Chapter 40 Clinical Approach to Infections in the Compromised Host
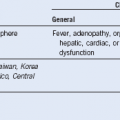
Figure 40-1 CONSTELLATION OF FACTORS CONTRIBUTING TO INCREASED RISK FOR INFECTION IN IMMUNOCOMPROMISED HOSTS.
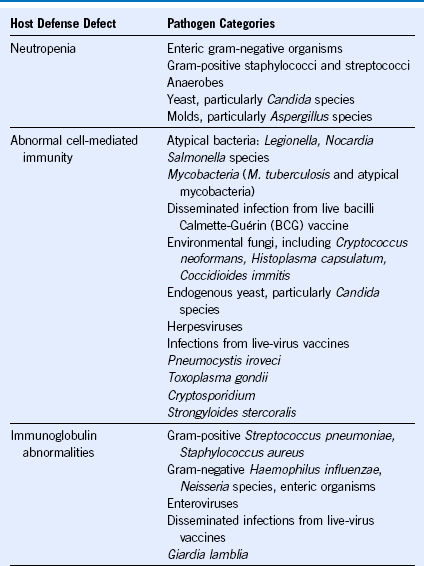
Table 40-1 Malignant and Select Nonmalignant Hematologic Diseases and Their Associated Infection-Predisposing Host Defects
| Hematologic Condition | Infection-Predisposing Host Defects |
|---|---|
| Acute myeloid leukemia | Neutropenia; therapies such as dose-intensive chemotherapy and hematopoietic stem cell transplant may result in additional anatomic disruptions, cell-mediated defects, and humoral defects |
| Acute lymphocytic leukemia | Neutropenia; therapy effects similar to acute myeloid leukemia |
| Hairy cell leukemia | Neutropenia (also monocytopenia); abnormal humoral immunity; T-cell suppressing therapy |
| Chronic lymphocytic leukemia | Hypogammaglobulinemia; abnormal cell-mediated immunity |
| Chronic myeloid leukemia | No prominent host defects unless aggressive therapy, advanced stage, or postsplenectomy |
| Multiple myeloma | Hypogammaglobulinemia; other host defects may occur with aggressive therapy or advanced stage |
| Hodgkin/non-Hodgkin lymphomas | Abnormal cell-mediated immunity, therapy-related neutropenia, splenic dysfunction (if splenectomy or radiation) |
| Myelodysplastic syndromes | Functional or absolute neutropenia |
| Aplastic anemia | Neutropenia; abnormal cell-mediated immunity from immunosuppressive therapies (e.g., steroids, antithymocyte globulin, cyclosporine, hematopoietic stem cell transplantation) |
| Paroxysmal nocturnal hemoglobinuria | Deficient Fc receptor may contribute to abnormal cell-mediated immunity |
| Hemolytic states (thalassemia) | Gallstones may serve as a nidus for infection; splenic dysfunction or splenectomy |
| Sickle cell disease | Can be neutropenic with aplastic crisis; bone infarcts may serve as a nidus for infection; splenic dysfunction with poor complement activation and opsonization from autosplenectomy |
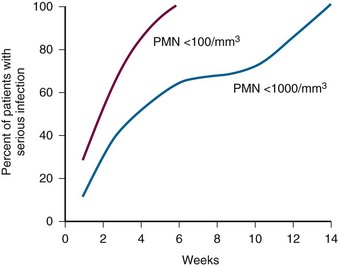
Figure 40-2 RELATIONSHIP OF SEVERITY AND DURATION OF NEUTROPENIA TO THE RISK FOR DEVELOPING A SERIOUS INFECTION.
(Courtesy GE Body.)