(q24;q32) and its association with Burkitt lymphoma2 led to focused genetic studies in various subtypes of lymphomas. Since then, cytogenetics has played a crucial role in providing substantial insight into the genetic mechanisms of lymphomagenesis. Consistent chromosomal alterations in lymphomas, specifically, non-Hodgkin lymphomas (NHLs), have greatly impacted the classification of NHLs in general, especially the B-cell lymphomas,3–5 and has sometimes even helped establish a distinct subtype as in mantle cell lymphoma.6 Clonal and relatively complex chromosome abnormalities exist in the majority of NHLs.7 A number of recurring cytogenetic abnormalities have now been associated with various subtypes of lymphomas; these include the t(14;18) in follicular lymphoma, t(8;14) and variants in Burkitt lymphoma, t(3;14) in diffuse large B-cell lymphoma, t(11;14) in mantle cell lymphoma, and t(2;5) and variants in anaplastic large-cell lymphoma.8 In many instances, however, the association of a chromosomal alteration with a histologic subtype is not absolute, and NHLs have continued to be reclassified based on collective analysis of characteristic morphologic, immunologic, and genetic features.
With the advent of fluorescence in situ hybridization (FISH) technologies and their implementation in paraffin-embedded tissues to interrogate the existence of specific genetic alterations in defined chromosomal regions, the feasibility of achieving genetic information for specific abnormalities has increased. Retrospective molecular cytogenetic studies and newer and more insightful techniques such as array comparative genomic hybridization (aCGH)9,10 and gene expression microarrays have helped determine various other gains, deletions, and amplifications and elucidated the pathways of activation and transformation.11–17 The World Health Organization (WHO) classification has therefore approved of a multiparametric approach of utilizing the clinical, morphologic, immunophenotypic, and genetic features. This has enhanced precise interpretation of clinical and translational investigations, leading to a better molecular understanding of lymphoid malignancies.18–20 Hence cytogenetic and molecular cytogenetic studies are necessary if not imperative components in lymphoma diagnosis and progression. Here we address and adhere to the various cytogenetic and molecular cytogenetic alterations as they present in the different subtypes of lymphomas and the approaches to detect these abnormalities in lymphoid malignancies, including the mature B-cell and T-cell neoplasms and Hodgkin lymphoma (HL).
Methods
Cytogenetics
Approximately 40 minutes before the initiation of harvest, the cells are treated with Colcemid, 0.2 μg/mL. After hypotonic treatment (0.4% KCl solution for 20 minutes at 37°C), the cells are prefixed by adding 2 mL of freshly prepared chilled 3:1 methanol–glacial acetic acid fixative and gently inverting the tubes. This is followed by three additional fixation cycles and air-dried slide preparation. The slides are generally “aged” in a hot oven (100°C) for 30 minutes or in a 60°C oven overnight. The slides are then G-banded with a trypsin pretreatment. When available, at least 20 metaphases are analyzed. Karyotypes of Giemsa-banded metaphase chromosomes are typically described according to the most recent version of the International System of Cytogenetic Nomenclature (ISCN 2009).21 Abnormal clones are defined as either two or more cells with the same structural abnormality or gain of the same chromosome, or the presence of three or more cells with loss of the same chromosome. However, if an abnormal karyotype contains a known NHL-associated translocation in only one cell, it is included in the nomenclature. All normal cells are also included in the nomenclature.22–24
FISH
Depending on the availability and requirement for differential diagnosis, FISH procedures are performed either on cell suspensions prepared from cryopreserved cell pellets or on 4- to 5-μm unstained paraffin embedded tumor tissue sections. FISH probes to investigate the majority of the specific NHL-related translocations or gene disruptions are commercially available. Many laboratories generate homebrew FISH probes for detection of common abnormalities to make the testing more cost effective. The protocol for FISH studies has been outlined in another article by Karen D. Tsuchiya elsewhere in this issue. Our laboratory protocol has been described in detail previously.22–24
Cytogenetic Abnormalities in Lymphomas
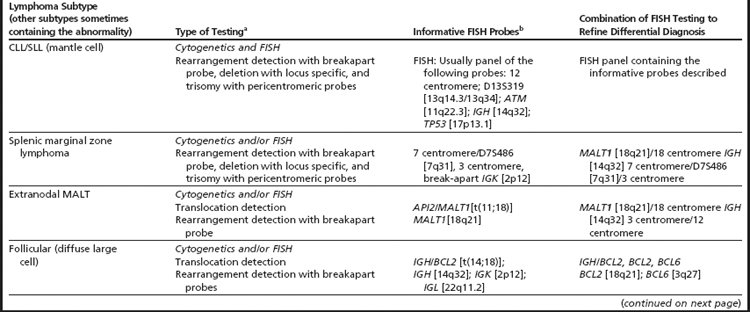
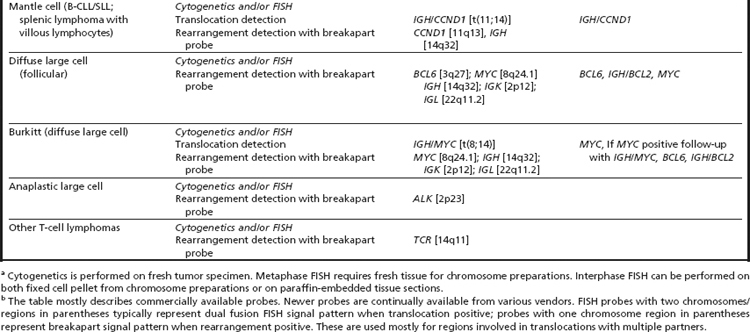
The core distinction in lymphoid malignancies historically has been HL and NHL. The majority of these are B-cell neoplasms, with fewer than 1% of HLs and 15% of NHLs being T/NK cell diseases. These may present as leukemic forms or as tumors of lymphatic organs. This section accounts for abnormalities that are identified by either conventional cytogenetics or FISH studies. Many of these present as primary abnormalities in some lymphoma subtypes, while being secondary or more downstream in clonal evolution in other subtypes. Often more than one of these abnormalities are seen in different lymphoma subtypes. To facilitate differential diagnosis, the possible existence of two or more abnormalities may need to be verified. Table 1 presents a list of primary abnormalities in most common lymphoma subtypes and Table 2 outlines the clinically available techniques to determine these abnormalities. Fig. 1 illustrates the various characteristic abnormalities and Table 3 summarizes the various recurrent cytogenetic alterations and those with prognostic implications. The descriptions of various subtypes of lymphomas have been presented in sequential order as they appear in the most recent edition of WHO classification of tumors of hematopoietic malignancies and lymphoid tissues8 and are limited only to lymphomas (plasma cell neoplasm/multiple myeloma is discussed in a separate article by Marilyn L. Slovack elsewhere in this issue).
Table 1 “Characteristic” primary chromosome abnormalities in common B- and T-cell lymphoma subtypes
| Chromosome Lesion | Gene Rearrangement | Lymphoma Subtype (other subtypes sometimes containing the abnormality) |
| Trisomy 12, del(13q), monosomy 13, del(14)(q24q32), t(14q32), del(11q22.3), del(17p13) | IGH rearrangement ATM deletion, TP53 deletion | CLL/SLL (mantle cell lymphoma) |
| t(2;7)((p12;q21) del(7q), gain 3/(3q) | IGK with CDK6 | Splenic marginal zone |
| t(11;18)(q21;q21) t(14;18)(q32;q21) t(3;14)(p14;q32) t(1;14)(p22;q32) | BIRC3 (API2)/MALT1 IGH/MALT1 FOXP1/IGH BCL10/IGH | Extranodal MALT |
| t(14;19)(q32;q13) | IGH/BCL3 | Nodal marginal zone |
| t(14;18)(q32;q21) and variants t(2;18)(p12;q21), t(18;22)(q21;q11.2) | IGH/BCL2IGK/BCL2BCL2/IGL | Follicular (diffuse large cell) |
| t(11;14)(q13;q32) | CCND1/IGH | Mantle cell (CLL/SLL; splenic lymphoma with villous lymphocytes) |
| t(3;14)(q27;q32) and multiple 3q27 partners t(3q27) | BCL6/IGH BCL6 rearrangement | Diffuse large cell (follicular) |
| t(8;14)(q24;q32) variants t(2;8)(p12;q24) and t(8;22)(q24;q11.2) | MYC/IGH IGK/MYC IGL/MYC | Burkitt (diffuse large cell) |
| t(2;5)(p23;q35) and multiple 2p23 partners t(2p23) | ALK/NPM ALK rearrangement | Anaplastic large cell |
| 14q11 rearrangements | TCR | Other T-cell lymphomas |
Table 3 Recurrent cytogenetic abnormalities including those with prognostic relevance in different categorized subtypes of B- and T-cell lymphomasa
| Lymphoma Subtype | Recurrent Chromosome Abnormalitiesa | Chromosome Abnormalities with Prognostic Relevanceb |
| B-Cell Lymphoma | ||
| B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma | Trisomy/gain: 3, 12, 18, 2p24–25, 3q26–27, 8q24 Monosomy/deletions/loss: 6q, 11q, 13q, 14q24–32,17p, Rearrangements: 2p12 (IGK), 6q21–23, 11q22–23, 12p13–15, 13q14.3, 14q22, 14q32 (IGH), 22q11.2 (IGL) Translocations: t(8;14)(q24;q32) and variants, t(9;14)(p13;q32), t(11;14)(q13;q32), t(14;18)(q32;q21) and variants, t(14;19)(q32;q13.3) | Poor prognosis: del(17p), del(11q), del(6q) t(8q24)/+8q24, del (9)(p21) Favorable prognosis: isolated 13q14.3 deletions |
| B-Promyelocytic | Abnormalities observed in CLL/SLL (trisomy 12 rare) Complex karyotypes | ND |
| Splenic marginal zone | Trisomy/gain: 3q Monosomy/deletions/loss: del(7q31–32) Translocations: t(11;14)(q13;q32), t(2;7)(p12;q21) | Poor prognosis: del(7q) |
| Hairy cell leukemia | Trisomy/gain: 5q13–31 Monosomy/deletions/loss: 14q22–24 Rearrangements: 14q, 15q | ND |
| Splenic B-cell leukemia/lymphoma, unclassifiable | Monosomy/deletions/loss: 17p13 (TP53) Rearrangements: 8q24, 14q32, 3q27 Complex rearrangements | ND |
| Lymphoplasmacytic | Trisomy/gain: 3 Deletions/loss: 6q Translocations: t(9;14)(p13;q32) | Poor prognosis: del(6q) |
| Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) | Trisomy/gain: 3, 18, 3q (3q27), 9q (9q34), 18q Rearrangements: 2q, 3q27 Translocations: t(1;14)(p22;q32), t(1;2)(p22;p12), t(11;18)(q21;q21), t(14;18)(q32;q21) (18q21–MALT1), t(3;14)(p14.1;q32) | Poor prognosis: del(9p), del(17p), t(1;14)(p22;q32), partial or complete trisomy of 18 |
| Nodal marginal zone | Trisomy/gain: 3, 18 Translocations: t(14;19)(q32;q21) Complex karyotypes | ND |
| Follicular | Trisomy/gain: X, 3, 5, 7, 8, 12 (12q), 18 (18q) Monosomy/deletions/loss: 1p36, 6q21, 6q23–26, 9p21, 10q22–24,17p13 Rearrangements: 1p, 3q27, 6q23–26, 11q, 12q13–15, 18q21, frequently as +der(18)t(14;18) Translocations: t(14;18)(q32;q21) and variants involving (18q21) BCL2, t(3;14)(q27;q32) and variants involving (3q27) BCL6 | Transformation/aggressive clinical course/poor prognosis: +X, del(1)(p36) +7, del(6q), del(9)(p21) (CDKN2A), 8q24 (MYC abnormality), del(10)(q22–q24), +11q, +12, and del(17p) (TP53), +18, and +der(18)t(14;18) Total number of abnormalities, presence of polyploidy, and markers |
| Mantle cell | Trisomy/gain: 3 (3q), 12 (12q) Monosomy/deletions/loss: Y, 1p, 6q, 9 (9p),10q, 11q, 13 (13q), 17p,18 Rearrangements: 1p13–p31, 3q27, 6q11–15, 6q23–27, 7p21, 8q24, 9p21, 10p12–13, 11q22–23, 13q11–13, 13q14–34, and 17p13-pter Translocations: t(11;14)(q13;q32), t(12;14)(p13;q32), t(2;12)(p12;p13), t(6;14)(p21;q32) and occasionally translocations involving (3q27) BCL6 | Transformation/aggressive clinical course/poor prognosis: Involvement of (8q24) MYC locus +3q, −9q, +12, del(13)(q14), del(17p) TP53, karyotypic complexity |
| Diffuse large-cell lymphoma (DLBCL) | Trisomy/gain: X, 3, 7, 9, 12, 18, 1q23–31, 1q32–44, 3q, 6p, 7p, 7q31–32, 8q22–24, 11q12–13, 12q14–24, 18q11–21, and 22q12-qter Monosomy/deletions/loss: Y, 4, 6, 13, 15, 17, 1p36-pter, 2p23-pter, 4q32-qter, 6q21–25, 8p12-pter, 9p21-pter, 11q23-qter, 12p12–13, 14q23-qter, 17p12–13, 18q21-qter Other breakpoints in rearrangements: 1p22, 1q21, 1q25, 3p21, 3q27, 4q31, 6p21, 7q33, 8q21, 8q24, 9p24, 16p13, 18q21, 19q13 Translocations: t(3;14)(q27;q32), t(2;3)(p12;q27), t(3;22)(q27;q11.2), t(8;14)(q24;q32), t(14;18) q32;q21 Breakpoints involved with 3q27 (BCL6): 4p13, 6p22, 7p13, 8q24, 11q23, 13q14, 15q22, 17q11 | Transformation/aggressive clinical course/poor prognosis: Del(9)(p21), del(17p), dup(1q), MYC rearrangement Reduced risk: Trisomy 5, 5q, 7q |
| DLBCL subtypes | ||
| T-histiocyte-rich large cell lymphoma (THRLBCL) | Trisomy/gain: Xq, 4q13–28, Xp21–11, 18q21 Monosomy/deletions/loss: 17p | ND |
| Primary DLBCL of central nervous system | Trisomy/gain: 12q, 22q, 18q21, with BCL2 and MAlT1 amplification Monosomy/deletions/loss: 6q | ND |
| Primary cutaneous DLBCL, leg type | Trisomy/gain: of 18q21.31–21.33, with BCL2 and MALT1 amplification Monosomy/deletions/loss: 9p21.3 (CDKN2A and CDKN2B) Translocations: involving CMYC, BCL6, and IGH | ND |
| EBV-positive DLBCL in elderly | ND | ND |
| Other lymphomas of large B cells | ||
| DLBCL associated with chronic inflammation | Complex karyotypes with numerous numeric and structural abnormalities | ND |
| Lymphoid granulomatosis | Nonrandom cytogenetic aberrations yet to be identified | ND |
| Primary mediastinal (thymic) large B-cell | Gains: 9p24, 2p15, Xp11.4–21 and Xq24–26 | ND |
| Intravascular large B-cell | Monosomy/deletions/loss: 6q21–24 Rearrangements of:1, 4, 5, 6, 8, 10 Translocations: t(11;14)(q13;q32), t(14;18)(q32;q21) | ND |
| ALK-Positive DLBCL | Translocations: t(2;17)(p23;q23) | ND |
| Plasmablastic lymphoma | ND | ND |
| HHV8-associated multicentric Castleman disease | ND | ND |
| Primary effusion lymphoma (PEL) | Trisomy/gain: X, 7, 12(12q) Rearrangements: 1q, complex karyotypes Translocations: t(8;14)(q24;q32) and variant MYC translocations | ND |
| Burkitt | Trisomy/gain: 7(7q), 8, 12, 1q21–25 Monosomy/deletions/loss: 6q, 7q, 8q, 13q, 17p Rearrangements: 1q23–31, 3q27, 8q24, 14q32, 17p13.1 Translocations: t(2;8)(p11;q24.1), t(8;14)(q24.1;q32), t(8;22)(q24.1;q11.2) | Transformation/aggressive clinical course/poor prognosis: del(13q) |
| B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and Burkitt lymphoma | Rearrangements: 3q27, 8q24, 14q32Translocations: t(2;8)(p11;q24.1), t(8;14)(q24.1;q32), t(8;22)(q24.1;q11.2), t(14;18)(q32;q21), t(3q27) BCL6 | Transformation/aggressive clinical course/poor prognosis: MYC rearrangement in addition to t(14;18)—“double hit” |
| T-cell lymphoma | ||
| T-cell prolymphocytic leukemia | Trisomy/gain: 6p, 8 (8q) (cytogenetics and CGH) Monosomy/deletions/loss: 6q, 8p, 10p (cytogenetics and CGH) Rearrangements: i(8)(p11), 11q (ATM), 17p, 22q Translocations: t(14;14)(q11;q32), (X;14)(q28;q11) | ND |
| T-cell large granular lymphocytic leukemia | Deletions/loss: 6q Rearrangements: 7p, 7q, 14q11 (TCR loci) | ND |
| Chronic lymphoproliferative disorders of NK cells | Usually normal karyotype | Transformation/aggressive clinical course/poor prognosis: Presence of karyotypic abnormalities |
| Aggressive NK cell leukemia | Trisomy/gain: By CGH (1p32-pter, 6p, 11q, 12q, 17q, 19p, 20q, and Xp) Monosomy/deletions/loss: del(6q21q25), 11p (by CGH, X, 6q16–27, 13q14–34, 11q22–25, 17p13) | ND |
| EBV-positive T-cell lymphoproliferative disorders of childhood | ND | ND |
| Adult T-cell | Trisomy/gains: 1p36, 1q, 2p, 3p, 4q, 6p25, 7p (7p22), 7q, 14q32 Monosomy/deletions/loss: 6q (6q15–21), 10p, 13q, 16q, 18p Rearrangements: 1p, 1q, 3q, 5p, 5q, 9q, 10p, 10q, 11q, 12q, 18q Translocation: t(14;14)(q11;q32) Rearrangements with 14q11: Xq, 1p, 1q, 3p, 3q, 8q, 10p, 11p, 12q, 18p | ND |
| Extranodal NK-T cell lymphoma, nasal type | Gains: 2q Loss: 1p36.23–36.33, 2p16.1–16.3, 4q12, 4q13.3–32.1, 5p14.1–14.3, 5q34–35.3, 6q16.1–q27, 11q22.3–23.3 | ND |
| Enteropathy-associated T-cell lymphpma (EATL) | Gains: 1q, 5q, 7q, 9q (9q31.3-qter), 16q12.1 Classic ETL-linked to celiac disease-gains:1q, 5q Monomorphic variant ETL-gain: MYC locus Loss: 8p, 9p, 13q | ND |
| Hepatosplenic T-cell lymphoma (HSTL) | Gain: 7, i(7q), 8 Loss: X, Y Rearrangements: 7q | ND |
| Subcutaneous penniculitis-like T-cell lymphomas (SPTL) | Trisomy/gain: 2q, 4q, 5q, 13q Monosomy/loss:1pter, 2pter, 10qter, 11qter, 12qter, 16, 19, 20, 22 | ND |
| Mycosis fungoides (MF) and Sezary syndrome (SS) | Trisomy/gain: 7, 8q, 17q, 18 Monosomy/loss: 1p, 6q, 9, 10, (10q) 10q, 13q, 17p, 19 Rearrangements: 1p32–36, 1q, 2q, 6q22–27, 8q22, 10q23–26, 12q21, 12q22, 17p11–13, 19p13.3, complex karyotypes Deletion NAV3 (POMFIlI) and amplification of JUNB in SS (FISH and CGH) | Transformation/aggressive clinical course/poor prognosis: Gain of 8q and loss of 6q and 13q |
| Primary cutaneous CD-30 positive T-cell lymphoproliferative disorders | Trisomy/gain: 9 Monosomy/loss: 6q21 and 18p11.3 | ND |
| Primary cutaneous peripheral T-cell lymphomas, rare subtypes | ND | ND |
| Primary cutaneous γδT-cell lymphomas | ND | ND |
| Peripheral T-cell lymphoma not otherwise specified | Trisomy/gain: 1q, 3p, 5p, 7q22–31, 8q24-qter, 11q13 17q (17q11–25),12p13, 22q Monosomy/deletions/loss: 4q, 5q, 6q22–24, 9p (9p21–q33), 10p13-pter, 10q (10q23–24), 11p11, 12q (12q21–22),13q (13q21) Translocations: t(14;19)(q11;q13), t(5;9)(q33;q22) | ND |
| Angioimmunoblastic T-cell lymphomas | Trisomy/gain: X, 3 (3q), 5 (5q), 11p11–q14 (11q13), 19, 21, 22q Monosomy/deletions/loss: 6q, 13q | Transformation/aggressive clinical course/poor prognosis: +X, aberrations of 1p31–32, and complex abnormalities |
| Anaplastic large cell (ALCL) ALK-positive | Trisomy/gain: X, 7, 9, 17p, and 17q24-qter Monosomy/deletions/loss: Y, 4q13–21, 6q, 17, 11q14, 13q Translocations: t(2;5)(p23;q35) Rearrangements with 2p23 (ALK): 1q25, inv(2)(p23q35) 3q21, 17q23, 19p13.1, 22q11.2, 17q25, Xq11–12 | Favorable prognosis: t(2;5)(p23;q35) and variants involving ALK |
| Anaplastic large cell lymphoma (ALCL) ALK-negative | Trisomy/gain: 1q, 3p, 6p21, 7 Monosomy/deletions/loss: 6q13–21, 13q, 15, 16pter, 16qter, 17p13 | ND |
| Hodgkin Lymphoma | ||
| Nodular lymphocyte predominant Hodgkin Lymphoma (NLPHL) | Similar rearrangements as in DLBCL t(3q27)(BCl6) rearrangements Polyploid (triploid to tetraploid)—complex karyotypes | Poor prognosis: del(13q) |
| Classical Hodgkin (cHL) | Gains: 4p16, 4q23–q24 and 9p23–p24 Monosomy/deletions/loss: 1p, 3p, 6q, 7q Rearrangements: 1p36, 6q15, 6q21, 7q22, 7q32, 8q24, 11q23, 12q24, 13p11, 14p11, 14q32, 15p11, 19p13 Translocation: t(14;18)(q32;q21) and other 14q32 (IGH) translocations with 2p16, 3q27, 8q24, 16p13, 17q12, 19q13 Polyploid (triploid to tetraploid)—complex karyotypes | ND |
B-Cell lymphomas
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
A rare disease in Eastern countries and the most common leukemia of adults in Western nations, chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) accounts for about 7% of NHL. The term SLL is used for the nodal form with the tissue morphology and immunophenotype of CLL. Of all hematologic malignancies, CLL/SLL shows the highest genetic predisposition.25 Cytogenetic abnormalities have been detected in nearly 80% of CLL/SLL, specifically by FISH techniques.26–28 The malignant CLL cells have a poor response to conventional mitogens; thus previous studies identified the cytogenetic abnormalities at a different frequency than those observed with specific FISH probes.27,29–31 Interphase studies demonstrated that del(13q) is the most common abnormality detectable by FISH.31 This is followed by trisomy 12 and deletions of 11q22–q23, 17p13, and 6q21.27 The use of mitogenic agents such as CD40L and immunostimulatory CpG-oligonucleotide DSP30 and IL2, has improved the percentage of metaphase chromosome abnormalities in CLL cases. CLL/SLL primarily depicts genomic imbalances; more chromosomal abnormalities and rare reciprocal translocations are observed with an overall karyotypic evaluation than focused FISH studies.28 The expression of tyrosine kinase ZAP-70 is associated with IGHV unmutated CLL genotype.17 The distribution of genomic abnormalities varies depending on the mutational status of VH.25 Trisomy 12, del(13q), del(11q), and del(17p) are frequently observed independent of each other. However, combinations of these abnormalities appearing together are not uncommon. The del(11q) and del(17p) are recurrently noted as secondary changes. Although rare, trisomies of 3, 8, and 18 and del(6q) have been observed, recurrently.32
Trisomy 12, frequently associated with atypical morphology,32 is found in nearly one third of CLL with abnormal karyotypes and in about 15% of all CLL as detected by FISH,29 with the minimum common gain being 12q13. Other additional recurrent aberrations among the trisomy 12 cases include trisomies of 18 and 19,33 t(14;18)(q24;q32) IGH-BCL2 fusion,34 t(14;19)(q32;q13) leading to IGH–BCL3 fusion,35 and del(14)(q24q32) with one breakpoint in IGH locus.36 Variant translocations including the 2p12 and 22q13 (IGK and IGL, respectively) are also observed. After initial FISH studies,29 abnormalities of 13/13q were accepted as the most frequent alteration in CLL/SLL. These are observed in 50% of CLL by FISH and in about 20% of abnormal karyotypes. The critical deletion region involves 13q14 and excludes the RB1 gene.37,38 Monoallelic as well as biallelic losses of 13q14, and monosomy/nullisomy of 13, have been observed in CLL/SLL. Deletions of 11q, involving the minimum deletion region 11q22–q23 which included the ATM gene, are observed mostly by interphase FISH studies.27,30,39 Structural abnormalities of 17p including deletions of TP53 are also seen in CLL/SLL and are associated with an unfavorable prognosis.28,40 Most cases containing translocation t(11;14)(q13;q32) linking the IGH–CCND1 genes may now be classified as mantle cell lymphoma (MCL); however, this may also rarely be noted CLL/SLL.
Progression of CLL/SLL to B-PLL is rare; however, an acute transformation to a diffuse large cell lymphoma, known as Ritcher’s syndrome, takes place in some cases and a very low percentage develop HL. Complex karyotypes, deletions of TP53 and ATM, and involvement of 8q24 (MYC region) and 9p21 (CDKN2A) are indicators of transformation,41 while isolated 13q14.3 deletions are associated with a favorable prognosis.27
B-Cell Prolymphocytic Leukemia
A neoplasm of B prolymphocytes with more than 55% of lymphocytes being prolymphocytes, B-cell prolymphocytic leukemia (B-PLL) is an extremely rare disease, comprising approximately 1% of lymphocytic leukemias.42 Chromosome abnormalities that are common in CLL/SLL are also characteristic of B-PLL.26,28,40 Complex karyotypes with nearly 50% cases containing the deletion of 17p including the TP53 gene have been demonstrated in B-PLL. In addition, deletions of 13q14 are also noted by FISH analysis. Trisomy 12 is rare in B-PLL.43 The initial finding of nearly 20% cases of B-PLL containing t(11;14)(q13;q32)44 is now refined, and these cases are more likely considered to be leukemic variants of mantle cell lymphoma.43,45
Splenic B-Cell Marginal Zone Lymphoma
Constituting about 2% of the lymphoid neoplasms, splenic B-cell marginal zone lymphoma (SMBZL) is seen mostly among patients older than 50 years of age.46 SMBZL is composed of small lymphocytes that surround and replace the splenic white pulp germinal center, efface the follicle mantle, and merge with a peripheral (marginal) zone of larger cells. Lymphoma cells may be found in the peripheral blood as villous lymphocytes (splenic lymphoma with circulating villous lymphocytes [SLVLs]).47 Deletion of 7q is the most frequent abnormality in SMBZL and is observed in nearly 40% of the cases; the critical region is 7q31–32. Gain of 3q and numerous other abnormalities have also been described.48–50 In addition, dysregulation of CDK6 gene as a result of a t(2;7)(p12;q21) has been demonstrated in some cases.51,52 The t(11;18), common in extranodal marginal zone lymphoma of mucosa associated lymphoid tissue (MALT), is absent in SMBZL. The presence of a 7q deletion may be associated with an unfavorable outcome.47,53
Hairy Cell Leukemia
An indolent and rare disease of small mature B lymphoid cells with oval nuclei and abundant cytoplasm with “hairy” projections, hairy cell leukemia (HCL) constitutes 2% of lymphoid leukemias, occurring at a median age of 50 years and exhibiting a strong male predominance (5:1 male to female ratio).54 Structural rearrangements of 14q including translocations involving 14q32 and deletions of 14q22−24 have been described.55 Further, abnormalities of chromosome 5 including gains in 5q13–31 have been observed.56,57
Lymphoplasmacytic Lymphoma
Lymphoplasmacytic lymphoma (LPL) involves small B lymphocytes, plasmacytoid lymphocytes, and plasma cells, usually involving bone marrow and sometimes lymph nodes and spleen. Walderstom macroglobulinemia (WM) is found in a large subset and is usually defined as LPL with BM involvement. These LPLs are characterized by excessive proliferation of an immunoglobulin M (IGM)-producing clone of malignant plasmacytoid cells.5 The distinction between marginal zone lymphoma (MZL) and LPL is sometimes difficult. These cases may be described as small lymphocytic lymphoma with plasmacytic differentiation.58 No specific cytogenetic abnormality is currently defined as a hallmark of LPL. Previously these lymphomas were associated with a characteristic translocation t(9;14)((p13;q32) involving the PAX5/IGH genes59; however, the translocation is rarely observed in LPL and is also observed in other B-cell neoplasms.60,61 Although deletion of 6q is nonspecific for LPL, it is most frequently noted in LPL/WM (6q21 deletions by FISH).62 Cases with a deletion of 6q have been associated with an adverse prognosis.
Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT lymphoma)
Composed of morphologically heterogeneous small B cells including marginal zone (centrocyte-like) cells, small lymphocytes, scattered immunoblasts, and centroblast-like cells, MALT lymphoma is an extranodal lymphoma that comprises 7% to 8% of all B-cell lymphomas.63 The differential diagnosis of MALT lymphoma includes the reactive inflammatory processes including Helicobactor pylori gastritis that typically precede the lymphoma and other small B-cell lymphomas (follicular lymphoma, mantle cell lymphoma, small lymphocytic lymphoma). The t(11;18)(q21;q21) is the most frequent translocation that occurs in MALT lymphoma. The API2 (BRIC3) gene on 11q21 and the MALT1 gene on chromosome 18q21 are disrupted and recombined to form a API2–MALT1 fusion gene on the derivative chromosome 11.64–66 Most often this appears as a sole abnormality.67–69 Approximately 15% of MALT lymphomas reveal the t(11;18) when molecular or FISH techniques are utilized; the majority of these are the gastric and pulmonal MALT cases.70,71 The t(11;18) appears to be specific for MALT lymphomas and has not been observed in nodal and splenic marginal zone B-cell lymphomas.64,65,72 Three other recurrent and mutually exclusive translocations are observed in MALT lymphoma. The t(14;18)(q32;q21), which deregulates the MALT1 gene through IGH juxtaposition,73,74 is observed in nearly 11% of MALT lymphomas, more frequently in ocular adnexel and liver lymphomas.70,71 This translocation can be distinguished from the cytogenetically identical t(14;18)(q32;q21) involving the IGH and BCL2 by using FISH techniques. The t(3;14)(p14.1;q32) resulting in the transcriptional deregulation of FOXP1 on 3p14.172 was identified in 10% of MALT lymphomas of thyroid, ocular adnexae/orbit, and skin. The t(1;14)(p22;q32), which juxtaposes the BCL10 gene with the IGH locus,75,76 is seen in 2% of MALT lymphomas.71 A variant t(1;2)(p22;p12) involving the IGK locus has also been described.77
Trisomies of 3 and 18 are seen in nearly 30% of all MALT lymphomas, including those that are translocation negative. Trisomies are more commonly seen in intestinal, salivary gland, and orbital adnexal lymphomas.70 Partial gains of 3q (3q27), 9q (9q34), and 18q are common in MALT.78,79 Deletions of 6q have also been observed in aCGH studies.80 MYC amplifications, del(9p), and del(17p) are seen in progressive disease.69–71 The t(1;14) and partial or complete trisomy 18 predict adverse clinical behavior.81 FISH studies on paraffin-embedded tissues help in the differential diagnosis of marginal zone and MALT lymphomas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree