22 Chronic myeloid leukaemia (CML) is a clonal myeloproliferative disorder which results from an acquired genetic change in a pluripotential stem cell. The disease is characterised by a gross overproduction of neutrophils and their precursors (Fig 22.1). It is unusual in having three clinical phases: a relatively benign ‘chronic phase’ is followed by an ominous ‘accelerated phase’ and, finally, an almost invariably fatal acute leukaemic phase termed ‘blast crisis’. Fig 22.1 Blood sample (right) from a patient with CML. The hallmark of CML cells is the presence of a Philadelphia (Ph) chromosome – the t(9;22)(q34;q11) chromosomal translocation. Over 95% of classical CML cases are Ph positive. The Ph translocation causes the fusion of the ABL proto-oncogene from chromosome 9 to the interrupted end of the breakpoint cluster region (BCR) of chromosome 22 (Fig 22.2). The chimeric BCR-ABL gene created on the Ph chromosome (22q−) encodes a protein with considerably greater tyrosine kinase activity than the normal counterpart. In chronic phase CML, cells in the progenitor pool have increased proliferation due to over-expression of BCR-ABL. The mechanism by which the BCR-ABL oncogene affects stem cell kinetics is not well understood. It presumably deregulates signalling pathways involved in proliferation, apoptosis, cellular adhesion and genomic stability. Progression to blast crisis with production of leukaemic stem cells requires complex additional events including increased proliferation and self-renewal capacity avoidance of cell death, a block in differentiation and bypassing of normal immune responses. Fig 22.2 The Philadelphia chromosome.
Chronic myeloid leukaemia

Note the greatly increased white cell component (‘buffy coat’) compared with the normal sample.
Pathogenesis
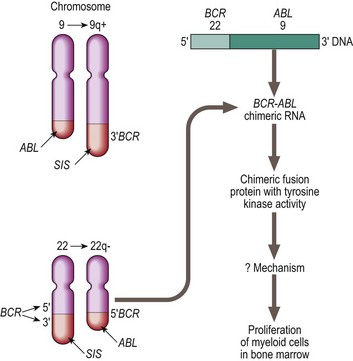
Chromosomal and molecular abnormalities in chronic myeloid leukaemia. In a translocation between chromosomes 9 and 22 (t(9;22) ) the oncogene ABL on chromosome 9 is moved to the breakpoint cluster region (BCR) of chromosome 22. The resulting BCR-ABL hybrid gene encodes a protein with high tyrosine kinase activity.
Oncohema Key
Fastest Oncology & Hematology Insight Engine



