CLINICAL MANIFESTATIONS
Part of “CHAPTER 58 – PRIMARY HYPERPARATHYROIDISM“
The signs and symptoms of primary hyperparathyroidism result from the hypercalcemia (see Chap. 59) and the hyperparathyroid state. In primary hyperparathyroidism, the classic target organs are the bones and the kidneys.
BONE DISEASE
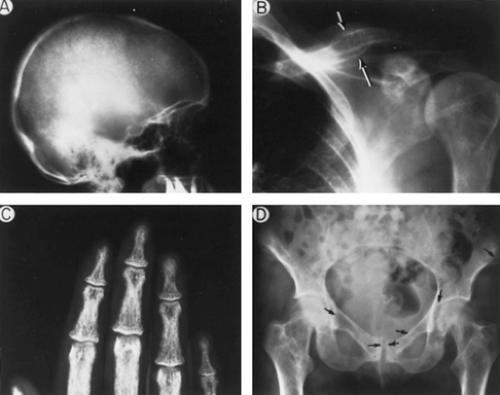
In classic primary hyperparathyroidism, the skeleton is involved in a process known as osteitis fibrosa cystica.30 Radiographically, subperiosteal bone resorption is seen in several typical sites (Fig. 58-1). The salt-and-pepper appearance of the skull, resorption of the distal phalanges, and tapering of the distal clavicles are classic features of the resorptive process in bone. Bone cysts and brown tumors also may be seen. Brown tumors are collections of osteoclasts intermixed with poorly mineralized woven bone. Another important radiologic feature of hyperparathyroid bone disease is demineralization caused by prolonged bone resorption. Osteopenia alone may be a radiographic characteristic of primary hyperparathyroidism. The differential diagnosis of osteoporosis should always include an evaluation for primary hyperparathyroidism.
Before the widespread use of the multichannel autoanalyzer in the early 1970s, the incidence of radiologically apparent bone disease in hyperparathyroidism was 10% to 15%. This figure is now much lower (<5%) because of the markedly higher detection of asymptomatic primary hyperparathyroidism in patients. Although grossly evident bone disease is no longer a frequent finding in primary hyperparathyroidism, more sophisticated diagnostic testing shows continued involvement of the skeleton in the hyperparathyroidism. Bone mineral densitometry and quantitative bone histomorphometry, for example, have detected evidence for hyperparathyroidism among patients without otherwise apparent hyperparathyroid bone disease.30 The changes are seen at cortical bone, which is found predominantly in the appendicular skeleton. Thinning of cortical bone can be detected by bone mineral densitometry. Figure 58-2 demonstrates typical preferential loss of cortical bone in primary hyperparathyroidism. In contrast, excess PTH secretion appears to have a relative protective effect against bone loss at sites of cancellous bone, such as vertebral bone. Trabecular plates are typically maintained in number and in connectivity in primary hyperparathyroidism (Fig. 58-3; see Chap. 55).31,32 and 33
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree