Richard J. Whitley
Chickenpox and Herpes Zoster (Varicella-Zoster Virus)
Varicella-zoster virus (VZV) causes two distinct clinical diseases. Varicella, more commonly called chickenpox, is the primary infection and results from exposure of a person susceptible to the virus to someone who is actively infected. Chickenpox is ubiquitous and extremely contagious, but for the most part, it is a benign illness characterized by a generalized exanthematous rash. It occurs seasonally and in epidemics. Recurrence of infection results in the localized entity known as herpes zoster, often referred to as shingles, a common infection among the elderly and immunocompromised hosts. Two live, attenuated vaccines for the prevention of chickenpox and herpes zoster are licensed in the United States. Vaccination is recommended for use in healthy children and in susceptible adults to prevent chickenpox (see Chapter 321). Similarly, the herpes zoster vaccine is recommended for adults older than 50 years of age to decrease the burden of illness and the overall incidence of shingles. The incidence of chickenpox was that of the annual birth rate but has been tremendously reduced with widespread vaccination. Surveillance for varicella in three counties in California, Texas, and Pennsylvania from 1995 to 2000 showed reductions in cases of varicella from 71% to 84% by years 1999 and 20001 with only 500 cases occurring in 2004.2 Since the implementation of a two-dose vaccine series, the incidence of chickenpox has decreased to 5 cases in 100,000 in states with adequate reporting.3 Approximately 1 million cases of herpes zoster, which result in more than 2 million physician visits annually, occur yearly in the United States. Likely, this approximation is an underestimation of disease occurrence. Many of these individuals require long-term follow-up medical care for postherpetic neuralgia (PHN).
Historical Overview
Shingles has been recognized since ancient times as a unique clinical entity because of the dermatomal vesicular rash; however, chickenpox was often confused with smallpox.4 In 1875, Steiner successfully transmitted VZV by inoculation of the vesicular fluid from a person suffering from chickenpox to human “volunteers.”5 The infectious nature of VZV was further defined by von Bokay,6,7 who observed chickenpox in persons who had close contact with others suffering from herpes zoster. He correctly described the mean incubation period for the development of chickenpox in susceptible patients, as well as the average range in days. Kundratitz in 19258 showed that the inoculation of vesicular fluid from patients with herpes zoster into susceptible persons resulted in chickenpox. Similar observations were reported by Brunsgaard9 and others,10 and in 1943 Garland11 suggested that herpes zoster was the consequence of the reactivation of latent VZV.
Since early in the 20th century, similarities in the histopathologic features of skin lesions and in epidemiologic and immunologic studies indicated that varicella and herpes zoster were caused by the same agent.12,13 Tyzzer14 described the histopathologic features of skin lesions resulting from VZV infections and noted the appearance of intranuclear inclusions and multinucleated giant cells. These descriptions came from histologic studies performed on serial skin biopsy specimens that were obtained during the first week of illness. The histopathologic descriptions were amplified by Lipschutz in 192115 for herpes zoster.
Isolation of VZV in 1958 permitted a definition of the biology of this virus.13 Viral isolates from patients with either chickenpox or herpes zoster demonstrated similar changes in tissue culture, specifically the appearance of eosinophilic intranuclear inclusions and multinucleated giant cells. These findings are virtually identical to those present on clinically available biopsy material. Taken together, these data provided a universal acceptance that both diseases were caused by VZV. By 1958, Weller and colleagues13,16–18 established that there were neither biologic nor immunologic differences between the viral agents isolated from patients with these two clinical entities. Later studies provided their identity by rigorous biochemical methods.19 Viral DNA from a patient with chickenpox who subsequently developed herpes zoster was examined by restriction endonuclease analysis, and the molecular identity of these two viruses was verified.20,21
The Pathogen and Its Replication
VZV is a member of the Herpesviridae family and shares structural characteristics with other members of the family. The virus has icosapentahedral symmetry and contains centrally located double-stranded DNA with a surrounding envelope. The size of the virus is approximately 150 to 200 nm, and it has a lipid-containing envelope with glycoprotein spikes.20,22 The naked capsid has a diameter of approximately 90 to 95 nm.23–25 The DNA contains 125,000 base pairs, or approximately 80 megadaltons, and encodes about 75 proteins. The organization of the viral genome is similar to that of other herpesviruses. There are unique long (105-kb) and unique short (5.2-kb) regions of the viral genome. Each unique sequence contains terminal repeat sequences. With replication, the unique short (US) region can invert on itself and result in two isomeric forms.26–28 Notably, a large portion of the VZV genome is co-linear with herpes simplex type 1 (HSV-1). For example, within the UL region of VZV, 56 of the 62 genes have HSV-1 homologues. Similarly, in the US region all four genes have homologues.
Seven VZV glycoproteins (gp) have been identified: gB, gC, gE, gH, gI, gK, and gL. These glycoproteins have been the subject of intense investigative interest because they represent the primary markers for both humoral and cell-mediated immune responses.
Only enveloped virions are infectious, likely accounting for the lability of VZV. Furthermore, the envelope is sensitive to detergent, ether, and air-drying. VZV is highly cell associated and spreads from cell to cell by direct contact. Virus can be isolated in a variety of continuous and discontinuous cell culture systems of human and simian origin. Approximately 8 to 10 hours after infection, virus-specific immunofluorescence can be detected in the cells immediately adjacent to the initial focus of infection. This parallels the microscopic observation of the radial spread of the cytopathologic process.29,30 Electron microscopic studies demonstrate the appearance of immature viral particles within 12 hours of the onset of infection. As with herpes simplex virus (HSV), the naked capsids acquire their envelope at the nuclear membrane, being released into the perinuclear space where large vacuoles are formed.23,31 Infectious virus is then spread to adjacent cells after fusion of plasma membranes.
Epidemiology of Varicella-Zoster Virus Infections
Chickenpox
Humans are the only known reservoir for VZV. Chickenpox follows exposure of the susceptible or seronegative person to VZV and represents the primary form of infection. Although it is assumed that the virus is spread by the respiratory route and replicates in the nasopharynx or upper respiratory tract, retrieval of virus from persons incubating VZV has been uncommon. However, the application of polymerase chain reaction (PCR) techniques to nasopharyngeal secretions of exposed and susceptible persons has detected VZV DNA and supports this hypothesis. Chickenpox was a common infection of childhood and affects both genders equally and people of all races. To a certain extent, the virus is endemic in the population at large; however, it becomes epidemic among susceptible persons during seasonal periods of late winter and early spring.32 Intimate contact appears to be the key determinant for transmission.
With the implementation of childhood vaccination programs in some countries, the epidemiology of chickenpox is changing dramatically with a falling incidence. However, many countries still do not employ universal immunization and, as a consequence, the epidemiology of infection remains as known historically.
Overall, chickenpox is a disease of childhood because 90% of cases occur in children younger than 13 years. Typically, the virus is introduced into the susceptible school-aged or preschool child. In a study by Wells and Holla,33 61 of 67 susceptible children in kindergarten through the fourth grade contracted chickenpox. Approximately 10% of persons older than 15 years are considered susceptible to VZV infection. The incubation period of chickenpox (i.e., the time interval between exposure of a susceptible person and the time the vesicular rash develops in an index case) is generally regarded to be 14 to 15 days, but disease can appear within a range of 10 to 20 days.34,35 Secondary attack rates among susceptible siblings within a household are between 70% and 90%.36 Patients are infectious for a period of approximately 48 hours before the period of vesicle formation and generally for 4 to 5 days thereafter until all vesicles are crusted.
Although chickenpox exists worldwide among children, it occurs more frequently in adults who reside in tropical regions than in those who reside in other geographic areas. Stokes noted a higher incidence of chickenpox among soldiers serving abroad during World War II, in whom the incidence was 1.41 to 2.27 per 1000 persons annually. These rates contrast with those in the United States, which were approximately half those reported among the soldiers.37
Herpes Zoster
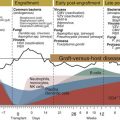
The epidemiology of herpes zoster is somewhat different. VZV characteristically becomes latent after primary infection within the dorsal root ganglia. Reactivation leads to herpes zoster, a sporadic disease. Histopathologic examination of the nerve root after infection with VZV demonstrates characteristics indicative of VZV infection. In persons who die after recent herpes zoster infection, an examination of the dorsal root ganglia reveals satellitosis, lymphocytic infiltration in the nerve root, and degeneration of the ganglia cells.38,39 Intranuclear inclusions can be found within the ganglia cells. Although it is possible to demonstrate the presence of VZV by electron microscopy, it has not been possible to isolate this virus in cultures, usually from explants of dorsal root ganglia, as has been done after HSV infection. Nevertheless, the application of PCR to extracted ganglionic DNA demonstrates latent viral DNA in neurons of sensory ganglia, including dorsal root, cranial, and enteric ganglia.40 The biologic mechanism by which VZV establishes latency remains unknown.
Herpes zoster is a disease that occurs at all ages, but it afflicts about 20% or more of the population overall, mainly the elderly.41,42 Herpes zoster, also known as shingles, occurs in persons who are seropositive for VZV or, more specifically, in those who have had chickenpox. Reactivation appears to be dependent on a balance between virus and host factors. Most patients who develop herpes zoster have no history of exposure to other persons with VZV infection at the time of the appearance of lesions. The highest incidence of disease varies between 5 and 10 cases per 1000 for persons older than 60 years.16 Approximately 4% of patients experience a second episode of herpes zoster; however, recurrences of dermatomal lesions are usually caused by HSV. This finding was verified in the SHINGLES PREVENT vaccine study.43 In a 7-year study performed by McGregor,44 the annualized rate of herpes zoster was 4.8 cases per 1000 patients and three fourths of those patients were older than 45 years. Persons who are immunocompromised have a higher incidence of both chickenpox and shingles.45–48 Herpes zoster occurs within the first 2 years of life in children born to women who have had chickenpox during pregnancy. These cases probably reflect in utero chickenpox with reactivation early in life.
Pathogenesis
Chickenpox occurs in susceptible persons who are exposed to virus after close personal contact. Histopathologic findings in human VZV infections, whether chickenpox or herpes zoster, are virtually identical. The vesicles involve the corium, or dermis. As viral replication progresses, the epithelial cells undergo degenerative changes characterized by ballooning, with the subsequent appearance of multinucleated giant cells and prominent eosinophilic intranuclear inclusions. Under unusual circumstances, necrosis and hemorrhage may appear in the upper portion of the dermis. As the vesicle evolves, the fluid becomes cloudy as a consequence of the appearance of polymorphonuclear leukocytes, degenerated cells, and fibrin. Ultimately, either the vesicles rupture and release infectious fluid, or the fluid gradually becomes reabsorbed.
As noted earlier, transmission is likely by the respiratory route, followed by localized replication at an undefined site, with lymphatic spread and seeding of the reticuloendothelial system and, ultimately, viremia. The occurrence of viremia in patients with chickenpox is supported by the detection of virus in peripheral blood mononuclear cells and by the diffuse and scattered nature of the skin lesions, and it can be verified in selected cases by the recovery of virus from the blood.49 The mechanism of VZV reactivation that results in herpes zoster is unknown.
Clinical Manifestations
Chickenpox
Chickenpox is generally a benign, self-limited disease in immunocompetent children, whose incidence has markedly decreased as the varicella vaccine becomes more widely used. There are fewer than 14 deaths per year in the United States.50 For the normal unimmunized child, chickenpox-associated mortality is less than 2 per 100,000 cases. This risk increases by more than 15-fold for adults. The presenting manifestations of chickenpox are a rash, low-grade fever, and malaise. A prodrome of the reported symptoms may occur 1 to 2 days before the onset of the exanthem in a few patients. For the most part, chickenpox in the immunocompetent child is associated with lassitude and a temperature of 100° to 103° F of 3 to 5 days’ duration. Subsequent constitutional symptoms include malaise, pruritus, anorexia, and listlessness; these symptoms gradually resolve as the illness abates. The skin manifestations, which are the hallmark of infection, consist of maculopapules, vesicles, and scabs in varying stages of evolution. The lesions initially contain clear vesicular fluid, but over a short period of time, they pustulate and scab. Most lesions are small, having an erythematous base with a diameter of 5 mm to as large as 12 to 13 mm. The lesions can be round or oval; central umbilication occurs as healing progresses. The lesions have often been referred to as “dew drop like” during the early stages of formation. If they do not rupture within a few hours, the contents rapidly become purulent in appearance. The lesions appear on the trunk and face and rapidly spread centrifugally to involve other areas of the body. Successive crops of lesions generally appear over a period of 2 to 4 days. Thus, early in the disease, the hallmark of the infection is the appearance of lesions at all stages, as noted previously. The lesions can also be found on the mucosa of the oropharynx and even the vagina; however, these sites are less commonly involved. The crusts completely fall off within 1 to 2 weeks after the onset of infection and leave a slightly depressed area of skin.
Immunocompromised children, particularly those with leukemia, have more numerous lesions, often with a hemorrhagic base. Healing takes nearly three times longer in this population.45 These children are at greater risk for visceral complications, which occur in 30% to 50% of cases and can be fatal in up to 15% of cases in the absence of therapy. A notable complication of cutaneous lesions is secondary bacterial infection, often in association with gram-positive organisms. Streptococcal toxic shock is a rare but potentially lethal complication of varicella. Infection in the neutropenic host can be systemic, beyond cutaneous involvement.
The most frequent noncutaneous site of involvement after chickenpox is the central nervous system (CNS); the neurologic abnormalities are manifested as acute cerebellar ataxia or encephalitis.34,51–53 Cerebellar ataxia has been estimated to occur in 1 in 4000 cases among children younger than 15 years. Cerebellar ataxia can appear as late as 21 days after the onset of rash. It is more common, however, for acute cerebellar ataxia to present within 1 week of the onset of the exanthem. An extensive review by Underwood53 of 120 cases demonstrated that ataxia, vomiting, altered speech, fever, vertigo, and tremor all were common on physical examination. Cerebrospinal fluid (CSF) from these patients often demonstrates lymphocytosis and elevated levels of protein. This is usually a benign complication in children, and resolution occurs within 2 to 4 weeks. PCR techniques can detect VZV DNA in the CSF.54
A more serious CNS complication is encephalitis, which can be life threatening in adults. Encephalitis is reported to occur in 0.1% to 0.2% of persons with the disease.52 Underwood’s review53 reveals this illness to be characterized by depression in the level of consciousness with progressive headaches, vomiting, altered thought patterns, fever, and frequent seizures. The duration of disease in these patients is at least 2 weeks. Some patients experience progressive neurologic deterioration that leads to death. Mortality in patients who develop encephalitis has been estimated to range between 5% and 20%, and neurologic sequelae occur in up to 15% of survivors.
A neurologic complication of note is the late appearance of cerebral angiitis after herpes zoster ophthalmicus. Angiitis typically presents as an ischemic stroke and can occur up to several months after herpes zoster of the trigeminal ganglia. This problem has been noted in several patients and defined as being progressive with a high mortality rate. Other nervous system manifestations of chickenpox include meningitis, transverse myelitis, and Reye’s syndrome.
A serious and life-threatening complication is the appearance of varicella pneumonitis, a complication that occurs more commonly in adults and in immunocompromised persons.32,51 Among adults, it is estimated to occur in 1 in 400 cases of infection and, not infrequently, in the absence of clinical symptoms, it appears 3 to 5 days into the course of illness and is associated with tachypnea, cough, dyspnea, and fever. Pregnant women during the second and third trimesters of gestation are particularly vulnerable to pneumonitis with primary infection. Chest radiographs usually reveal nodular or interstitial pneumonitis. Varicella pneumonitis can be life threatening when it occurs in pregnant women during the second or third trimester.
In a prospective study of male military personnel, radiographic abnormalities were detected in nearly 16% of enlisted men who developed varicella, yet only one fourth of these persons had evidence of cough.55 Only 10% of those with radiographic abnormalities developed evidence of tachypnea, indicating that asymptomatic pneumonitis may exist more commonly than was initially predicted. Other manifestations of noncutaneous and non-neurologic involvement include the appearance of myocarditis, nephritis, bleeding diatheses, and hepatitis.
Perinatal varicella is associated with a high death rate when maternal disease develops 5 days before delivery or up to 48 hours postpartum.56,57 In large part, this is the consequence of the newborn failing to receive protective transplacental antibodies, as well as the immaturity of the neonatal immune system. Under such circumstances, mortality has been reported to be as high as 30%. Affected children have progressive disease involving visceral organs, especially the lung. The outcome in these children was summarized by Brunell.58 Congenital varicella, although uncommon, is characterized by skin scarring, hypoplastic extremities, eye abnormalities, and evidence of CNS impairment.59
Varicella has been associated epidemiologically with the development of Reye’s syndrome and co-administration of aspirin. Therefore, the administration of aspirin is contraindicated in persons with varicella. Cutaneous complications of concern are the development of secondary skin infections, especially those caused by Staphylococcus aureus.
Chickenpox in the Immunocompromised Patient
Chickenpox in the immunocompromised child or adult is a cause of significant morbidity and mortality. As noted previously, the duration of healing of cutaneous lesions can be extended by a minimum of threefold. However, a more important problem is the progressive involvement of visceral organs. Data from a variety of immunocompromised patient populations indicate a broad spectrum of disease in persons with lymphoproliferative malignancies and solid tumors versus bone marrow transplant recipients. Approximately one third of children develop progressive disease with involvement of multiple organs, including the lungs, liver, and CNS.45 Most of these children developed pneumonitis within the first week after the onset of infection, as do 20% of all those who acquire chickenpox. Mortality in this patient population has approximated 15% to 18%.45,60,61 Patients with lymphoproliferative malignancies who require continuous chemotherapy appear to be at greatest risk for visceral involvement.
In persons undergoing hematopoietic stem cell transplantation, the incidence of VZV infections over the first year has been estimated to be 30% by 1 year after transplantation. Eighty percent of these infections occurred within the first 9 months after transplantation, and 45% of these patients had cutaneous or visceral dissemination (see Chapter 312). Overall, 23 deaths occurred in one prospective series.47 Risk factors identified for the acquisition of VZV infection included an age between 10 and 29 years, a diagnosis other than chronic myelogenous leukemia, the post-transplant use of antithymocyte globulin, allogeneic transplant, and acute or chronic graft-versus-host disease. Notably, graft-versus-host disease increases the probability of visceral dissemination significantly. Patients receiving HSV prophylaxis with acyclovir 800 mg orally twice daily or valacyclovir 500 mg orally twice daily or receiving treatment for cytomegalovirus (CMV) reactivation with ganciclovir are protected against reactivation of VZV.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree