Abstract
Eosinophilia in neonates is identified when the blood concentration of eosinophils exceeds the upper reference range limit. To avoid the potential pitfall of laboratory or technician error, perhaps the definition should be two subsequent eosinophil counts above the upper reference limit. The 95th percentile for blood concentration of eosinophils increases slightly over the first month following birth. Initially a count ≥1,200/µL would exceed the upper range, and by about four weeks a count of above 1,500/µL would exceed the upper limit [1]. This latter value is similar to that generally used to define eosinophilia in adults [2]. Adults with persistent eosinophilia are well advised to have the situation evaluated, because an association has been seen between persistent eosinophilia and end-organ damage [2]. Some adults with persistent eosinophilia have elevated blood Interkeukin-5 (IL-5) concentrations [3]. Some with hypereosinophilic syndrome have an eosinophilic leukemia involving a translocation in the tyrosine kinase gene [4].
Eosinophilia and Eosinopenia
Eosinophilia in neonates is identified when the blood concentration of eosinophils exceeds the upper reference range limit. To avoid the potential pitfall of laboratory or technician error, perhaps the definition should be two subsequent eosinophil counts above the upper reference limit. The 95th percentile for blood concentration of eosinophils increases slightly over the first month following birth. Initially a count ≥1,200/µL would exceed the upper range, and by about four weeks a count of above 1,500/µL would exceed the upper limit [1]. This latter value is similar to that generally used to define eosinophilia in adults [2]. Adults with persistent eosinophilia are well advised to have the situation evaluated, because an association has been seen between persistent eosinophilia and end-organ damage [2]. Some adults with persistent eosinophilia have elevated blood Interkeukin-5 (IL-5) concentrations [3]. Some with hypereosinophilic syndrome have an eosinophilic leukemia involving a translocation in the tyrosine kinase gene [4].
Interleukin-5 (IL-5) probably plays a role as a regulator of eosinophil production. Evidence for this includes the reports of Lee and associates [5] and Dent and coworkers [6] who produced transgenic mice that constitutively over-expressed IL-5. These animals had profound eosinophilia, generally equaling 60% of circulating leukocytes. However, mice with a targeted gene disruption of IL-5 that consequently produce no IL-5, have a reduced number of blood and marrow eosinophils but no other apparent hematologic defects [6]. Further evidence that IL-5 regulates eosinophil production comes from studies of Rennick and colleagues [7] and Sher and associates [8] who used specific neutralizing antibody directed against IL-5 and observed that such inhibits the eosinophilia otherwise seen in parasitized mice. More evidence that IL-5 stimulates eosinophil production comes from the work of Lu and colleagues [9] who determined that recombinant murine IL-5 had the greatest effect of any factor tested on colony generation of eosinophilic progenitors.
Evidence that IL-5 is a regulator of eosinophil production in humans was provided by Brugnoni and associates, who reported a patient with hypereosinophilia caused by a population of T cells that secreted large amounts of IL-5 [10]. Glucocorticoid administration can result in an abrupt drop in blood eosinophil concentrations, accompanying reduced expression of IL-5 [11]. Interferon-α, which has beneficial effects in many eosinophil-mediated disorders, also inhibits IL-5 gene expression [12]. In a manner reminiscent of the actions of granulocyte colony-stimulating factor on neutrophils, IL-5 stimulates eosinophil function and eosinophil production. Walsh and coworkers observed that IL-5 enhances the adhesion of human eosinophils by a mechanism dependent on CD 11/18 family of adhesions glycoproteins [13]. However, IL-5 does not enhance adhesion of neutrophils. Taken together, this information indicates that IL-5 is a significant physiologic regulator of eosinophil production and function.
Eosinophilia is not a rare finding in the neonatal intensive care unit, but in reports of such, various definitions for eosinophilia have been used. When comparing reports, the definition used for eosinophilia is obviously critical, because the higher the cut-off level used, the lower will be the prevalence of eosinophilia.
The expected range of blood concentrations of eosinophils in neonates has been reported in a few small studies, and more recently in a very larger study including over 80,000 neonates [1]. Medoff and Barbero reported that during the first 12 hours after birth blood eosinophil concentrations range from 20 to 850/µL [14]. On the basis of that report, eosinophilia on the first day of life would be defined as a blood eosinophil count of more than 850/µL. Our large study suggests that a count exceeding 1,200/µL on the day of birth is a more accurate definition of an elevated count [1]. Xanthou reported that by the fifth day after birth eosinophil concentrations had a much greater range than on the first day, with values of 100 to 2,500/µL [15]. Our data suggests that counts as high as 2,500/µL would always be abnormal.
Burell postulated that a complete lack of blood eosinophils in neonates should be considered an abnormality [16]. He found that an absence of eosinophils on the complete blood count (CBC) was common only among infants who fared poorly and subsequently died. He reported that on the day of death there was generally a complete absence of blood eosinophils. Bass reported that blood eosinophil concentrations declined rapidly in the presence of bacterial infection [17]. Our work also suggests that a blood eosinophil count of zero/μL is abnormal, falling below the 5th % reference range [1].
In growing preterm infants, a nonspecific low-grade eosinophilia is so common as to have been given the label “eosinophilia of prematurity.” Despite its relatively frequent occurrence, the causes and significance of this condition are uncertain. Defining eosinophilia as blood concentration >700/µL, Gibson and coworkers found that 75% of preterm infants develop eosinophilia [18]. They also observed that this eosinophilia of prematurity generally occurs during a period in which an anabolic state is established. This anabolic state and the accompanying eosinophilia usually are seen in the second or third week of life, and the eosinophilia persists for many days and sometimes for weeks. Portuguez-Molavasi reported that at least one episode of eosinophilia (defined as a count exceeding 1,000/µL) occurred in 35% of all infants admitted to an intensive care nursery [19]. Craver reported that eosinophils can be seen in the cerebrospinal fluid weeks after intraventricular hemorrhage [20], but the significance of this finding is not clear, and this finding did not correlate with blood eosinophil counts.
Although several reports suggest that the eosinophilia of prematurity is benign, the work of Patel and colleagues suggests otherwise [21]. In a retrospective evaluation of 261 admissions to their intensive care unit, eosinophilia (defined as >1,000 eosinophils/µL) was found in 33 patients. When age-matched patients without eosinophilia were compared with these, the development of sepsis was much higher in those with eosinophilia. All of 10 neonates born at 26 weeks’ gestation or younger who developed eosinophilia also developed at least one nosocomial infection. Twenty of 23 born at >26 weeks’ gestation who developed eosinophilia also had sepsis, compared with only 4 of 23 matched infants who did not have eosinophilia. Whether eosinophilia preceded, was concomitant with, or came after the infections is not clear, but these researchers warn of the correlation between eosinophilia and sepsis, particularly with Gram-negative organisms.
The clinical significance of the eosinophilia of prematurity was also addressed by Odelram and associates using the observation that high blood concentrations of eosinophils are often seen in atopic diseases [22]. They attempted to correlate eosinophil counts in neonates with the subsequent development of atopy, determined at the age of 18 months, but little or no correlation was found. Yamamoto and coworkers observed that blood eosinophils counts might be somewhat elevated in neonates who develop chronic lung disease and suggested that eosinophils might become activated in certain patients with hyaline membrane disease and that these cells could subsequently appear in the airways [23]. This postulate accounts for the timing of the eosinophilia of prematurity and the development of chronic lung disease, but not all infants with the eosinophilia of prematurity develop chronic lung disease, and not all neonates with chronic lung disease have antecedent eosinophilia. Others have postulated that medications or constituents of hyperalimentation solutions are responsible for the eosinophilia.
Tissue infiltration with eosinophils has been associated with a variety of pathological conditions in neonates. Most of these conditions are accompanied by blood eosinophilia, and thus eosinophils have been postulated as central to the pathogenesis of these conditions. These include the relatively transient and benign cutaneous eruption within days after birth, termed erythema toxicum neonatorum [24, 25], a similar but much more marked cutaneous eruption termed neonatal eosinophilic pustulosis [26, 27], and infantile eczema [28]. Chronic respiratory inflammation associated with eosinophilic pulmonary infiltrates, sometimes with accompanying blood eosinophilia, include Chlamydia trachomatis [29], respiratory syncytial virus [30], and bronchopulmonary dysplasia [23, 31]. Other inflammatory conditions associated with eosinophilic infiltrates and eosinophilia are neonatal eosinophilic esophagitis [32], eosinophilic colitis [33], subcutaneous fat necrosis with eosinophilic granules [34], a variety of infections, necrotizing enterocolitis, and after erythrocyte transfusions [35]. The exact roles of eosinophils in the pathogenesis of these conditions, and whether blood eosinophil counts can be of value in identifying or suspecting these conditions, remain to be determined.
Neutrophilia and Leukemoid Reactions
Reference ranges for blood neutrophil concentrations of neonates are very wide. Neonates born at high altitude (above 4,000 ft) have an even wider range of expected values than do those born at sea level. For instance, blood neutrophil concentrations following birth in Colorado [36] New Mexico [37], and Utah [38] all have a substantially higher 95% reference limit than do those reported in Dallas, Texas [39–41] and Athens, Greece [15, 42]. In these reports, no differences are apparent in the 5% limit, but the 95% limit at high altitude is almost twice that at sea level. The exact mechanism by which high altitude results in considerably higher blood neutrophil counts, over the first days after birth, is unclear. Moreover, it is possible that this difference in upper range limit, ascribed to altitude, is actually the result of differences other than altitude. Large numbers of neutrophil counts from neonates in yet other sites would be helpful in confirming whether there is indeed an important altitude-based difference in blood neutrophil concentration. For instance, data from the neonatal intensive care units (NICUs) at very high altitudes in South America and Asia, and additional data from NICUs at sea level would help resolve this issue.
Bacterial infection is the condition most commonly reported as the cause of neonatal neutrophilia [43, 44]. Chorioamniotitis has been associated with neonatal leukemoid reactions, particularly among extremely low birth weight (ELBW) neonates [45]. Leukemoid reactions were first reported by Krumbhaar in 1926 as an extreme elevation in blood neutrophil concentration [46]. Leukemoid reactions in the NICU have been defined variably as a leukocyte count in excess of 50 × 103/µl, or if more than 2% of the blood leukocytes are immature myeloid cells capable of division (myeloblasts, promyelocytes, or myelocytes). As a consistent approach, at the University of Florida (85 ft above sea level) we defined a neonatal leukemoid reaction as: (1) a blood neutrophil count greater than 30.0 × 103/µL between birth and 60 hours of life; (2) a count greater than 15.0 × 103 /µL from 60 hours to 28 days; or (3) greater than 5% blasts, promyelocytes, or myelocytes on a differential blood cell count regardless of the blood neutrophil count [47]. When defined this way, leukemoid reactions were identified in 1.3% of our NICU patients. Evaluating these neonates, even with neutrophil counts as high as 100,000/µL, did not identify any with hyperviscosity and, except for one patient with trisomy 21, all cases of extreme neutrophilia were transient, persisting generally for only a few days. We suspect the responsible kinetic mechanism for this variety of neonatal neutrophilia is increased neutrophil production, not steroid-induced leukocytosis, and is likely from granulocyte colony-stimulating factor (G-CSF) produced during chorioamnionitis or relatively mild to moderately severe neonatal infections [47].
Leukemoid reactions in the NICU, particularly among ELBW and very low birth weight (VLBW) neonates, tend to presage the later development of chronic lung disease. Zanardo et al. suggested that the in utero exposure to proinflammatory cytokines initiating the neonatal leukemoid reaction, conditions the lungs to damage and prolongs the need for supplemental oxygen [48]. Hsiao and Omar also reported this association between early leukemoid reaction, in ELBW neonates, and a higher incidence of bronchopulmonary dysplasia (54% in those with a leukemoid reaction vs. 25% in matched controls that did not have a leukemoid reaction) [49]. However, they found no significant differences in neurodevelopmental outcome between groups at 2 years of age. Zanardo et al. provided further confirmation that histological chorioamnionitis is a risk factor predisposing to leukemoid reaction and subsequently to chronic lung disease [50].
Neonates with Down syndrome have a high prevalence of hematologic abnormalities, including neutrophilia, transient myeloproliferative disorder, congenital leukemia, thrombocytopenia, and polycythemia [51]. Cutaneous vesiculopustular eruptions have been described in those with neonatal myeloproliferative disorders. These lesions contain immature hematopoietic cells similar to blasts, and resolution occurs without specific treatment, concurrent with resolution of the hematologic disorder [52, 53]. Neonates with Down syndrome and a leukemoid reaction have a 20 to 30% probability of developing acute megakaryocyte leukemia, associated with mutations in the N-terminal activation domain of the GATA-1 gene [54, 55].
Case report association have been made between persistent neonatal neutrophilia and persistent severe pulmonary hypertension [56], and between persistent neutrophilia and leukocyte adhesion deficiency [57]. It might be that some of the previous publications on neonatal neutrophilia should be re-examined in light of altitude-appropriate reference ranges [58]. For instance, patients with Down syndrome [51], trisomy 13 [59], and trisomy 18 [59] are all very likely to have neutrophilia in the neonatal period, but the influence of altitude complicates this conclusion. Other considerations discovered by studying very large sample sizes of CBC include that, during the first day following birth, neonates delivered after labor have 20% to 30% higher blood neutrophil counts than do those delivered by cesarean section without labor (38). Also, over the first 3 days, females have higher neutrophil counts than do males, averaging 10% to 20% higher [38].
Neutropenia
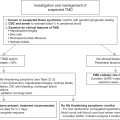
Among newborn infants, the CBC is one of the most commonly obtained of all blood tests. Sometimes a CBC is ordered anticipating that neutropenia might be present, as is the case in a neonate with septic shock, or in a small for gestational age (SGA) neonate born after severe preeclampsia. However, most cases where a neonate’s CBC reveals neutropenia come as an unexpected puzzle. The neonatologist or pediatrician seeing such a result might wonder: What conditions should I consider in the differential diagnosis? Will the neutropenia be a significant medical problem or will it be trivial and transient? What steps should I take to evaluate the neutropenia? Should I obtain cultures and initiate antibiotic treatment? Should I order IVIg? Should I order G-CSF?
One reasonable place to start this process is by repeating the CBC, to ensure laboratory error is not responsible for the finding. While the repeat sample is being drawn and run, you might consider the following three issues in order to generate a framework in which to proceed if the repeat test confirms that neutropenia is indeed present. These three questions are: (1) Does the neutropenia appear to be congenital or acquired? (2) Does the baby have signs of illness that could be the result of an infection, or is she/he basically well appearing? (3) Are there additional abnormalities on the CBC?
First, how are you defining neutropenia? Consider the number of neutrophils per microliter of blood, also known as the ANC (absolute neutrophil count) and not just the WBC (white blood cells or leukocytes per microliter). If you find an ANC less than 1,000/µL twice sequentially, the patient can be said to have neutropenia. If you find two simultaneous ANCs <500/µL the patient can be said to have severe neutropenia. Counts above 1,000/µL can technically be neutropenic, if they fall below the 5th percentile reference range. For instance, an ANC of 3,000/µL 6 hours after birth is indeed an abnormally low ANC. The fact that the ANC is below the reference range signals the presence of pathology. However, it is doubtful that a count as high as 3,000/µL constitutes a host-defense deficiency or renders the patient at high risk for acquiring an infection. Therefore, we tend to use the diagnosis “neutropenia,” or place neutropenia on the problem list, only if the ANC is twice, sequentially, less than 1,000/µL.
Table 16.1 shows three questions to consider when evaluating a neonate with neutropenia.
Table 16.1 Evaluating a neonate with neutropenia
| Three questions to consider when neutropenia is found on a neonate’s CBC |
|---|
| 1. Does the neutropenia appear to be congenital or acquired? |
| 2. Does the baby have signs of illness that could be the result of an infection, or is she/he basically well appearing? |
| 3. Are there additional abnormalities on the CBC? |
1. Does the neutropenia appear to be congenital or acquired? Is this the first CBC obtained on this patient? The common neonatal neutropenias are often seen on the very first CBC. These include the neutropenia of maternal hypertension and the neutropenia associated with early-onset sepsis. Alternatively, has the patient had a normal ANC for days or weeks and now has neutropenia? If so, what else has changed? Has a significant infectious illness or NEC been acquired? Is this a case of late neutropenia appearing in an otherwise growing preterm neonate, sometimes called “idiopathic neonatal neutropenia”? These late-appearing varieties of neonatal neutropenia cannot be ascribed to maternal hypertension or alloimmune mechanisms.
2. Does the baby have signs of illness that could be the result of an infection, or is she/he basically well appearing? Mild infections in neonates tend to result in neutrophilia, while septic shock is more likely to result in neutropenia. Thus, when severe neutropenia if found in a well appearing neonate, the neutropenia is not at all likely to be the neutropenia of sepsis. A well-appearing neonate with neutropenia raises the possibility of immune-mediated neutropenia (alloimmune, maternal autoimmune, or neonatal autoimmune). Similarly, a neonate with any of the varieties of severe congenital neutropenia can appear completely well, unless infection has been acquired. When an otherwise well neonate has syndromic features and neutropenia, it is likely that the neutropenia is part of the syndrome. Other tie-ins with the issue of well versus ill, include hypoglycemia and neutropenia with glycogen storage disease type Ib and pancreatic exocrine insufficiency and neutropenia with Shwachman–Diamond syndrome.
3. Are there additional abnormalities on the CBC? Neutropenia resulting from sepsis is generally accompanied by characteristic laboratory features. An increased immature to total (I/T) ratio is common, reflecting the call of neutrophil from the marrow to sites of infection. The hematology laboratory technician sometimes reports morphological changes in the neutrophils, like toxic granulation, Dohle bodies, and vacuolization. Thrombocytopenia and an elevated MPV sometimes accompany the neutropenia of sepsis. Shock and acidosis are characteristics as well. Contrariwise, the neutropenia of pregnancy-induced hypertension (PIH) should not have a high I/T ratio or the morphological changes of infection.
By considering these three questions, preliminary conclusions can be rapidly reached and these will dictate the next steps. The neutropenia of infection requires appropriate antibiotic coverage and intensive care monitoring and treatment. This is the case in early-onset sepsis and also late onset conditions including NEC and neutropenic late-onset sepsis (most late-onset bacterial infections generate neutrophilia not neutropenia). If the neonate is well but neutropenic, when would antineutrophil antibody tests be helpful and when should the possibility of severe congenital neutropenia be considered?
In general, we suggest waiting until neutropenia has persisted 5 days of more, or until severe neutropenia has persisted for 2 days or more, before engaging in further evaluation of the etiology. Transient cases of neutropenia such as the variety related to PIH, will spontaneously remit or at least will significantly improve over this period. When evaluating the possibility of immune-mediated neutropenia the assistance of a specialized neutrophil serology laboratory is needed. The initial evaluation screen can be run on blood drawn from mother and father. If neutropenia persists after a negative immune-neutropenia evaluation, particularly if the ANC remains <500/µL, it is time to consider severe congenital neutropenia.
Given this framework for the initial approach, readers can now consult the following paragraphs, Table 16.2, and the section “Consistent Approaches” for more detail regarding the pathogenesis, evaluation, and treatment of the common and rare varieties of neutropenia among neonates.
Table 16.2 Classification of varieties of neutropenia in neonates based on timing of presentation and whether they are primarily the result of reduced production vs. accelerated destruction of neutrophils
| Categories of neutropenia in neonates |
|---|
| Transient hyporegenerative neutropenias present at birth |
|
| Neutropenias with accelerated neutrophil destruction generally present in first days |
|
| Chronic hyporegenerative neutropenias generally present in first days |
|
| Neutropenias presenting late in the NICU course |
|
The Transient Hyporegenerative Neutropenias Present at Birth
Maternal Hypertension, Donors of Twin–Twin Transfusion Syndrome, Rh Hemolytic Disease
Transient hyporegenerative neutropenia is common among neonates whose mothers had PIH, and in donors of twin–twin transfusions, and in neonates with Rh hemolytic disease. These three varieties of neonatal neutropenia are considered together, because of the many features they have in common. Specifically, they are not accompanied by an elevated I/T ratio or morphological abnormalities of the neutrophils, neutropenia is present at delivery, they have elevated NRBC, reticulocyte counts, and serum erythropoietin concentrations, and the neutropenia generally persists for only a few days [60–66].
Studies of the bone marrow and cultures of the granulocytic progenitors of these patients indicated that the neutropenia is the result of impaired neutrophil production days [60–62, 65, 66]. Zook and coworkers found no association of placental pathology with incidence or severity of neutropenia [67]. Guner et al. found no difference in G-CSF serum levels in neutropenic versus non-neutropenic neonates whose mothers had preeclampsia [68], but Tsao et al. found lower levels of G-CSF in cord blood of infants whose mother had PIH, with the lowest values in those with neutropenia [69].
The issue of whether this variety of transient hyporegenerative neutropenia imparts an antibacterial host-defense defect remains unsettled. Koenig and Christensen [66] and Cadnapaphornchai and Faix [64] observed a significantly larger proportion of late-onset bacterial infection among VLBW neonates who had neutropenia from PIH than among non-neutropenic matched controls. Manzoni et al. found that Candida colonization was significantly increased among those with neutropenia from PIH (62% vs. 35% colonization rate in the first month) [70]. They also found multiple sites of Candida colonization to be higher among those with neutropenia (P<0.002). In contrast, Teng et al. found no increase in nosocomial infections among VLBW infants with early neutropenia from PIH compared with matched controls who did not have early neutropenia [71].
The administration of G-CSF to neonates with this variety of neutropenia increases the blood neutrophil concentration and increased antibacterial function of neutrophils [72–74], but no evidence indicates fewer infections, or a survival advantage, of the G-CSF recipients. On that basis, we do not recommend G-CSF treatment for neonates with the neutropenia of PIH (see the section on “Consistent Approaches”).
Neutropenias Associated with Therapeutic Hypothermia for Hypoxic Ischemic Encephalopathy
Therapeutic hypothermia has become standard of care for term newborn infants diagnosed with hypoxic ischemic encephalopathy in the first few hours after birth [75–78]. In a randomized, controlled, multicenter trial of systemic hypothermia in neonatal hypoxic ischemic encephalopathy, total and leukocyte subsets and serum chemokine levels were measured over time in both hypothermia and normothermia groups as primary outcomes for safety [79]. The hypothermia group had significantly lower median circulating total WBC and leukocyte subclasses than the normothermia group before rewarming. While the absolute neutrophil count rebounded after rewarming in the hypothermia group, chemokines were negatively correlated with their target leukocytes in the hypothermia group, suggesting active chemokine and leukocyte modulation by hypothermia. Relative leukopenia at 60–72 hours correlated with more severe central nervous system injury in the hypothermia group.
The Neutropenias Due to Accelerated Neutrophil Destruction Generally Present at Birth
Neutropenia of Sepsis and the Immune-Mediated Neutropenias
Neonates with overwhelming infection, including septic shock, are very likely to develop neutropenia. At least two mechanisms can contribute: neutrophil margination and depletion of the marrow neutrophil reserves. Neutrophil margination occurs within hours of intravenous bacterial endotoxin administration and involves a movement of circulating neutrophils to the marginal pool, including sequestration of neutrophils in the pulmonary vasculature [80]. This variety of neutropenia can be sudden and severe, resulting in fewer than 500 neutrophils/µL of blood. If a single bolus of endotoxin is given, the margination neutropenia persists for an hour or so.
Neutropenia accompanying depletion of the neutrophil reserves has a more ominous significance, as it signals few neutrophils in the marrow reserve. Animal studies comparing the hematopoietic response to infection between neonates and adults demonstrate the kinetic differences in the supply and release of neutrophil pools from the bone marrow [81]. These developmental differences increased susceptibility of newborn animals to exhaustion of bone marrow reserves when subjected to experimental infection and ultimately limited their capability to survive these infections [82, 83]. Septic neonates who are neutropenic have a higher mortality than non-neutropenic neonates [84, 85]. Neonates also have an immaturity of neutrophil production. Immaturity of granulopoiesis in preterm neonates is manifest by a low neutrophil cell mass, a reduced capacity for increasing progenitor cell proliferation and frequent occurrence of neutropenia in response to sepsis [86]. This variety of neonatal neutropenia is accompanied by an elevated I/T ratio, morphological findings of neutrophils consistent with infection. Even with excellent NICU care the patient might succumb to the infection, in which case the neutropenia generally persists until death, alternatively if the patient begins to recover from the shock state the neutrophil count generally begins to rise and within a few days might be replaced by neutrophilia.
Isoimmune Neonatal Neutropenia
Isoimmune neonatal neutropenia results from maternal production of IgG directed against antigens on fetal neutrophils [87]. This is analogous to Rh hemolytic disease in that maternal sensitization to fetal neutrophil antigens results in transplacentally acquired IgG antibody destroy the infant’s neutrophils [88]. Maternal sensitization may occur during gestation and may occur even in the fetus of a primigravida [89]. The incidence of isoimmune neonatal neutropenia is estimated to be 0.5 to 2 per 1,000 live births [90].
Affected infants frequently develop a fever in the first days of life and are particularly susceptible to cutaneous infections caused by Staphylococcus aureus. Beta-hemolytic Streptococcus and Escherichia coli have also been linked to infections among susceptible infants with this disorder. The onset of infection is usually concurrent with severe neutropenia. In the circulation the concentrations of other myeloid lineages particularly monocytes and eosinophils are typically increased. Characteristic findings on bone marrow evaluation are myeloid hyperplasia with a paucity of mature neutrophils and normal erythropoietic and megakaryocytic elements.
Neutrophil antibodies are detected in the sera of mother and infant. The antibodies react against neutrophils of the patient and of the father, but they do not react against neutrophils from the mother. Several neutrophil-specific antibodies have been implicated, including most commonly human neutrophil alloantigens (HNA)-1, HNA-2, and HNA-3. Other antigenic targets include NC1, SH, SAR, LAN, LEA, CN1, and certain HLA antigens. HNA-1 and NC1 have been identified as isotypes of the FcγIII receptor [87]. HNA-2 is an antigen on glycoprotein (GP)50 and HNA-3 corresponds to an antigen on GP75-90. The infant’s neutrophil counts typically normalize over the first 1 to 5 weeks of life as might be expected with the half-life of maternal antibodies.
Treatment for affected infants is supportive. Therapy also includes appropriate antibiotic administration for infections and close follow-up. The use of prophylactic antibiotics has been shown to be ineffective. Intravenous immunoglobulin (IVIg) administration and steroid therapy have not been shown to consistently improve circulating neutrophil counts. For infants with persistence of extremely low neutrophil counts, less than 500 cells per microliter, G-CSF administration might be undertaken. This therapy usually results in a prompt clinical response in circulating neutrophil concentrations.
Maternal Autoimmune Neutropenia
Neonatal autoimmune neutropenia results from transplacental passage of maternal IgG autoantibodies directed against neutrophil antigens. Mothers of these infants can be asymptomatic or have autoimmune neutropenia from systemic lupus erythematosus or idiopathic thrombocytopenic purpura [91, 92].
Neonatal Autoimmune Neutropenia
Autoimmune neutropenia (AIN) is a disorder caused by increased destruction of neutrophils as a result of autoantibodies to the patient’s own neutrophils [93]. The incidence is approximately 1 per 100,000 live births [94]. Primary AIN is not associated with other autoimmune disorders such as systemic lupus erythematosus. Reports of associations with parvovirus B19 and β-lactam antibiotics suggest mechanisms such as development of cross-reacting antibodies resulting from molecular mimicry, changes in endogenous antigens, enhanced HLA expression, or loss of suppression of self-reacting lymphocyte clones. HNA-1a (NA-1) autoimmunization has been linked to HLA-DR2, a finding implicating immune response genes [95]. Patients with this immune mediated neutropenia are identified in the first 3 years of life with a variety of infections. In approximately 80% of patients the infections are mild, consisting of abscesses, conjunctivitis, gastroenteritis, otitis media, pyoderma, and upper respiratory infections. In the remaining cases AIN predisposes to serious infections such as meningitis, pneumonia, and sepsis [96]. Diagnosis of AIN is made by detection of neutrophil-specific antibodies [97]. Generally, patients with AIN do not require specific treatment for the neutropenia, however, to increase neutrophil counts in cases of severe infection or before elective surgery, some patients have been treated with corticosteroids, IVIg or G-CSF. Corticosteroids and IVIg increased neutrophil counts in about 50% of individuals, whereas G-CSF increased neutrophil counts in all patients treated [97]. Infections are treated symptomatically with antibiotics. Infants with recurrent infections are often treated with prophylactic antibiotics.
The Chronic Hyporegenerative Neutropenias Generally Present at Birth
Severe Congenital Neutropenia and Cyclic Neutropenia
Severe congenital neutropenia and cyclic neutropenia are rare disorders of myelopoiesis usually caused by heterogeneous mutations in ELANE, the gene that encodes neutrophil elastase [98, 99]. Mutations in CSF3 R, RAS, and RUNX1 are associated with evolution to myelodysplastic syndrome (MDS) and acute myelogenous leukemia (AML), but the biological basis for the substantial difference in risk of leukemic evolution for cyclic neutropenia versus severe congenital neutropenia is not known [100–102].
Patients with severe congenital neutropenia usually have ANC less than 500 cells/mL without regular cyclic fluctuations and a bone marrow showing maturational arrest of the myeloid lineage. Cyclic neutropenia is characterized neutrophil fluctuations from near 2,000 cells/mL to less than 200 cells/mL at approximately 21 day intervals [103]. The duration of the neutropenic episodes ranges from 3 to 10 days. Other formed elements in the blood with short circulation times such as monocytes, platelets and reticulocytes also cycle. Bone marrow aspirates during periods of neutropenia are noteworthy for cellular hypoplasia or maturational arrest [104]. Individual with cyclic neutropenia have medical histories of repetitive infections occurring in tandem with cyclic episodes of depressed circulating neutrophil concentrations. The severity of infections tends to correlate with the degree of neutropenia. Although cyclic neutropenia is usually benign, death from sepsis occurs in as many as 10% of affected individuals. The disease persists throughout the patients’ lifetimes [105].
A recent review of data from the Severe Chronic Neutropenia International Registry (SCNIR) including 307 patients with ELANE mutations was conducted to assess the relationships of mutations and risk for severe outcomes and MDS/AML [106]. The diagnosis was made based on clinical data, and the ELANE mutations were identified later in all cases. The SCNIR population included 40 families with 2 or more affected members (cyclic neutropenia 20 families; severe congenital neutropenia 20 families). The family members with neutropenia had ELANE mutations, and all members with ELANE mutations had neutropenia. Of the 307 patients only 10 were not exposed to G-CSF. For the severe congenital neutropenia patients, there were 15 deaths attributable to MDS/AML and 3 transplant-related deaths in patients who failed to respond to G-CSF, and 4 others of unknown cause. For the cyclic neutropenia patients, there were 8 deaths, none due to MDS/AML. Three deaths were attributable to sepsis; two of these patients were known not to be taking G-CSF as recommended, and one other patient was never treated with G-CSF. One death followed hematopoietic transplantation (not for MDS/ AML). The causes of the other four deaths were: cancer (one), heart failure (one), stroke (one), and unknown (one).
Infections were common in these patients before G-CSF, including mouth ulcers (80%), pneumonia (49%), abscesses (19%), sepsis (17%), cellulitis (12%), and peritonitis (3%). Sixty-one of 97 patients (63%) with mutations unique to SCN reported pneumonia, compared to 31 of 73 patients (42%) with overlapping mutations and 5 of 26 patients (19%) with mutations only seen in cyclic neutropenia. Abscesses occurred in all patient groups: overlapping mutations (4 of 73, 5%), cyclic neutropenia (4 of 26, 15%) or severe congenital neutropenia (19 of 97, 20%) [106].
With longitudinal follow-up, severe events (MDS/AML, stem cell transplant, or death) was far greater in severe congenital neutropenia versus cyclic neutropenia patients (8 of 120 cyclic neutropenia versus 62 of 187 severe congenital neutropenia, P < 10−4). The striking excess of severe events over time in severe congenital neutropenia versus cyclic neutropenia and for mutation unique to severe congenital neutropenia versus the overlapping mutations in patients on G-CSF was also highly statistically significant (P < 10−4).
The investigators grouped mutations in five principal categories: missense, frameshift, termination, intronic, and deletion or insertion. The missense mutations were most common, and 94% were predicted to have a probable or possible damaging effect on the protein structure by Polyphen 2 analysis. The most striking finding was the association of frameshift mutations in congenital patients with a high risk of abscesses (8/17 evaluable patients, 47%) and evolution to MDS/AML (6/19 patients, 32%). It appears also that a higher proportion of termination mutations are associated with leukemic transformation, but the number of these patients is relatively small. Two mutations C151Y (3/4 patients) and G214 R (3/9 patients) appear to confer a high risk of leukemia. The apparent high risk associated with these mutations may be attributable to major changes in protein structure due to size and charge/polarity differences of exchanged amino acids. Overall, the study demonstrated that clinically important genotype–phenotype correlations of clinical outcomes and the results of sequencing of ELANE for patients with cyclic and congenital neutropenia. Some mutations appear to be linked to a relatively good prognosis, notably P139 L, IVS4+5 G>A, and S126 L, whereas other mutations, specifically C151Y and G214 R, are associated with a notably poor prognosis. This analysis provides useful information to guide clinical care and to focus research on the cellular and molecular mechanisms for neutropenia and leukemogenesis in these patients [106].
Shwachman–Diamond Syndrome
Shwachman–Diamond syndrome is an autosomal recessive disorder, with an incidence estimated at 1 in 50,000 births, characterized by ineffective hematopoiesis, exocrine pancreatic dysfunction, and metaphyseal dysostosis, and an increased risk of leukemia [107]. Typically, patients with Shwachman–Diamond syndrome present in the first year of life with diarrhea and failure to thrive. In addition to pancreatic insufficiency these patients uniformly develop neutropenia. About 60% of patients are malnourished and short in stature and many also exhibit ichthyotic skin rashes. Shwachman–Diamond syndrome is also associated with other clinical findings including microcephaly, hypertelorism, retinitis pigmentosa, syndactyly, cleft palate, dental dysplasia, skin pigment defects, and myocardial fibrosis [108]. Leukemic transformation has been known to occur. Patients are predisposed to skin infections and pneumonia as a result of the neutropenia. Supportive measures for patients with Shwachman–Diamond syndrome include pancreatic enzymes, antibiotics, transfusions, and granulocyte colony-stimulating factor. The only definitive therapy is bone marrow transplantation.
Boocock and colleagues reported a causal mutation in the SBDS gene (named after Shwachman–Bodian–Diamond syndrome) [109]. Approximately 90% of Shwachman–Diamond syndrome patients have biallelic mutations in the SBDS gene. The structure and function of the SBDS gene has not been determined, but accumulating evidence suggests that the gene plays a role in ribosome biosynthesis and RNA processing [110]. Shwachman–Diamond syndrome cells exhibit abnormal expression of multiple genes involved in ribosome biogenesis and rRNA and mRNA processing and to have decreased expression of several ribosomal protein genes involved in cell growth and survival [111]. Additionally, SBDS has been shown to co-sediment with the 60S ribosomal precursor subunit in sucrose gradients and to associate with the 28S rRNA that is a component of the 60S subunit [110]. Although these findings provide evidence for a role of SBDS in ribosome biogenesis, SBDS is a multifunctional protein and may contribute to non-ribosomal activities that play a role in the clinical phenotype. SBDS genotyping may be used to confirm the definitive diagnosis.
Reticular Dysgenesis
Reticular dysgenesis, also called congenital aleukocytosis, is characterized by severe neutropenia associated with leukopenia, presence of rudimentary thymic lymphoid and splenic tissue, and agammaglobulinemia [112]. Histological examination of the bone marrow, spleen, and lymphoid tissue reveals normal reticular structure with normal erythroid and megakaryocyte elements, but with absent or sparse myeloid cells. Bacterial and viral infections occur early in life and are severe. Aggressive antibiotic therapy and supportive care are necessary for survival. Treatment with G-CSF and granulocyte-macrophage colony-stimulating factor (GM-CSF) has been ineffective. Bone marrow transplantation remains the only long-term treatment option available for infants with this disorder [112, 113].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree