Contralateral Prophylactic Mastectomy
Todd M. Tuttle
INTRODUCTION
Patients with unilateral breast cancer are at increased risk for developing cancer in the contralateral breast. As a result, some patients choose contralateral prophylactic mastectomy (CPM) to prevent cancer in the contralateral breast. Several studies have reported that the CPM rates have markedly increased in recent years in the United States. In this chapter, we will discuss recent CPM trends, potential reasons patients choose CPM, outcomes after CPM, and alternative strategies for managing the increased risk of contralateral breast cancer among survivors of unilateral breast cancer.
CPM TRENDS
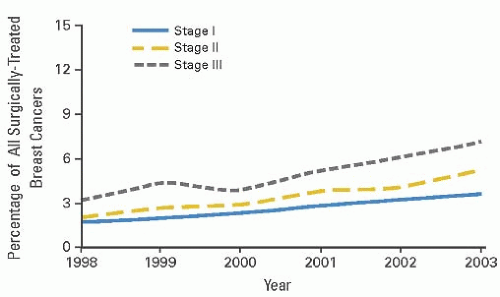
Contralateral prophylactic mastectomy is the removal of the normal intact breast among women with unilateral breast cancer. The Surveillance Epidemiology and End Results (SEER) registry began coding CPM in 1998. At that time, the proportion of patients who underwent CPM in the United States was very low (1). However, the CPM rate among all surgically treated patients with invasive breast cancer increased 150% from 1998 to 2003 in the United States (Fig. 34-1). Among mastectomy patients, the CPM rate increased 162% from 1998 to 2003 (Fig. 34-2). These trends were observed for all cancer stages and continued to increase at the end of the study period with no plateau. Among the SEER registries, Atlanta had the highest CPM rates, while Connecticut had the lowest rates. Although significant geographic variations were observed between different SEER registries, no general geographic trends were identified. Similar findings were observed in the SEER database among patients with ductal carcinoma in situ (DCIS) (2).
Other studies using different databases have confirmed these findings. Using the American College of Surgeons’ National Cancer Data Base (NCDB), Yao et al. reported similar increases in CPM rates from 1998 to 2007; by 2007, the rates were still increasing with no plateau effect (3). In a study using the New York State Cancer Registry, McLaughlin et al. reported that CPM use more than doubled from 1995 to 2005 (4). Single-institutional studies have also demonstrated marked increases in CPM rates (5, 6 and 7).
In contrast, similar trends have not been observed in Europe. In a single-center study from Switzerland, Güth et al. reported that the CPM rates at an academic surgery center did not increase from 1995 to 2009 (8). The authors concluded that the increased use of CPM was a “trend made in the USA.” Another study supports this viewpoint. In an international registry of women with unilateral breast cancer and BRCA mutation, Metcalfe et al. reported that 49% of women in the United States underwent CPM (9). In contrast, the CPM rates for Europe and Israel were only about 10% or less.
Various patient, tumor, and treatment factors are significantly associated with CPM rates (see Table 34-1). Younger women are much more likely to receive CPM (1, 3). White race, higher education level, private health insurance, and family history of breast cancer have also been associated with higher CPM rates (1, 3, 5, 7). In the SEER study, the presence of infiltrating lobular histology was one of the strongest predictors of CPM (1). Yet, population-based studies indicate that the risk of contralateral breast cancer is not significantly increased for infiltrating lobular histology as compared with infiltrating ductal histology (10). Multicentric breast cancer has also been associated with higher CPM rates (11). BRCA testing is significantly associated with CPM, even among patients who do not have BRCA mutations. In one singlecenter study, the CPM rate was 40% among those patients who tested negative for mutations (12). Several studies have reported that preoperative MRI is associated with CPM (5, 7, 11). Patients treated at comprehensive cancer programs or teaching facilities are more likely to receive CPM (3).
REASONS FOR INCREASED CPM RATES
This trend towards more aggressive breast cancer surgery is curious and counterintuitive in the modern era of minimally invasive surgery. The following section of this chapter is largely speculative because the exact reasons for increased CPM rates in the United States are unknown. However, many factors probably contribute to increased CPM use. Public awareness of genetic breast cancer and increased BRCA testing may partially explain these observations. Improvements in mastectomy (including skin-sparing and nipple-sparing mastectomy) and reconstruction techniques and access to breast reconstruction probably contribute to increased CPM rates.
Moreover, symmetric reconstruction is often easier to achieve after bilateral mastectomy as compared to unilateral mastectomy. Additionally, the native and reconstructed breast age differently, so symmetric outcomes may diminish over time.
Moreover, symmetric reconstruction is often easier to achieve after bilateral mastectomy as compared to unilateral mastectomy. Additionally, the native and reconstructed breast age differently, so symmetric outcomes may diminish over time.
Several studies have reported that preoperative breast MRI is associated with higher CPM rates (5, 7). The proposed explanation is that MRI findings introduce concern about the opposite breast. For example, a patient is diagnosed with a unilateral breast cancer, and clinical breast examination and mammography of the contralateral breast are normal. The patient is an ideal candidate for breast-conserving treatment. However, an MRI is obtained which demonstrates an occult indeterminate lesion in the contralateral breast. Next, the patient undergoes a second-look (targeted) ultrasound to characterize this MRI finding. The ultrasound imaging is normal, so she gets called back again for an MRI-guided biopsy, which is negative for cancer. However, the patient decides to have bilateral mastectomy to avoid this stressful scenario again. Preoperative breast MRI probably contributes to increased CPM rates, but the initial observed CPM trends in the United States preceded the widespread use of breast MRI (1, 3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree