Interpreting the case study results
Some of the blood test results for the patient in the case study are out of range. We will work through the following questions in order to interpret these results:
•What values are abnormal for the condition?
•What would the blood tests from a typical RA patient look like?
•Why have these blood tests been requested?
Finally, we will apply the strategy.
What values are abnormal or typical for the condition?
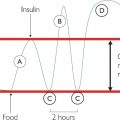
An initial observation is that some conditions (like RA) can be cyclical, and the blood tests may not always match the clinical symptoms (see Test 2). Yet these false negatives could be problematic if this was a one-off blood test.
Looking at the values that are abnormal, we can make the following observations.
The white cell count is high. This count is raised in response to inflammation caused by an autoimmune response, some blood cancers and infection. The values observed, the duration of the condition and the presenting symptoms rule out a bacterial or viral infection. Given that red blood cell count (RBC) and platelet production is normal, a bone marrow dysfunction (leukaemia or myeloma) is unlikely. Hence these values are consistent with RA.
The neutrophils are high. Neutrophil numbers increase in response to sustained production of chemoattractants (which attract cells) like C-reactive protein (CRP) and TNF-alpha. CRP is raised relative to inflammation. Inflammation is cellular damage. Therefore CRP will rise in an autoimmune response through to severe burns and trauma. In practice, neutrophil increase is associated with bacterial infection, which causes inflammation and an increase in CRP. Neutrophils directly destroy the bacteria in the blood. In the case study, CRP and neutrophil values, the timeframe of the tests (one year) and presenting symptoms make a bacterial infection unlikely. The values are therefore consistent with an autoimmune response.
The haematocrit (percentage of red blood cells in the whole blood) is low. However, there are no symptoms of anaemia, the value is very close to the reference range 0.353 (low range 0.360) and crucially it doesn’t fit with the other markers of red cell status. RBC and haemoglobin (Hb) are both normal. The value is not changing over time. A false positive is likely, and the result could be described as ‘not clinically significant at this time’.
Plasma viscosity (PV) is high. PV is a marker of ‘extra stuff’ in the blood. In this case, it is raised due to increased white cells (neutrophils) and globulins (antibodies).
Globulins are raised. Globulins are a crude, surrogate measure of antibody production. The globulin count is raised when antibodies are produced, and antibodies are produced by B cells (a type of lymphocyte). Globulin increases in viral infections (a normal response by the lymphocytes to infection). But the case study patient’s lymphocytes are normal and she has no symptoms. The globulins are raised in a myeloma (dysfunctional B cells), but again the lymphocyte count and globulin value make a diagnosis of myeloma unlikely. (A Bence Jones protein or electrophoresis band will confirm.) Globulins are often raised in an autoimmune response. Because the body makes antibodies to ‘itself’, this will not usually increase the lymphocyte count (as would be seen if the antibodies were being produced against a large viral infection, driving up lymphocyte number and antibody production).
Why have these blood tests been requested?
This woman is typical of the patients encountered in practice – she has several different conditions, for which she is taking several types of medication. Looking at the long list of tests can be overwhelming and confusing. A useful strategy is to split the blood tests into a ‘hierarchy of conditions’ and discuss which ones require red flags (to be actioned quickly), referrals, interventions and repeat tests.
To monitor RA, the white cell count, neutrophils, PV, CRP and globulins have been requested. Any significant change in these values could indicate an additional bacterial infection. Thus, this suite of blood tests may be monitored by the secondary care specialist consultant for RA and by the primary care practitioner for additional infections.
To monitor the effects of methotrexate, two suites have been requested: LFTs, U&Es and FBC (red cell markers). Methotrexate can be toxic to some patients and the LFT panel will provide a red flag if this is the case. This also explains why the patient has a blood test every four weeks.
Methotrexate works in autoimmune conditions by restricting folate availability in the blood. Folate (folic acid) is the ‘currency’ the cells use to replicate (multiply) and grow (hence methotrexate’s use as an anti-cancer therapy). Long-term restriction of folate can lead to macrocytic (high red cell volume) anaemia because red blood cell lifespan is only 12 weeks. To monitor this long-term predisposition to anaemia, RBC, Hct, Hb and MCV are measured regularly.
As a differential diagnosis, platelets (and RBC) are measured for possible bone marrow dysfunction, which could be masked by increased white cells in the autoimmune response.
U&Es are measured as a general marker of kidney function; and potassium is a red flag for a cardiac event. As a differential for anaemia, is any possible anaemia linked to renal insufficiency? Finally, U&Es are measured (in the case study) as a differential diagnosis for the LFTs. Some liver enzymes, like alkaline phosphatase (Alk Phos or ALP), are also found in the kidney. A raised ALP and normal U&Es can quickly indicate that the liver is the likely origin and cause for investigation.
Applying the strategy
Let’s think about family groups and the four questions to apply to these results.
The initial family group in the FBC, and a great place to start with any blood test, is Hb for red blood cells, then white cells, then platelets.
•Look at Hb – this is in range.
•Now look at Hb’s two mates (red cell indices), HCT and RBC. The only one out of range is HCT.
Now let’s apply the four questions to HCT:
•How far out of range is it? Not very. It’s borderline. In fact it’s been borderline for some time and is often in range normal.
•Is the patient symptomatic? No.
•Is this an important blood test? No, the HCT result doesn’t usually change the management of the patient.
•What do its mates say? Well, RBC and Hb are both in range so they don’t support HCT.
•We will therefore ignore HCT as a false positive.
Next, check platelets:
•They are in range so the bone marrow is likely to be working OK.
Next, look at the WBC:
•The WBC is out of range – elevated.
•What type of WBC is causing this increase? Neutrophils.
•What switches on neutrophils? CRR
•CRP is also out of range in a group (CDL), which is commensurate with autoimmune.
Now look at the four questions for the white cells:
•Are they far out of range? Yes.
•Does the patient have symptoms? Yes.
•Family group? Yes (WBC, neutrophils, CRP).
•Is this an important result? Yes.
Finally, mop up any additional bloods, such as globulin:
•Globulin measures antibodies so this could be due to a viral infection.
•But the lymphocytes (the WBC that fight viral infection) are not raised.
•The CRP isn’t high enough, and the patient doesn’t really have the expected symptoms.
•So the rise in globulins is much more likely to be caused by the presence of auto-antibodies, as seen in autoimmune (which this patient has).
•We only measured liver function because the patient is on a drug called methotrexate which can be toxic to the liver.
•So we now note the globulin result, which is actually nothing to do with the liver (as discussed).
To summarise, all the bloods (apart from HCT) are fairly ‘normal’ for a patient with rheumatoid arthritis (RA) and we can ignore the HCT as a false positive.
Self-assessment
Work through some case studies in your own setting and apply the four questions, family groups, input and output, and think about the four ways in which blood can change.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree