Cystic Lesions
Sung Wook Seo
Young Lae Moon
Francis Young-In Lee
This chapter includes cystic lesions which may occur in bone. Epidermal inclusion cysts and ganglions may also occur in soft-tissues, where the pathophysiology is similar. Simple bone cysts and aneurysmal bone cysts represent distinct clinical entities which occur within bone only.
Epidermal Inclusion Cyst
Epidermal inclusion cysts are more commonly seen as soft-tissue lesions, but may involve bone, and present in either case as painful digital lesions which typically require surgical extirpation.
Pathogenesis
Etiology
For both soft-tissue and intraosseous epidermal inclusion cysts, penetrating trauma causes epidermal tissue to be deposited deep within the tissues
Pathophysiology
Epidermal tissue traumatically deposited within the deeper tissue grows and causes cyst formation
Cystic lesion filled with keratinous materials lined with flattened squamous epithelium
Diagnosis
Physical Examination and History
Clinical Features
Painful, often swollen mass most often within distal digit
History of penetrating trauma in many cases
Radiologic Features
Intraosseous geographic radiolucent lesion
Distal phalanx of fingers common
Pathologic findings
Cystic cavity filled with keratinaceous debris
Diagnostic Workup Algorithm
Differential diagnosis includes intraosseous synovial or ganglion cyst
Diagnosis usually apparent radiographically, confirmed histologically
Treatment
Surgical Indications/Contraindications
Painful lesions bone can be curetted and grafted
Degenerative Cyst (GEODES)
Pathogenesis
Etiology
Related to underlying degenerative arthritis
Pathophysiology
Damage to cartilage theorized to allow fluid intravasation within bone, leading to cyst formation
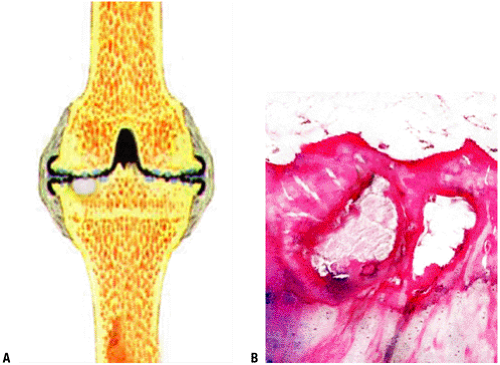
Pathology: Cystic lesion filled with fluid or gelatinous or proteinaceous material, demarcated by fibrocartilaginous tissues (Fig. 5.3-1)
Diagnosis
Physical Examination and History
Clinical Features
Dictated by manifestations of underlying arthritis
Pain, local tenderness, variable stiffness, loss of motion
Radiologic Features
Plain x-ray
Cyst: geographic, smooth, often sclerotic borders with central radiolucency within epiphysis immediately adjacent to joint, often on both sides of joint
Variable associated arthritic changes:
loss of joint space, osteophytes, subchondral sclerosis, subluxation may be present
some joints show few or no degenerative changes
MRI
Pathologic findings
Cystic cavity filled with serous fluid, proteinaceous, or gelatinous material and lined with flattened fibrocartilaginous tissues
Diagnostic Workup Algorithm
Usually evident radiographically without the need for histological confirmation
In presence of established arthritis, plain radiographs often suffice
In absence of other radiographic signs of arthritis, MRI may be useful
Differential diagnosis includes other epiphyseal lesions
PGCAT: Pigmented villonodular synovitis (PVNS), giant cell tumor of bone, chondroblastoma, clear cell chondrosarcoma aneurysmal bone cyst, tuberculosis (and other cause for Brodie’s abscess)
Treatment
Surgical Indications/Contraindications
If diagnosis is clear, direct treatment towards underlying joint arthritis
If diagnosis not clear, biopsy may be necessary
Simple Bone Cyst (Unicameral Bone Cyst)
Unicameral bone cyst is a serous or serosanguineous fluid-filled cavity which typically behaves in an inactive fashion, not causing symptoms until pathological fracture occurs through the cyst. The clinical presentation, location, and radiographic features are classic enough that the diagnosis may usually be readily established. Treatment continues to evolve, and is site dependent, but often involves aspiration and injection.
Pathogenesis
Etiology
Unknown but theories suggest epiphyseal plate defect or venous outflow obstruction
Epidemiology
Ages
Peak incidence 4–10 years of age
85% within first two decades
Gender: Males > females 3:1
Distribution
Proximal humerus most common
Proximal femur #2
Calcaneus #3
Other relatively common sites: proximal tibia, ilium
Most common sites in adults: calcaneus and ilium
Pathophysiology
Unknown
Classification
Active position: Immediately juxtaposed to growth plate
Not to be confused with Enneking stage 2 benign (active) classification
Inactive position: Growth plate no longer adjacent to cyst
Not to be confused with Enneking stage 1 benign (inactive) classification
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree