Although initially designed for treatment of patients with metastatic cancers, drugs are now used at some time point during the course of the illness of most cancer patients. Cytotoxic drugs cure some disseminated cancers (
Table 1-3) and are effective in decreasing tumor volume, alleviating symptoms, and even prolonging life in many other types of metastatic cancer that are not curable.
Adjuvant chemotherapy regimens are used in patients who have had primary tumors resected and who, although possibly cured by surgery, are at significant risk of recurrence. Adjuvant therapy decreases tumor recurrence rates and prolongs survival in selected patients with breast cancer, colorectal cancer, non-small cell lung cancer, osteosarcoma, and other tumors.
Neoadjuvant chemotherapy effectively reduces the bulk of primary tumors prior to surgical resection or irradiation of tumors that would otherwise be difficult or impossible to resect. It is often used in patients with locally advanced head and neck carcinomas, esophageal cancer, non-small cell lung cancer, osteosarcoma and soft tissue sarcomas, bladder cancer, and breast cancer. This approach often allows a more limited surgical operation, or even surgery-sparing radiation therapy, and thereby preserves organ function and minimizes cosmetic changes. It also may decrease local recurrence and the initial clinical response of the tumor mass can serve as an indication of tumor sensitivity to the drugs used, and therefore a signal to continue chemotherapy after surgery.
The design of multi-drug treatment regimens is based on a number of considerations. These include (a) the kinetics of tumor growth, (b) responsiveness of the pathologic and molecular type of tumor to specific drugs, (c) the biochemical mechanisms of each drug’s cytotoxic activity as well as their mechanisms of resistance, and (d) the pharmacokinetic behavior of drugs in question and their patterns of toxicity to normal organs. Some chemotherapy regimens have been designed to minimize emergence of drug resistance, based on preclinical experiments or theoretical models of drug resistance. The molecular actions and pharmacokinetic features of individual drugs are considered in detail in succeeding chapters, but the impact of these factors on trial design is reviewed at this juncture to provide a framework for understanding regimen design.
Kinetic Basis of Drug Therapy
The objective of cancer treatment is to reduce the tumor cell population to zero. Chemotherapy experiments with rapidly growing transplanted tumors in mice have established the validity of the
fractional cell kill hypothesis, as developed by Skipper et al.,
8 which states that a given drug concentration applied for a defined time period will kill a constant fraction of the cell population, independent of the absolute number of cells. Regrowth of tumor occurs during the drug-free interval between cycles. Thus, each treatment cycle kills a specific fraction of the remaining cells. Assuming that drug-resistant cells do not outgrow, the results of treatment are a function of (a) the dose of drug administered and (b) the number and frequency of repetitions of treatment.
Based on these cytokinetic considerations, most chemotherapy regimens consist of cycles of intensive therapy repeated as frequently as allowed by the tolerance of dose-limiting tissues, such as bone marrow or gastrointestinal tract. The object of these cycles is to reduce the absolute number of remaining tumor cells to 0 (or <1) through the multiplicative effect of successive fractional cell kills (e.g., given 99% cell kill per cycle, a tumor burden of 1011 cells will be reduced to <1 cell with six cycles of treatment: [1011 cells] × [0.01]6 < 1).
The fractional cell kill hypothesis was derived from studies of the treatment of murine leukemias, and was applied successfully to the cure of human leukemia and lymphoma. For more slowly growing solid tumors in humans, a number of confounding factors distort the fundamental assumption of constant fractional cell kill per cycle with. Most solid tumors (such as lung and colon cancers) are recognized at a stage of decelerating growth, when tumor vascularity is not adequate to provide oxygen and nutrients to the bulk of the tumor. These large tumors contain a high fraction of slowly dividing or noncycling cells (termed “G0 cells”). Most antineoplastic agents, particularly the antimetabolites and antitumor antibiotics, are effective against rapidly dividing cells. Some selectively kill cells during specific phases of the cell cycle (S-phase, for cytosine arabinoside, and mitosis, for the vincas and taxanes). The initial kinetic features of a large, poorly vascularized, and slowly growing tumor are unfavorable for treatment with these drugs. However, alkylators and adduct-forming platinum derivatives attack DNA in all phases of the cell cycle, and retain activity against nondividing or slowly dividing cells. Thus, they are often used to reduce tumor bulk. An initial reduction in cell numbers produced by surgery, radiotherapy, or non-cell-cycle-specific drugs may indirectly improve blood flow and thereby push the slowly dividing cells into more rapid cell division. A reduction in tumor volume may recruit nondividing cells into the cell cycle, where they become increasingly susceptible to therapy with cell-cycle-specific agents. Thus, an initially slowly responding tumor may become more responsive to antimetabolites or antimitotic drugs after surgical debulking or after initial treatment with alkylators, and fractional cell kill may actually increase with sequential courses of treatment.
The biochemical and molecular heterogeneity of advanced human tumors introduces additional complexity to the simple hypothesis that multiple cycles of fractional cell kill translate into tumor cure. Isoenzyme typing, karyotypic analysis, and molecular studies have demonstrated that most human tumors evolve from a single malignant cell.
9 This original homogeneity does not persist during later stages of tumor growth; in fact, studies of human tumors disclose that clinically evident malignancies are composed of cell types with differing molecular, biochemical, morphologic, and drug-response characteristics. This heterogeneity results from the genomic instability of malignant cells. Indeed, mutations in cell-cycle checkpoint control genes, such as
p53, and in DNA repair genes, such as the
MSH genes in familial colon cancer, may be the initial event in malignant transformation of many tumor types, establishing a fundamentally mutable clone from which diverse subclones evolve. Thus, spontaneous amplifications, deletions, or other alterations affect a broad expanse of genes in tumors, some of which affect the target proteins that control drug response and cell cycle.
10 These mutations lead to heterogeneity and account for outgrowth of resistant tumor cells during or after treatment. This has been clearly demonstrated in the pretreatment isolation of imatinib (gleevec)-resistant cells from selected patients with chronic myelogenous leukemia.
11 When a diverse population of tumor cells are subjected to the selective pressure of drug treatment, drug-sensitive tumor cells are destroyed, but subpopulations of resistant cells survive and proliferate. With some notable exceptions (treatment of chronic myelogenous leukemia with imatinib, gestational choriocarcinoma treated with methotrexate, cyclophosphamide treatment for African Burkitt’s lymphoma, and cladribine treatment for hairy cell leukemia), single-agent chemotherapy rarely produces long-term remission or cure of advanced malignancies. Of necessity, the most successful treatment regimens have combined multiple agents with different mechanisms of action.
A second possible reason for failure of chemotherapy is the existence of stem cell populations within the tumor; these cells possess a multidrug-resistant phenotype and the capacity of unlimited self-renewal.
12 It is postulated, but still unproven, that failure of therapy may result from the persistence of tumor stem cells following eradication of the more drug-sensitive and more differentiated bulk of the tumor population.
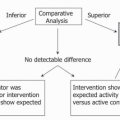
Prediction of Drug Response to Individual Agents
The results of clinical trials set the standard for treatment of most types of cancer, but for most metastatic cancers, only a fraction of patients respond, and those responses are temporary. To avoid the needless toxicity of ineffective treatment, especially in diseases with only modest rates of response, it would be desirable to predict sensitivity for the specific tumor and patient at hand. Various systems have been established and some even commercialized for testing tumor cells in vitro to predict response to a panel of candidate drugs, but only fragmentary evidence, and no prospective controlled trial data, exist to justify their routine use.
Biochemical and molecular tests for drug sensitivity have proven predictive value in the practice of oncology; these include tests for hormone receptor protein expression and
HER-2-neu amplification in breast cancer, the mutational status of k-Ras in colorectal cancer, and most recently the test for mutational activation of the EGFR receptor in non-small cell lung cancer (see relevant chapters). The results of each of these tests are highly correlated with clinical responsiveness to specific therapies. Other tests offer promise for clinical use. Expression of components of the DNA repair pathway correlates with patient survival after platinum-based treatment.
13 Similarly, high concentrations of dihydrofolate reductase have
been associated with resistance to methotrexate,
14 as is a failure to transport or polyglutamate the drug.
15 High intratumoral levels of the DNA repair enzyme methylguanine methyl transferase predict resistance to nitrosoureas, dacarbazine, and temozolomide, all of which damage DNA by alkylating the
O6 position of guanine.
16 Mutations in mismatch DNA repair (the
MSH6 gene) are associated with resistance to methylating agents, to 6-mercaptopurine, and to cisplatin and carboplatin.
17 However, these molecular/biochemical tests have not been tested prospectively to prove their value in selecting treatment with cytotoxic drugs, and routine laboratory tests are not available.
Molecularly targeted discovery offers the hope of identifying new drugs tailored to specific receptors and intracellular enzymes critical for cell signaling and for maintaining viability and growth of tumors. Targeted drugs are effective against subsets of human malignancy. One such target, the
bcr-abl tyrosine kinase, results from a translocation specific for chronic myelogenous leukemia (CML), and virtually all CML patients have this translocation at diagnosis. Imatinib, an inhibitor of the kinase, has striking activity in chronic and blastic phases of CML, and has limited toxicity for normal bone marrow cells.
18 Because imatinib also inhibits the
c-kit tyrosine kinase, it is effective against gastrointestinal stromal tumors (GIST). Most patients with GIST express a mutated and activated form of
c-kit. Pretreatment sequencing of the
c-kit gene provides important prognostic information and allows appropriate selection of patients for treatment with imatinib (exon 11 mutations), sunitinib (exon 9 mutations), or other experimental drugs.
19Genetic tests to select patients for specific targeted therapies may dramatically improve response rates to these drugs. Activating mutations in the EGFR gene identify non-small cell lung cancer (NSCLC) patients who have a 70% response rate to gefitinib as first line therapy. Tumors lacking such mutations do not show clinical tumor regression, although some may derive benefit from a slowing of their growth.
20 The test for EGFR mutations should be performed in any nonsmoking patient with unresectable NSCLC.