CLOMIPHENE CITRATE
Part of “CHAPTER 97 – OVULATION INDUCTION“
Clomiphene citrate, which was introduced in 1956, was first observed to achieve conception in humans in 1961.9 It is used primarily in women with chronic anovulation secondary to PCOS or with a luteal-phase defect, or to induce superovulation in eumenorrheic women with infertility. Clomiphene citrate is produced as a racemic mixture of two isomers: trans (62%) and cis (38%). The cis form is probably the one responsible for ovulation induction. Although it is available in a lower dose as a separate ovulation induction agent, no comparisons have been made between cis-clomiphene citrate and the commonly used racemic version.
Clomiphene has prolonged estrogen-receptor binding, with a plasma half-life of 5 to 7 days; indeed, it has been recovered in feces up to 6 weeks after discontinuation of treatment.10 This binding to the estrogen receptor produces both antagonistic and agonistic effects. The first effect noted after the administration of clomiphene is an elevation in gonadotropin secretion that has been attributed to an antagonistic effect of this drug on the estrogen receptors in the hypothalamus. Clomiphene may also have a direct effect on the pituitary and ovary, both to enhance gonadotropin secretion and to induce aromatase activity synergistically with FSH. No stimulation of the cortisol, androgen, or progesterone receptor is noted.
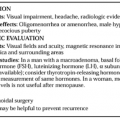
INDICATIONS FOR TREATMENT
The primary indication for clomiphene treatment is for induction of ovulation in the estrogenized, anovulatory woman, who usually has a history of reproductive dysfunction since puberty. Most of these women have PCOS, which includes symptoms of oligomenorrhea and hirsutism. In this group, FSH levels will increase to stimulate follicular development and ovulation in 70% of patients 5 to 10 days after taking the last dose.
Clomiphene is administered after a spontaneous menses or a progestin-induced withdrawal bleed. It is usually prescribed for 5 days starting between cycle days 2 and 5. The drug should be started early in the follicular phase to assure adequate follicular recruitment.
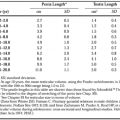
The starting dose of clomiphene for the majority of patients is 50 mg, but a dose of 25 mg may be considered for patients of lower body weight or a dose of 75 to 100 mg for obese patients. If no ovulatory response is noted, the dose should be increased by 25 to 50 mg during the next cycle, to a maximum dose of 250 mg. These doses are higher than those either approved or recommended by the FDA, but are consistent with clinical usage and experience. The lowest dose that causes ovulation should be used, because higher doses may have an antiestrogenic effect on the endometrial lining (preventing thickening) that may impede implantation. Follicular development may be monitored with the use of transabdominal or transvaginal ultrasonography. When the leading follicle (i.e., the largest) reaches a diameter of 17 to 20 mm, it is considered to be mature and close to ovulating. Although an increase in pregnancy rates has been noted when ultrasonography was used in cycle monitoring, its routine use is probably not cost effective.11 Human chorionic gonadotropin (hCG) (10,000–20,000 IU intramuscularly) can be given to women with a mature follicle on ultrasonography, because it allows better cycle control and more precise timing of intercourse or the performance of inseminations. If ultrasonography is not used, intercourse should be initiated every other day starting 3 days after the last clomiphene dose, or it can be timed with a urinary LH surge detection kit. Some kits may give false-positive readings, however, even during clomiphene ingestion, because of the increase in gonadotropin secretion that clomiphene may cause.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree