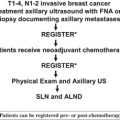
Since its introduction in the mid-1990s, sentinel lymph node (SLN) biopsy has revolutionized the management of breast cancer patients, allowing for a minimally invasive method to accurately stage the axilla without the need for axillary lymph node dissection and its concomitant morbidity in node-negative patients. The ability to identify the lymph nodes most likely to harbor metastases has allowed for increased scrutiny of these lymph nodes, often finding minimal disease in the SLNs. The relevance of such minute disease has been controversial, and there has been considerable debate as to how best to manage such patients.
Since its introduction in the mid-1990s, sentinel lymph node (SLN) biopsy has revolutionized the management of breast cancer patients, allowing for a minimally invasive method to accurately stage the axilla without the need for axillary lymph node dissection (ALND) and its concomitant morbidity in node-negative patients. The ability to identify the lymph nodes most likely to harbor metastases has allowed for increased scrutiny of these lymph nodes, often finding minimal disease in the SLNs. The relevance of such minute disease has been controversial, and there has been considerable debate as to how best to manage such patients.
What constitutes a positive sentinel lymph node?
SLNs are frequently subjected to increased pathologic scrutiny, often involving serial sectioning, the use of immunohistochemistry (IHC), and molecular techniques using polymerase chain reaction (PCR). Such careful evaluation has led to an upstaging of patients who may have been found to be node negative on routine histopathologic examination. Several studies have found that up to a third of patients may be found to have SLN metastases when their SLNs are subjected to more intensive examination ( Table 1 ). When investigators re-examined ALND specimens of patients in older studies, such as the Ludwig Trial V, using serial sectioning and IHC, they found micrometastases in 7% to 9% of patients who had previously been categorized as node negative. Further, these patients had a significantly worse overall and disease-free survival than those who were truly node negative. Although hematoxylin-eosin (H&E) staining remains the gold standard for detecting metastases, many pathologists continue to use IHC in the evaluation of SLNs. The Association of Directors of Anatomic and Surgical Pathology recommends that the results of IHC should be evaluated in the context of routine histopathology.
| Study | No. of Patients | Technique | No. Upstaged (%) |
|---|---|---|---|
| Inokuchi (2003) | 342 | IHC | 5 (2) |
| Mullenix (2005) | 183 | IHC | 8 (4) |
| Wong (2001) | 869 | IHC | 58 (7) |
| Schreiber (1999) | 210 | IHC | 17 (9) |
| Pendas (1999) | 385 | IHC | 41 (11) |
| McIntosh (1999) | 52 | IHC | 8 (14) |
| Ryden (2007) | 132 | IHC/SS | 3 (2) |
| Weaver (2000) | 489 | IHC/SS | 20 (4) |
| Pargaonkar (2003) | 64 | IHC/SS | 5 (8) |
| Weaver (2009) | 54 | IHC/SS | 5 (9) |
| Stitzenberg (2002) | 55 | IHC/SS | 7 (13) |
| Yared (2002) | 96 | IHC/SS | 19 (20) |
| Inokuchi (2003) | 342 | RT-PCR | 31 (9) |
| Sakaguchi (2003) | 80 | RT-PCR | 13 (16) |
| Manzotti (2001) | 117 | RT-PCR | 23 (20) |
| Gillanders (2004) | 344 | RT-PCR | 112 (33) |
Although the modality used to detect nodal metastases should be recorded, the seventh edition of the American Joint Committee on Cancer staging system uses the size of the tumor deposit to determine lymph node positivity. Tumor deposits should be measured as the largest dimension of any group of contiguous cells, regardless of whether or not they are confined to the node. Tumor deposits less than 0.2 mm are considered isolated tumor cells (ITCs) of unknown biologic significance (ie, node negative). Tumor deposits measuring 0.2 to 2.0 mm or those containing more than 200 individual tumor cells in a single node section are considered micrometastases (N1[mic]) (ie, node positive).
Although the prognostic impact of ITCs and micrometastasis is the subject of the American College of Surgeons Oncology Group (ACOSOG) Z-0010 trial and the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-32 trial, other studies have provided some insight into their relevance. For example, in a multicenter study of 1259 patients with a mean follow-up of 4.9 years, distant recurrence rates were significantly different between SLN-negative patients (6%) and those with ITCs (8%), micrometastases (14%), and macrometastases (21%). Similarly, a study from Memorial Sloan-Kettering in which ALND specimens of 368 patients treated between 1976 and 1978 were evaluated with serial section and IHC found that 17 patients (5%) were found to have micrometastases and 5 patients (1%) were found to have macrometastases. The finding of these deposits was associated with a significantly worse disease-free survival than those who were truly node negative.
Several studies have assessed the incidence of finding non-SLN metastases in the setting of ITCs and micrometastases ( Table 2 ). A meta-analysis demonstrated that in patients with SLN micrometastasis, approximately 20% would have nonsentinel metastasis. Therefore, micrometastases constitute node-positive disease, and completion ALND is currently recommended. Patients with ITCs or clusters measuring less than 0.2 mm, however, are considered node negative and no further axillary surgery is required. In a recent survey of American Society of Clinical Oncology members, the finding of micrometastases were found to “always” or “sometimes” influence clinical decisions in 54.7% and 43.8% of respondents, respectively, whereas 52.9% stated that ITCs never had an impact. Only 22.1% of respondents stated, however, they would “always” recommend an ALND for micrometastases, whereas 73% stated they would recommend it “sometimes.” Factors influencing this decision included primary tumor size, patient age, tumor grade, lymphovascular invasion, and size of the metastasis.
| Study | No. of SLN + Patients | ITC/Micrometastases | No. of NSLN Positive (%) |
|---|---|---|---|
| Cserni (2007) | 26 | ITC | 0 (0) |
| Calhoun (2005) | 61 | ITC | 3 (4.9) |
| Van Rijk (2006) | 54 | ITC | 4 (7.4) |
| Schrenk (2005) | 44 | ITC | 4 (9.1) |
| Van Deurzen (2007) | 23 | ITC | 3 (13.0) |
| Viale (2005) | 116 | ITC | 17 (15.8) |
| Houvenaeghel (2006) | 187 | ITC | 30 (16.0) |
| Menes (2005) | 31 | ITC | 6 (19.4) |
| Fournier (2004) | 16 | ITC/micrometastasis | 1 (6.3) |
| Nos (2003) | 123 | ITC/micrometastasis | 8 (6.5) |
| Yu (2005) | 70 | ITC/micrometastasis | 5 (7.1) |
| van Iterson (2003) | 54 | ITC/micrometastasis | 6 (11.1) |
| Hung (2005) | 24 | ITC/micrometastasis | 4 (16.7) |
| Fleming (2004) | 16 | ITC/micrometastasis | 3 (18.8) |
| Mignotte (2002) | 68 | ITC/micrometastasis | 15 (22.1) |
| den Bakker (2002) | 32 | ITC/micrometastasis | 11 (34.4) |
| Rutledge (2005) | 29 | Micrometastasis | 1 (3.4) |
| Zgajnar (2005) | 36 | Micrometastasis | 4 (11.1) |
| Gipponi (2006) | 116 | Micrometastasis | 16 (13.8) |
| Houvenaeghel (2006) | 301 | Micrometastasis | 43 (14.3) |
| Fink (2008) | 12 | Micrometastasis | 2 (16.7) |
| Chagpar (2005) | 84 | Micrometastasis | 15 (17.9) |
| Van Deurzen (2007) | 101 | Micrometastasis | 20 (19.8) |
| Reynolds (1999) | 27 | Micrometastasis | 6 (22.2) |
| Schrenk (2005) | 78 | Micrometastasis | 78 (23.1) |
| Leidenius (2005) | 84 | Micrometastasis | 22 (26.2) |
| Li (2007) | 68 | Micrometastasis | 18 (26.4) |
| Menes (2005) | 30 | Micrometastasis | 6 (20.0) |
| Viale (2005) | 318 | Micrometastasis | 68 (21.3) |
| Cserni (2004) | 32 | Micrometastasis | 8 (33.3) |
Treatment of sentinel node positive disease: the need for ALND?
Although controversial, there is little evidence that ALND improves survival. The 25-year follow-up from the landmark NSABP B-04 trial showed no difference in survival for patients who received elective ALND compared with those who did not. Nonetheless, ALND provides excellent local control. Many patients with SLN metastases have no further disease in the axilla ( Table 3 ), thus raising the question of whether or not ALND is needed in all SLN-positive patients. The University of Louisville Breast Sentinel Node Study, a multicenter prospective trial of 4131 patients, found that 63.1% of SLN-positive patients had disease limited to the sentinel nodes. ALND is associated with significant morbidity, including numbness, swelling, and decreased range of motion of the shoulder. Therefore, there has been considerable interest in identifying a subset of SLN-positive patients in whom the risk of non-SLN metastases is so low that ALND may be avoided.
| Study | No. of Patients | % Patients with No Non-SLN Metastases |
|---|---|---|
| Yu et al (2005) | 286 | 34.3 |
| Viale (2005) | 794 | 49.7 |
| van Deurzen (2007) | 193 | 51.8 |
| Degnim et al (2005) | 574 | 58.3 |
| Soni et al (2005) | 149 | 58.4 |
| Cserni et al (2004) | 150 | 60.0 |
| Kocsis et al (2004) | 140 | 61.0 |
| Van Zee et al (2003) | 1075 | 61.1 |
| Schrenk et al (2005) | 379 | 62.3 |
| van Iterson et al (2003) | 135 | 66.0 |
| Nos et al (2003) | 263 | 76.0 |
| Houvenaeghel (2009) | 490 | 84.9 |
| Houvenaeghel (2006) | 301 | 85.7 |
Another reason to advocate that all patients with a positive SLN should undergo completion ALND is to obtain accurate staging information that may affect adjuvant therapy decisions. Although it may be argued that contemporary use of systemic therapy is often guided by primary tumor information and that the absolute number of total lymph nodes involved may be of little consequence to therapy decisions, others may find information, in particular regarding lymph node ratio, to affect their decision making. Furthermore, the number of positive nodes may affect decisions regarding postmastectomy radiation therapy (PMRT). Although the American Society of Clinical Oncology and the American Society of Therapeutic Radiology and Oncology continue to recommend PMRT in the setting of 4 or more positive nodes, more recent data suggest that PMRT may be of benefit even in the 1 to 3 node-positive group. Proponents of treating all node-positive patients with PMRT on the basis of these data may argue, therefore, that information obtained from completion ALND will not affect their management.
Finally, accurate staging is dependent on the absolute number of positive nodes and provides prognostic information. ALND has not been found to adversely affect long-term quality of life and, therefore, remains standard of care after a positive SLN biopsy.
Treatment of sentinel node positive disease: the need for ALND?
Although controversial, there is little evidence that ALND improves survival. The 25-year follow-up from the landmark NSABP B-04 trial showed no difference in survival for patients who received elective ALND compared with those who did not. Nonetheless, ALND provides excellent local control. Many patients with SLN metastases have no further disease in the axilla ( Table 3 ), thus raising the question of whether or not ALND is needed in all SLN-positive patients. The University of Louisville Breast Sentinel Node Study, a multicenter prospective trial of 4131 patients, found that 63.1% of SLN-positive patients had disease limited to the sentinel nodes. ALND is associated with significant morbidity, including numbness, swelling, and decreased range of motion of the shoulder. Therefore, there has been considerable interest in identifying a subset of SLN-positive patients in whom the risk of non-SLN metastases is so low that ALND may be avoided.