The rectum begins where the large bowel loses its mesentery, at the level of the body of the third sacral vertebra.
Peritoneum covers the upper portion laterally and anteriorly near its junction with the sigmoid colon and only anteriorly near the peritoneal reflection. The peritoneum is reflected anteriorly onto the seminal vesicles and bladder in males and onto the upper vagina and uterus in females, leaving the lower half of the rectum without a peritoneal covering.
Three transverse folds, two on the left and one on the right, divide the rectum topographically into thirds. The middle transverse fold, approximately 11 cm from the anal verge, provides a landmark for the peritoneal reflection.
The portion below the middle valve is the rectal ampulla; if it is resected, stool frequency is often increased markedly (important to consider when choosing between a “radical” sphinctersparing procedure, such as coloanal anastomosis, or a “conservative” sphincter-sparing procedure, such as endocavitary irradiation).
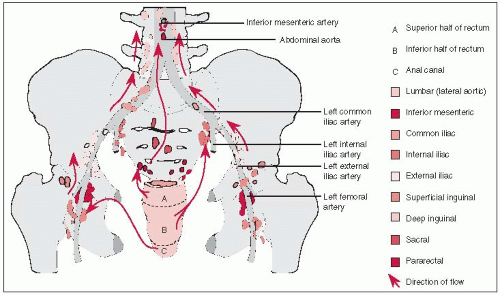
Lymphatic drainage follows the superior rectal vessels, which empty into the inferior mesenteric nodes.
Lymphatic drainage of the middle and lower rectum also occurs along the middle rectal vessels, terminating in the internal iliac nodes.
The lowest part of the rectum and upper part of the anal canal share a plexus that drains to the lymphatics that accompany the inferior rectal and internal pudendal blood vessels and ultimately drain to the internal iliac nodes.
Ascending and descending colon and splenic and hepatic flexures lack mesentery and are immobile because of their retroperitoneal location.
Cecum lacks a true mesentery but may have some mobility because of short folds of peritoneum that are variably present.
Lymphatic drainage follows the inferior mesenteric vessels for left colon and superior mesenteric vessels for right colon.
If tumor involves adjacent organs in the true or false pelvis, iliac nodes may be at risk.
Periaortic lymph nodes may be at risk when cancer invades the retroperitoneum.
Discontinuous spread of colon and rectal cancer occurs by peritoneal seeding, lymphatic pread, hematogenous spread, and surgical implantation.
Peritoneal spread is rare in rectal cancer because most of the rectum is below the peritoneal reflection.
Extension within the bowel usually occurs only for short distances.
Primary venous and lymphatic channels originate in submucosal layers of bowel; cancers limited to the mucosa are at little risk for dissemination.
Lymph node involvement occurs in nearly 50% of patients with deeper tumors.
Skip metastasis or retrograde spread occurs in 1% to 3% of node-positive patients and is thought to be due to lymphatic blockage.
Hematochezia is the most common presenting feature in rectal and lower sigmoid cancer.
Abdominal pain is common in patients with colon cancer.
Other presenting symptoms include change in bowel habit, nausea, vomiting, anemia, or abdominal mass.
Diagnostic procedures include detailed history, physical examination, and endoscopic, radiographic, and laboratory studies (Table 28-1).
In patients with rectal cancer, a digital rectal examination and an endoscopy are mandatory.
For colon and rectal tumors, attention should be paid to palpation of any extrarectal mass that may suggest peritoneal spread.
TABLE 28-1 Diagnostic Workup for Colorectal Cancer
General
History
Physical examination, including detailed rectal examination
Pelvic examination (female patients)
Radiographic and Endoscopic Studies
Barium enema or colonoscopy
Proctosigmoidoscopy (if colonoscopy not done)
Chest radiography
Computed tomography or magnetic resonance imaging (pelvis, abdomen, if indicated)
Intrarectal ultrasound (if indicated)
Routine Laboratory Studies
Complete blood cell count
Blood chemistry profile, including liver and renal function studies
Carcinoembryonic antigen
Molecular biologic markers
Source: From Martenson JA Jr, Gunderson LL. Colon and rectum. In: Perez CA, Brady LW, eds. Principles and practice of radiation oncology, 3rd ed. Philadelphia, PA: Lippincott-Raven, 1998:1489-1510, with permission.
In women, a complete pelvic examination, including rectovaginal examination, is mandatory.
Potential areas of metastatic spread, including inguinal lymph nodes (particularly with rectal lesions near the dentate line), supraclavicular lymph nodes, liver, abdominal mass, or ascites, should be evaluated.
Barium enema and proctosigmoidoscopy or colonoscopy should be performed to rule out second primary large bowel cancers and to biopsy any suspicious lesions.
For rectal cancer, barium enema performed before resection, including a crosstable lateral view, can assist greatly in planning radiation therapy.
Intrarectal ultrasonography is useful in determining if lesions are limited to the bowel wall and therefore amenable to sphincter-preservation techniques such as local excision or endocavitary irradiation and to assess lymph node involvement.
If liver and renal function studies are abnormal, computed tomography scan or ultrasonography is indicated.
Preoperative carcinoembryonic antigen (CEA) value is an independent prognostic factor in large bowel cancer; serial measurement postoperatively is used to identify disease progression in asymptomatic patients.
Dukes described a staging system based on extent of disease penetration through the bowel wall and presence or absence of nodal metastasis (5).
The Astler-Coller staging system allows specification of both tumor penetration and nodal involvement; its modification also permits specification of tumor adherence to surrounding organ structures (Table 28-2) (2, 29).
The Dukes, Astler-Coller, and modified Astler-Coller systems are postoperative pathologic staging systems and cannot be used preoperatively.
The tumor-node-metastasis system of the American Joint Committee on Cancer can be used as a clinical (preoperative) or postoperative pathologic staging system (Table 28-2) (1).
TABLE 28-2 AJCC Staging Categories for Colon and Rectal Cancer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||