Corticotropin (ACTH)-dependent hypercortisolism is commonly due to an ACTH-secreting pituitary adenoma (80%–90%). Most patients with ACTH-dependent hypercortisolism are women with slowly progressive mild to moderate Cushing syndrome (CS) who will have an ACTH-secreting pituitary tumor. The mean time from symptom onset to diagnosis in patients with pituitary CS is more than 3 years, and the diagnosis is frequently confused with polycystic ovarian syndrome. When a clear-cut pituitary tumor is found on magnetic resonance imaging (MRI) in a woman with slowly progressive and mild-to-moderate ACTH-dependent CS, proceeding directly to transsphenoidal pituitary surgery (TSS) is a reasonable next step.
Case Report
The patient was a 33-year-old woman who was referred for evaluation and management of a pituitary adenoma. The pituitary lesion was incidentally discovered on a recent MRI of the brain that was performed due to severe headaches several times a week (“15/10” in intensity). Her medical history was positive for polycystic ovarian syndrome diagnosed 5 years ago (based on symptoms of weight gain and hirsutism), newly diagnosed diabetes mellitus type 2, mild hypertension, and anxiety. Since high school, she had gradually gained 140 pounds in weight and noticed progressive development of dorsocervical and supraclavicular pads. Her menstrual cycles were irregular. Her medications included alprazolam, 0.25 mg as needed for anxiety; metformin, 500 mg twice a day; and liraglutide, 1 mg daily for treatment of diabetes mellitus type 2. On physical examination, her blood pressure was 132/88 mmHg, and her body mass index (BMI) was 46.6 kg/m 2 . She was obese. She had mild supraclavicular pads, a dorsocervical pad, mild facial rounding, and mild facial erythema. She did not have signs of easy bruising, thinning of the skin, striae, or proximal myopathy. Clinical examination suggested a pretest probability of CS to be moderate.
INVESTIGATIONS
The baseline laboratory test results are shown in Table 54.1 . The serum cortisol concentrations were increased and lacked diurnal variation. The 24-hour urine free cortisol excretion and the
| Biochemical Test | Result | Reference Range |
| 8 am serum cortisol, mcg/dL | 15 | 7–25 |
4 pm serum cortisol, mcg/dL | 12 | 2–14 |
1-mg overnight DST cortisol mcg/dL | 18 | <1.8 |
24-Hour UFC, mcg | 138 | <45 |
Late night salivary cortisol, ng/dL | 78 | ≤100 |
ACTH, pg/mL | 53 | 10–60 |
DHEA-S, mcg/dL | 246 | 31–228 |
Prolactin, ng/mL | 15.7 | 3–27 |
IGF1, ng/mL | 240 | 59–279 |
Free thyroxine, ng/dL | 1.2 | 09–1.7 |
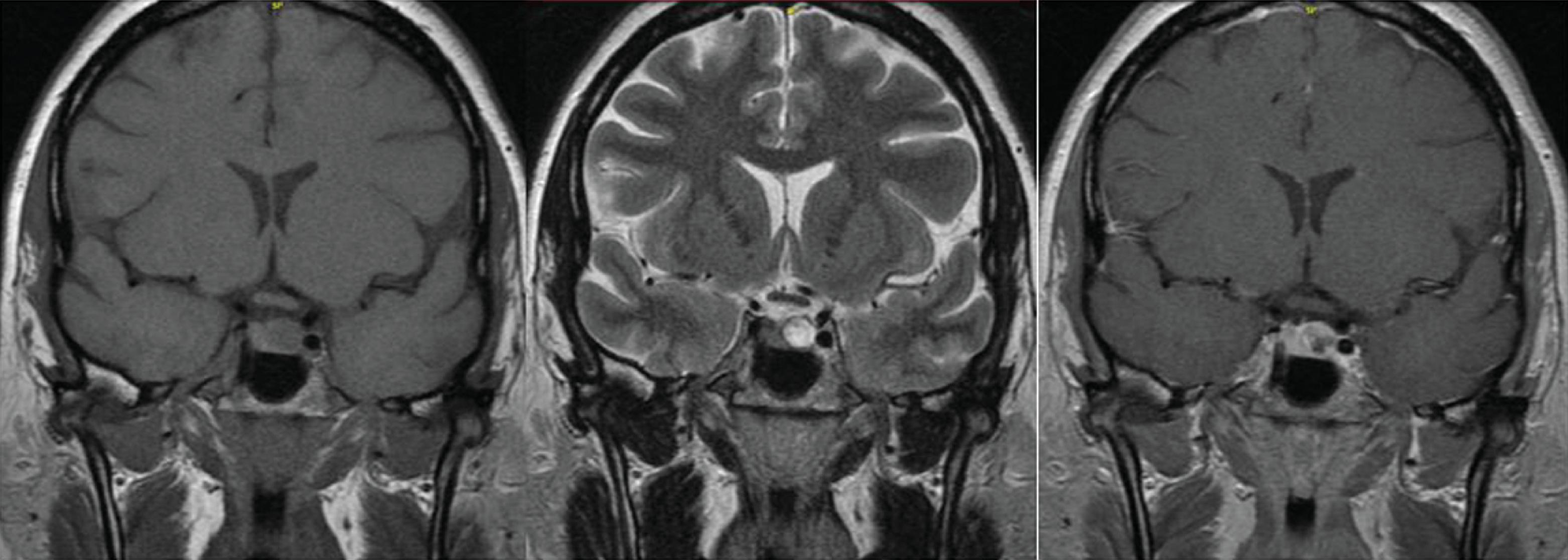
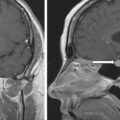
1-mg overnight dexamethasone suppression test (DST) were abnormal, while the late-night salivary cortisol concentration was within normal ranges. The laboratory profile, in conjunction with the clinical presentation, confirmed ACTH-dependent CS. Workup for pituitary dysfunction otherwise was negative. Head MRI showed an 8 × 10 × 7–mm pituitary adenoma in the left aspect of pituitary gland ( Fig. 54.1 ).