Neurologic symptoms commonly occur in oncology patients, and in some cases they may be the presenting symptom of malignancy. Cancer-related neurologic syndromes are rarely pathognomonic and must be differentiated from other benign or serious conditions. This article reviews common neuro-oncologic syndromes that may lead to urgent evaluation in the emergency department, including cerebral edema, altered mental status, seizures, acute stroke, leptomeningeal metastases, and paraneoplastic neurologic syndromes.
Neurologic disorders are a frequent cause of emergency department (ED) visits, subspecialty consultation, and hospital admissions in oncology patients. Neurologic disorders are often the presenting symptom of systemic cancer. In addition, neurologic complications are a source of significant disability, morbidity, and mortality in cancer patients. This article provides an overview of selected cancer-related neurologic emergencies that present to the ED, including cerebral edema and increased intracranial pressure, altered mental status, seizures, acute stroke, leptomeningeal metastases, and paraneoplastic neurologic syndromes.
Cerebral edema and increased intracranial pressure
As a brain tumor enlarges, it produces focal findings by invasion and compression of surrounding brain tissue. More generalized signs and symptoms, such as headache, nausea, vomiting, papilledema, and depressed levels of consciousness, result from increased intracranial pressure due to the space occupied by the tumor mass, associated cerebral edema, or obstruction of cerebrospinal fluid outflow pathways.
Vasogenic edema occurs as tumor growth leads to disruption of the blood-brain barrier and increased capillary permeability, which allows a protein- and sodium-rich plasma filtrate to enter the extracellular fluid space and spread throughout adjacent white matter. Increased hydrostatic pressure within the tumor, an osmotic gradient, and the absence of a lymphatic system within the central nervous system also lead to extracellular fluid accumulation. As a result, focal mass effect, increased intracranial pressure, compromise of local blood supply, or brain herniation syndromes may occur.
Headaches are reported at presentation by approximately one half of all brain tumor patients, especially those with rapidly growing neoplasms or infratentorial tumors. At first glance these headaches may seem nondescript, but there are characteristics of headache in this patient population that the ED triage team will find valuable. Brain tumor patients generally describe a dull nonthrobbing headache similar to a tension headache. The headache is mild at onset, becoming increasingly more severe over days and weeks, and is typically associated with other symptoms of increased intracranial pressure and focal neurologic deficits. In fact, less than 10% of brain tumor patients have isolated headache syndromes, making the presence of abnormal neurologic signs and symptoms an important diagnostic distinction between tumor-related and benign headaches. The classic brain tumor headache syndrome, characterized as a dull, aching pain that awakens the patient from sleep or is present on awakening with improvement thereafter, and often aggravated by positional change or Valsalva maneuvers, or associated with nausea and vomiting, is actually rare to nonexistent. Obstructive hydrocephalus is often associated with a more acute headache presentation and vomiting.
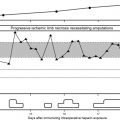
Patients with brain tumors may also experience headaches in conjunction with plateau pressure waves. Under normal circumstances, vasomotor tone automatically adjusts to maintain constant intracranial pressure with positional changes or other variables. However, in patients with brain tumors, mass effect and other factors can impede vasomotor autoregulation leading to plateau pressure waves that are characterized by the abrupt rapid elevation of intracranial pressure for brief 5- to 20-minute periods. This sudden change in intracranial pressure produces short duration (20–30 minutes) headaches that are precipitated by a change in posture, and are often accompanied by an abrupt decline in mental status and emesis. Level of alertness is generally unaffected, but loss of consciousness can occur. These symptoms may be confused with seizure activity in patients with a known diagnosis of brain tumor.
Altered mental status is the initial symptom or sign in one third of brain tumor patients. Disturbances range from psychomotor retardation to lethargy to obtundation and coma. Papilledema is noted in approximately 8% of malignant glioma patients at presentation. Most patients with papilledema do not report ocular symptoms, but some report transient visual obscurations or blurred vision. Visual acuity is generally unaffected. Early fundoscopic manifestations of papilledema include disc hyperemia, subtle edema of the nasal disc, small hemorrhages of the nerve fiber layer, and loss of spontaneous venous pulsations, which are normally present in 80% of the population. Later, the disc becomes grossly elevated, the margins obscure, and hemorrhage, exudates, and cotton wool spots may occur. Increased intracranial pressure may also cause vomiting, with or without nausea, as pressure is exerted on brain stem structures. Vague nonvertiginous dizziness is a frequent accompaniment. Projectile vomiting without nausea frequently occurs in patients with posterior fossa tumors and obstructive hydrocephalus.
Focal mass lesions can result in the asymmetric shift of brain contents from one intracranial compartment to another, producing herniation syndromes ( Table 1 ). False localizing signs are more commonly seen with slow growing neoplasms that produce prolonged elevation of intracranial pressure and chronic tissue shift. Acute herniation syndromes involving the medial temporal lobes (transtentorial herniation) or the cerebellar tonsils (tonsillar herniation), are often fatal and treatment outcomes, when successful, are poor. The earliest manifestation of transtentorial herniation is unilateral papillary dilatation and decrease in level of consciousness followed by ipsilateral or contralateral hemiparesis. Tonsillar herniation leads to compression of the respiratory centers in the medulla and ultimately respiratory arrest. Careful observation during recording of vital signs by the ED triage team may allow for the appreciation of warning signs of impending herniation such as abnormal breathing patterns (Cheyne-Stokes, central neurogenic hyperventilation, Biot’s breathing), repetitive respiratory reflexes (sighing, yawning, hiccups), and Cushing’s triad, which consists of bradycardia, hypertension, and change in respiratory pattern.
| Type of Herniation | Definition | Symptoms/Signs |
|---|---|---|
| Transtentorial herniation | ||
| Downward displacement of the brain through the tentorium at the level of the incisura |
|
| Upward displacement of brain through the tentorium at the level of the incisura |
|
| Subfalcine/cingulated herniation | Displacement of brain underneath the falx |
|
| Tonsillar herniation | Downward displacement of infratentorial brain through the foramen magnum |
|
| Sphenoid/alar herniation | Supratentorial brain displaced anteriorly or posteriorly over the wing of the sphenoid bone | Frequently asymptomatic |
| Temporal lobe displaced anteriorly and superiorly over the sphenoid bone | — |
| Frontal lobe is displaced posteriorly and inferiorly over the sphenoid bone | — |
| Extracranial herniation | Displacement of brain through a cranial defect | Herniated brain may become ischemic |
Currently there is no standard protocol or algorithm to guide the emergency medicine physician for the management of increased intracranial pressure or brain herniation. Likewise, there is a paucity of prospective clinical trial data on which to base management. General treatment approaches are contingent on rapidity and severity of neurologic symptoms, and vary widely from institution to institution. In some cases, medical management may reverse herniation syndromes, or serve to temporarily stabilize the patient until surgical decompression is possible.
Corticosteroids
Glucocorticoids, in particular dexamethasone, play a major role in the management of symptomatic cerebral edema. Approximately 70% to 80% of brain tumor patients will experience symptom improvement following dexamethasone treatment. In nonemergent clinical situations, the daily dose of dexamethasone ranges from 6 mg to 24 mg and is typically divided into 2 to 4 doses. The long half-life of dexamethasone permits twice daily dosing, and the provision of 4 daily doses has become entrenched in current medical practice. In patients with impaired consciousness, rapidly progressing signs of increased intracranial pressure, or cerebral herniation, an intravenous bolus of dexamethasone (40–100 mg) followed by a maintenance dose of dexamethasone of 40 to 100 mg over 24 hours in divided doses may be effective in reversing symptoms. Concurrent provision of 20 mg of intravenous furosemide may further augment the effect of the steroid.
Physiologically, the first change after steroid administration is a decrease in plateau waves followed by a gradual decline in intracranial pressure over 48 to 72 hours. Symptomatic improvement can be seen within the first few hours of intravenous steroid therapy, and maximal clinical improvement is generally achieved within 24 to 72 hours. Evidence of generalized brain dysfunction typically improves before focal neurologic symptoms or signs. If the desired clinical response is not achieved within 48 hours of standard dexamethasone dosing, the dose can be doubled every 48 hours until clinical response or a total daily dose of 100 mg of dexamethasone is reached. The patient should then be maintained on the lowest dose necessary to maintain symptom control.
Hyperventilation
Intubation and hyperventilation to a target partial pressure of carbon dioxide (pCO 2 ) of 30 mm Hg remains the most rapid means of decreasing increased intracranial pressure. As the pCO 2 decreases, cerebral vasoconstriction in undamaged areas of the brain occurs, resulting in decreased cerebral blood volume and intracranial pressure. The benefit of hyperventilation manifests within 30 seconds and is maintained for about 15 to 20 minutes. Thereafter, a compensatory metabolic acidosis negates its effect. The primary usefulness of hyperventilation is to gain immediate control of intracranial pressure, allowing time for other treatment modalities to take effect.
Osmotherapy
Hyperosmolar agents create an osmotic gradient that effectively draws water from the extracellular space to the higher osmolarity in blood, thereby reducing brain volume and intracranial pressure. Historically, mannitol is the most commonly used osmotic agent; however, there is growing evidence in support of the use of hypertonic saline. Mannitol is typically provided as a 20% to 25% solution and given as a 0.5- to 2.0-g/kg intravenous loading dose. The effect of mannitol manifests within 15 to 30 minutes and is generally sustained for several hours. If clinically warranted repeated small intravenous boluses may be administered, however, repeated doses of mannitol may precipitate rebound intracranial hypertension. The provision of a loop diuretic such as furosemide given 15 to 20 minutes after mannitol as a one time 20-mg intravenous dose may augment the benefit of mannitol. Hypertonic saline at concentrations ranging from 3% to 23.4% seems to be as effective if not superior to mannitol with a more favorable side effect profile. However, unlike mannitol, hypertonic saline is a significant vesicant, which should be preferentially infused into a central line.
Adjunct Therapies
Additional adjuncts to the management of increased intracranial pressure and acute herniation syndromes include elevation of the head, propofol or pentobarbital anesthesia, and hypothermia. Elevation of the head by 30 degrees with care to avoid flexion or extension of the neck maximizes venous outflow. Propofol induces vasoconstriction and decreases the cerebral metabolic rate of oxygen, which in turn reduces cerebral blood flow, cerebral blood volume, and intracranial pressure. Barbiturates also suppress cerebral metabolism, which subsequently decreases cerebral blood flow and cerebral blood volumes. Hypothermia can reduce the cerebral metabolism rate of oxygen by 5% per degree reduction in core body temperature, thereby decreasing cerebral blood flow and intracranial pressure. However, increased risk of cardiac dysrhythmias, coagulopathy, and systemic infection limit its usefulness.
Altered mental status
Delirium
Delirium occurs in 25% to 40% of patients with cancer, and is present in up to 90% of terminally ill cancer patients. Delirium, often used synonymously with acute confusion, is the most common cause of neurologic consultation in cancer patients, and results in upwards of 10% of admissions to general oncology wards. The syndrome is characterized by rapid onset over hours or days of fluctuating abnormalities of thought, perception, and levels of awareness. More specifically, decreased attention and disorganized thinking are accompanied by variable altered level of consciousness, disorientation, decreased short term memory, hallucinations or illusions, alteration of sleep-wake cycle, and abnormal behavior modulation. Mood and behavior changes are often the primary outward manifestation of delirium. Patients may exhibit loud, boisterous, aggressive, and agitated behavior, or alternatively may have quiet, reserved, and passive behavior, and appear depressed. Brief simplistic psychotic ideas are commonly present, and neurologic signs such as unsteady gait and tremor may be seen.
Delirium often goes unrecognized, or may be confused with dementia, depression, psychoses, seizures, or attributed erroneously to terminal illness. In addition, it is consistently associated with more numerous and longer hospital stays, and increased morbidity and mortality.
Delirium remains a clinical diagnosis. Although various instruments or assessment tools have been developed to screen patients for delirium, they remain largely unvalidated, unstudied, and unused in patients with cancer. Key to recognition of delirium is a clear understanding of the patient’s baseline cognitive functioning, as well as critical assessment of ongoing symptoms, which may require ancillary history from family members or other caregivers. In addition, a high index of suspicion, and awareness of associated risk factors and etiologies of delirium in the cancer patient is required of the ED team.
Delirium may result from direct and indirect effects of cancer and its treatment on the central nervous system. Multiple precipitating factors were identified in more than 60% of cancer patients with delirium, with a median number of 3 probable causes per patient. The most common causes of delirium in the cancer patient included drugs, systemic infection, structural brain lesions, and metabolic dysfunction. Metabolic aberrations included hyponatremia, hypoxia or hypoperfusion, and renal failure. Cancer type and chemotherapy were not generally contributing factors. In one report, low albumin levels were found in 80% of patients, but cachexia was not recorded and the extent of malnutrition was not known. Similar to reports in noncancer patients, surgical procedures precipitated delirium in up to 40% of patients. Likewise, infection was a strong risk factor for delirium, but it rarely occurred in isolation. Data from elderly, noncancer patients found that delirium, not an elevated temperature, was frequently the first sign of sepsis. Nonconvulsive status epilepticus (NCSE) may be an under-recognized cause of delirium in comatose patients.
It is critical that the emergency medicine physician appreciates that delirium is reversible with appropriate intervention in more than 50% of patients. Moreover, meaningful functional improvement can be seen in patients with advanced cancer if any reversible contributing factors are treated. Reversible precipitants of delirium include opioid and nonopioid psychoactive medications, dehydration, infection, surgical procedures, structural brain abnormalities, and NCSE. Rapid improvement is frequently seen in patients with brain tumors or hemorrhagic metastases after administration of corticosteroids, which is often initiated in the ED.
With few exceptions, the diagnostic evaluation of delirium in cancer patients does not differ from that routinely undertaken in noncancer patients. Neuroimaging is indicated in most cancer patients with delirium including those with a nonfocal examination, the exception being patients who rapidly clear following a medical intervention. Notably, lateralizing signs are absent in one fourth of patients with delirium and a structural brain lesion on neuroimaging. Electroencephalography is indicated in comatose or significantly clouded patients; the reported incidence of NCSE in these patients is 6% to 8%. In addition, because 3 or more contributory factors are often present, the diagnostic workup should not be truncated after the identification of one reasonable cause of delirium.
Overall, delirium is a poor prognostic factor in cancer patients. Statistically significant decreases in median survival are reported in cancer patients with delirium compared with those without delirium, especially if the acute confusion is attributable to structural brain lesions or multiple toxic or metabolic abnormalities.
Nonconvulsive Status Epilepticus
NCSE has been reported to be the underlying cause of altered mental status in up to 6% of cancer patients. A high index of suspicion is required for the diagnosis of NCSE, in part due to its variable and nonspecific presentation, its lack of associated motor activity, and the absence of a prior history of epilepsy or seizures in most patients at presentation. NCSE is classically defined as a state of continuous or intermittent seizure activity without return to baseline lasting at least 30 minutes. More recently, the Epilepsy Research Foundation defined NCSE as a range of conditions in which electrographic seizure activity is prolonged, resulting in nonconvulsive clinical symptoms.
The one consistent clinical symptom of NCSE is fluctuating altered mental status; however, even then, symptoms can encompass a spectrum ranging from psychomotor retardation to mild confusion to depressed consciousness. Motor manifestations are often limited to focal myoclonic jerks involving the face, eyelids, or extremities, however brief tonic or clonic movements of one or multiple extremities may also occur. Additional possible manifestations include head deviation, automatisms, and eye movement abnormalities including hippus, nystagmoid eye movements, repeated blinking, and persistent eye deviation. In one prospective study, the combination of a remote risk factor for seizures (previous stroke, neurosurgical procedure, brain tumor, or history of meningitis) and ocular movement abnormalities on neurologic examination had 100% sensitivity for NCSE, but low specificity.
In some cases, imaging findings may support the diagnosis of NCSE. Characteristic cortical ribbon hyperintensity on long repetition time (TR)-weighted magnetic resonance sequences or diffusion weighted imaging sequences, with or without leptomeningeal enhancement was reported in 4 of 8 patients with NCSE in one series. Imaging findings did not respect vascular territories, lacked mass effect, and either resolved or improved on follow-up imaging studies.
Emergent electroencephalography (EEG) is recommended for patients with suspected NCSE. If an emergent EEG is not possible, an empirical trial of intravenous lorazepam should be considered given the tolerable risk of lorazepam compared with the benefit of potential prevention of secondary cerebral damage.
Altered mental status
Delirium
Delirium occurs in 25% to 40% of patients with cancer, and is present in up to 90% of terminally ill cancer patients. Delirium, often used synonymously with acute confusion, is the most common cause of neurologic consultation in cancer patients, and results in upwards of 10% of admissions to general oncology wards. The syndrome is characterized by rapid onset over hours or days of fluctuating abnormalities of thought, perception, and levels of awareness. More specifically, decreased attention and disorganized thinking are accompanied by variable altered level of consciousness, disorientation, decreased short term memory, hallucinations or illusions, alteration of sleep-wake cycle, and abnormal behavior modulation. Mood and behavior changes are often the primary outward manifestation of delirium. Patients may exhibit loud, boisterous, aggressive, and agitated behavior, or alternatively may have quiet, reserved, and passive behavior, and appear depressed. Brief simplistic psychotic ideas are commonly present, and neurologic signs such as unsteady gait and tremor may be seen.
Delirium often goes unrecognized, or may be confused with dementia, depression, psychoses, seizures, or attributed erroneously to terminal illness. In addition, it is consistently associated with more numerous and longer hospital stays, and increased morbidity and mortality.
Delirium remains a clinical diagnosis. Although various instruments or assessment tools have been developed to screen patients for delirium, they remain largely unvalidated, unstudied, and unused in patients with cancer. Key to recognition of delirium is a clear understanding of the patient’s baseline cognitive functioning, as well as critical assessment of ongoing symptoms, which may require ancillary history from family members or other caregivers. In addition, a high index of suspicion, and awareness of associated risk factors and etiologies of delirium in the cancer patient is required of the ED team.
Delirium may result from direct and indirect effects of cancer and its treatment on the central nervous system. Multiple precipitating factors were identified in more than 60% of cancer patients with delirium, with a median number of 3 probable causes per patient. The most common causes of delirium in the cancer patient included drugs, systemic infection, structural brain lesions, and metabolic dysfunction. Metabolic aberrations included hyponatremia, hypoxia or hypoperfusion, and renal failure. Cancer type and chemotherapy were not generally contributing factors. In one report, low albumin levels were found in 80% of patients, but cachexia was not recorded and the extent of malnutrition was not known. Similar to reports in noncancer patients, surgical procedures precipitated delirium in up to 40% of patients. Likewise, infection was a strong risk factor for delirium, but it rarely occurred in isolation. Data from elderly, noncancer patients found that delirium, not an elevated temperature, was frequently the first sign of sepsis. Nonconvulsive status epilepticus (NCSE) may be an under-recognized cause of delirium in comatose patients.
It is critical that the emergency medicine physician appreciates that delirium is reversible with appropriate intervention in more than 50% of patients. Moreover, meaningful functional improvement can be seen in patients with advanced cancer if any reversible contributing factors are treated. Reversible precipitants of delirium include opioid and nonopioid psychoactive medications, dehydration, infection, surgical procedures, structural brain abnormalities, and NCSE. Rapid improvement is frequently seen in patients with brain tumors or hemorrhagic metastases after administration of corticosteroids, which is often initiated in the ED.
With few exceptions, the diagnostic evaluation of delirium in cancer patients does not differ from that routinely undertaken in noncancer patients. Neuroimaging is indicated in most cancer patients with delirium including those with a nonfocal examination, the exception being patients who rapidly clear following a medical intervention. Notably, lateralizing signs are absent in one fourth of patients with delirium and a structural brain lesion on neuroimaging. Electroencephalography is indicated in comatose or significantly clouded patients; the reported incidence of NCSE in these patients is 6% to 8%. In addition, because 3 or more contributory factors are often present, the diagnostic workup should not be truncated after the identification of one reasonable cause of delirium.
Overall, delirium is a poor prognostic factor in cancer patients. Statistically significant decreases in median survival are reported in cancer patients with delirium compared with those without delirium, especially if the acute confusion is attributable to structural brain lesions or multiple toxic or metabolic abnormalities.
Nonconvulsive Status Epilepticus
NCSE has been reported to be the underlying cause of altered mental status in up to 6% of cancer patients. A high index of suspicion is required for the diagnosis of NCSE, in part due to its variable and nonspecific presentation, its lack of associated motor activity, and the absence of a prior history of epilepsy or seizures in most patients at presentation. NCSE is classically defined as a state of continuous or intermittent seizure activity without return to baseline lasting at least 30 minutes. More recently, the Epilepsy Research Foundation defined NCSE as a range of conditions in which electrographic seizure activity is prolonged, resulting in nonconvulsive clinical symptoms.
The one consistent clinical symptom of NCSE is fluctuating altered mental status; however, even then, symptoms can encompass a spectrum ranging from psychomotor retardation to mild confusion to depressed consciousness. Motor manifestations are often limited to focal myoclonic jerks involving the face, eyelids, or extremities, however brief tonic or clonic movements of one or multiple extremities may also occur. Additional possible manifestations include head deviation, automatisms, and eye movement abnormalities including hippus, nystagmoid eye movements, repeated blinking, and persistent eye deviation. In one prospective study, the combination of a remote risk factor for seizures (previous stroke, neurosurgical procedure, brain tumor, or history of meningitis) and ocular movement abnormalities on neurologic examination had 100% sensitivity for NCSE, but low specificity.
In some cases, imaging findings may support the diagnosis of NCSE. Characteristic cortical ribbon hyperintensity on long repetition time (TR)-weighted magnetic resonance sequences or diffusion weighted imaging sequences, with or without leptomeningeal enhancement was reported in 4 of 8 patients with NCSE in one series. Imaging findings did not respect vascular territories, lacked mass effect, and either resolved or improved on follow-up imaging studies.
Emergent electroencephalography (EEG) is recommended for patients with suspected NCSE. If an emergent EEG is not possible, an empirical trial of intravenous lorazepam should be considered given the tolerable risk of lorazepam compared with the benefit of potential prevention of secondary cerebral damage.
Seizures
New onset seizures herald the diagnosis of central nervous system brain tumors in 20% to 40% of patients, and account for 10% to 15% of adult-onset seizures. Furthermore, seizures occur at some point in the clinical course in 40% to 60% of patients with gliomas, in 30% to 40% of patients with brain metastases, and in approximately 13% of all cancer patients. Seizure risk varies depending on the tumor type and location, patient age, and tumor treatment. Slow-growing tumors that involve or abut the cerebral cortex are associated with a higher incidence of seizures.
In many cases, a clinical diagnosis of seizure is established after the patient history and examination is performed. However, disorders such as syncope, migraine, medication effects, and nonepileptic spells, may be confused with seizures. In addition, the diagnosis of NCSE is often overlooked in the ED. Head computed tomography (CT) and routine EEG should be considered as part of the neurodiagnostic evaluation of adult patients with unprovoked first seizure in the emergency department. Brain imaging results in an acute management change in approximately 10% to 15% of these patients and EEG demonstrates significant abnormalities in approximately one third of patients, and provides risk assessment for seizure recurrence.
Seizures associated with brain tumors and other structural lesions are most often simple partial or complex partial seizures. Secondarily generalized seizures may occur, but the focal onset of these seizures often goes unnoticed by the patient or witnesses. Postictal deficits (Todd’s paralysis) are more common in patients with structural brain lesions and may be prolonged. Whereas convulsive status epilepticus is rare in patients with brain tumors, it is fatal in 6% to 35%. In contrast to structural seizures in brain tumor patients, seizures related to metabolic abnormalities are typically generalized seizures. Standard of care diagnostic evaluation and seizure management is appropriate in the brain tumor patient with the following specific considerations.
Many physicians endorse the prophylactic use of anticonvulsant medications in brain tumor patients who have never had a seizure, citing the high frequency of seizures in this patient population and the low risk of seizure medications. However, the emergency medicine physician must appreciate the lack of evidence that prophylactic anticonvulsant medications will prevent seizures in these patients, and that seizure medications are not without potential side effects and drug interactions. Phenytoin, a commonly prescribed anticonvulsant medication, causes a morbilliform rash in approximately 20% of brain tumor patients. Stevens-Johnson syndrome is rare, but is seen more often with the combination of radiation therapy, steroid taper, and phenytoin. Even minor side effects of antiepileptic drug can negatively impact quality of life of patients already undergoing aggressive antitumor therapy. In addition, enzyme-inducing anticonvulsant medications may interact with chemotherapy and other drugs. For this reason, the use of nonenzyme-inducing anticonvulsant medications is preferable. Practice parameters issued by the American Academy of Neurology (AAN) currently recommend withholding prophylactic anticonvulsants in brain tumor patients who have never had a seizure.
A related issue is the provision of prophylactic anticonvulsant medications in the setting of neurosurgical procedures. Traditionally, neurosurgeons prescribe prophylactic anticonvulsant medications before and for 6 to 12 weeks after neurosurgical procedures. The AAN practice guidelines recommend the tapering and discontinuance of anticonvulsant medications after the first postoperative week in brain tumor patients without known seizures.
The etiology of provoked seizures in cancer patients is similar to that of the general population. However, some causes are particularly linked to cancer therapies. One such example is reversible posterior leukoencephalopathy syndrome (RPLS), also known as posterior reversible encephalopathy syndrome. RPLS in cancer patients is associated with numerous chemotherapeutic agents, especially cisplatin. RPLS has also been reported following the administration of 5-fluorouracil, bleomycin, vinblastine, vincristine, etoposide, paclitaxel, ifosfamide, cyclophosphamide, doxorubicin, cytarabine, methotrexate, oxaliplatin, and bevacizumab.
The classic presentation of RPLS is the development of a subacute syndrome of headache, altered consciousness, generalized seizures, and visual disturbances, occurring in conjunction with posterior cerebral white matter vasogenic edema on CT/MRI. Typically the syndrome manifests over several days, but a more acute presentation may occur. Altered consciousness may vary from excessive drowsiness to coma, seizures may be focal or generalized, and visual disturbances range from blurred vision to cortical blindness. Additional neurologic symptoms such as paresis may also be present. Moderate to severe hypertension occurs in approximately 75% of patients. Hypertension typically develops at the same time as neurologic symptoms, but occasionally it may precede the clinical manifestations of RPLS.
Radiographically, MRI typically demonstrates symmetric hemispheric edema in the parietal and occipital lobes involving cortical and subcortical white matter, approximating the border zone vascular territory. Although involvement of the parietal and occipital lobes occurs most often, similar radiographic abnormalities can be located in the frontal lobes, the inferior temporal-occipital junction, and the cerebellum. Focal areas of restricted diffusion are seen in less than one fourth of patients. Approximately 15% of patients have radiographic evidence of hemorrhage in the form of focal hematoma, or isolated sulcal or subarachnoid blood.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree