Carcinoma of the Follicular Epithelium: Surgical Therapy
Gregory W. Randolph
Gerard M. Doherty
Introduction
The management strategy for follicular cell-derived thyroid carcinoma includes operation for nearly all patients, as well as radioiodine therapy and thyroid hormone therapy administration. The operative portion of the strategy is important because of two related issues: It dictates the course and options for the radioiodine and thyroid hormone therapies, and it has the potential to cause significant life-changing adverse effects.
Extent of Thyroidectomy for Possible Thyroid Cancer
The assessment of patients with a solitary or multiple thyroid nodules is considered elsewhere (see Chapters 48 and 49). In particular, thyroid resection that leaves a substantial portion of the ipsilateral lobe in place can create difficult decisions if the definitive diagnosis is malignant. Much of the decision-making for diagnostic procedures is based upon cytology, and the risk of malignancy. Some parameters other than cytology can importantly affect the decision to operate and the extent of thyroidectomy. These include age of the patient (higher malignancy risk <20 and >60), gender (males have increased risk of malignancy), family history of thyroid malignancy syndromes such as Familial Papillary Carcinoma, Cowden’s Syndrome, MEN 2A or 2B, personal history of exposure to ionizing radiation especially as a child and history of a rapidly growing thyroid mass (1). Size, firmness, and fixation of the nodule, presence of additional nodules, lymphadenopathy, and vocal cord paralysis (VCP) must all be assessed in the initial physical evaluation that may include ultrasound and should include laryngoscopy. TSH elevation and some ultrasonographic findings
(including solidness, irregular margins, microcalcification, central blood flow, taller than wide morphology, and increased elastography measures of firmness and density) are associated with a higher likelihood of malignancy and may thus influence the extent of the initial diagnostic procedure (2,3). Molecular assessment of the fine needle aspiration cytology (including assessment for BRAF, RET-PTC, RAS, PAX8/PPAR Gamma, and immunohistochemical staining for galectin 3) will likely significantly impact malignancy risk assessment in the future once more definitive experience with these tests is available. Cytopathologic analysis interpreted in the context of the other key clinical parameters is important in the decision to operate and in discussions of the extent of thyroidectomy. In general, no less than a total thyroid lobectomy is appropriate, and the more likely a lesion is to be a cancer, the greater should be the consideration for total thyroidectomy.
(including solidness, irregular margins, microcalcification, central blood flow, taller than wide morphology, and increased elastography measures of firmness and density) are associated with a higher likelihood of malignancy and may thus influence the extent of the initial diagnostic procedure (2,3). Molecular assessment of the fine needle aspiration cytology (including assessment for BRAF, RET-PTC, RAS, PAX8/PPAR Gamma, and immunohistochemical staining for galectin 3) will likely significantly impact malignancy risk assessment in the future once more definitive experience with these tests is available. Cytopathologic analysis interpreted in the context of the other key clinical parameters is important in the decision to operate and in discussions of the extent of thyroidectomy. In general, no less than a total thyroid lobectomy is appropriate, and the more likely a lesion is to be a cancer, the greater should be the consideration for total thyroidectomy.
Goals of Operation for Papillary Carcinoma of the Thyroid
While the specifics of resection for papillary thyroid carcinoma are individualized, the principles of cancer therapy apply for all patients. As outlined in the ATA Guidelines, the goals of initial surgical therapy are these (4):
To remove the primary tumor, disease that has extended beyond the thyroid capsule, and involved cervical lymph nodes. Completeness of surgical resection is an important determinant of outcome, while residual metastatic lymph nodes represent the most common site of disease persistence/recurrence.
To minimize treatment-related morbidity. The extent of surgery and the experience of the surgeon both play important roles in determining the risk of surgical complications.
To permit accurate staging of the disease. Because disease staging can assist with initial prognostication, disease management, and follow-up strategies, accurate postoperative staging is a crucial element in the management of patients with differentiated thyroid cancer.
To facilitate postoperative treatment with radioactive iodine, where appropriate. For patients undergoing radioiodine remnant ablation, or radioiodine treatment of residual or metastatic disease, removal of all normal thyroid tissue is an important element of initial surgery. Near total or total thyroidectomy also may reduce the risk for recurrence within the contralateral lobe.
To permit accurate long-term surveillance for disease recurrence. Both radioiodine whole body scanning and measurement of serum thyroglobulin are affected by residual normal thyroid tissue. Where these approaches are utilized for long-term monitoring, near-total or total-thyroidectomy is required.
To minimize the risk of disease recurrence and metastatic spread. Adequate surgery is the most important treatment variable influencing prognosis, while radioactive iodine treatment, TSH suppression, and external beam irradiation each play adjunctive roles in at least some patients.
Explicit understanding and consideration of these goals in the operative planning for each patient helps to frame the decision-making regarding the extent of operation appropriate for each person with thyroid carcinoma.
Imaging Prior to Operation for Papillary Carcinoma of the Thyroid
Given the importance of defining the extent of disease and customizing an operation for each person with thyroid carcinoma, preoperative imaging fills a crucial role in treatment planning. Both the ATA and NCCN Guidelines now include preoperative ultrasound examination specifically to evaluate for lymphadenopathy in the lateral neck in order to allow inclusion of those areas in the operative plan. Though prophylactic lymphadenectomy in the lateral neck is not recommended, removal of palpable or imageable disease is recommended.
Ultrasound examination is widely available, highly sensitive, low risk and low cost, and so it has become the cervical imaging modality of choice for most thyroid carcinoma. However, there are limitations of ultrasound, especially for bulky disease or for disease that extends posterior to the sternum or clavicles. For these situations, cross-sectional imaging with CT scan or MRI including intravenous contrast can be very helpful and is recommended.
Extent of Thyroidectomy for PTC >1 cm
The extent of thyroidectomy for patients with especially low-risk PTC has been actively debated for decades fueled by the prolonged long-term survival of the vast majority of patients with PTC and the possibility of higher complication rates with more extensive operations. Although well-differentiated thyroid carcinoma (WDTC) certainly can be a lethal disease, it is associated with prolonged survival in the vast majority of patients, and can be categorized as to risk based upon well-established criteria (Table 50C.1).
Table 50C.1 Key Factors in Various Prognostic Schemes | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||
There is recent important evidence from Bilimoria and coworkers, who studied a group of over 52,000 national cancer database patients with papillary carcinoma. They found, using Cox hazards modeling adjusting for age, race, income, lymph node status, distant metastasis, radioactive iodine use and year of diagnosis, that for lesions greater or equal to 1 cm, there is significant improvement in both survival and recurrence at 10 years with total thyroidectomy compared to less than total thyroidectomy (5). Recommendation 26 of the revised ATA guidelines of 2009 suggests total thyroidectomy is the preferred procedure for most patients with the preoperative diagnosis of PTC (4). Current NCCN guidelines also suggest total thyroidectomy for all patients with PTC except those with extremely favorable risk profiles (between 15 years and 45 years of age, no history of XRT, no distant metastasis, no cervical lymphadenopathy, no aggressive histology and size less than 4 cm) (6). Total thyroidectomy is also favored in most endocrinologist-published guidelines including those of the American Association of Clinical Endocrinology as well as European guidelines (7,8).
While the mainstream recommendation for total thyroidectomy characterizes most current treatment recommendations of endocrine organizations, one must acknowledge that extent
of surgery, especially for low-risk PTC has been studied for decades and that there exists an extensive past literature investigating both survival and recurrence both supporting (9,10,11,12,13,14,15,16,17,18,19,20,21,22) and negating (18,19,23,24,25,26,27,28,29,30,31,32,33) total thyroidectomy for PTC patients.
of surgery, especially for low-risk PTC has been studied for decades and that there exists an extensive past literature investigating both survival and recurrence both supporting (9,10,11,12,13,14,15,16,17,18,19,20,21,22) and negating (18,19,23,24,25,26,27,28,29,30,31,32,33) total thyroidectomy for PTC patients.
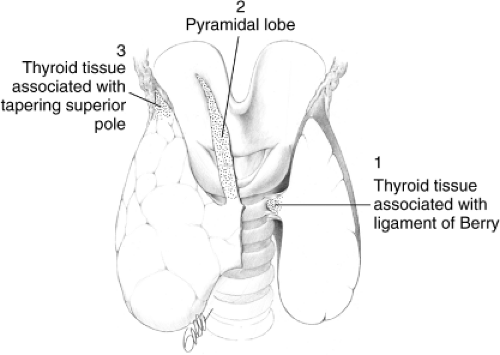 Figure 50C.1 Front view of thyroid and larynx, showing three areas that may contribute to thyroid bed radioactive iodine uptake after total thyroidectomy: 1, thyroid tissue associated with ligament of Berry; 2, thyroid tissue associated with unresected pyramidal lobe; 3, thyroid tissue associated with unrecognized tapering of the superior thyroid pole. (From: Randolph GW. Surgery of the Thyroid and Parathyroid Glands. Saunders, 2003 Philadelphia, with permission – Figure 22-4). |
Following total thyroidectomy, even in expert hands, a significant number of patients have residual thyroid tissue that requires postoperative ablation (see Fig. 50C.1) (34,35,36).
Surgical Complications
Surgical treatment must blend a thorough oncologic approach with a commitment to minimize the potential risk of complications (Table 50C.2). Certainly in skilled hands total thyroidectomy can be offered with low morbidity (73). However, “non-expert” surgeons perform 86% of routine thyroid surgery (74) and 50% of patients undergoing thyroid surgery in the US are performed by surgeons performing less than five thyroidectomies per year (75). Complications are more common in such patients (74).
Table 50C.2 Contemporary Thyroid Surgery Complications | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
Recurrent Laryngeal Nerve Paralysis
Permanent recurrent laryngeal nerve (RLN) paralysis rates in expert hands generally are in the 1% to 2% range (76). However, many reports reveal significantly higher rates, in the 6% to 8% range including rates as high as 23% (19,32,33). The reported prevalence of RLN injuries after thyroid surgery in fact varies widely. A recent analysis of 27 articles reviewing over 25,000 patients undergoing thyroidectomy found the average immediate postoperative VCP rate was 9.8%. The rate of permanent VCP varied 10-fold, according to the method of examining the larynx, and ranged from 0% to 18.6% (77). The Scandinavian quality register (SQR) for thyroid and parathyroid surgery, reporting results from 40 endocrine surgical units from Sweden and Denmark specializing in endocrine surgery, noted an immediate VCP rate of 4.3% (78). In the national UK British Association of Endocrine and Thyroid Surgeons (BAETS) audit, a VCP rate of 2.5% was found 79). Both Scandinavian and British quality registers derive from
surgeon-reported data without routine postoperative laryngeal exam. For the SQR, the rate of VCP doubled when patients were subjected to routine laryngeal exam as opposed to postoperative laryngoscopy that was performed only in patients with persistent and severe voice changes. Administrators of these two national databases deem the rates of temporary and permanent RLN palsy to be severely underestimated (78,79). Bilateral thyroidectomy is a unique offering in cervical procedures in that both left and right cranial nerves that innervate the airway introitus are subject to risk. Though extremely rare, bilateral nerve injury is a risk in every patient, and has the potential to require temporary or permanent tracheostomy.
surgeon-reported data without routine postoperative laryngeal exam. For the SQR, the rate of VCP doubled when patients were subjected to routine laryngeal exam as opposed to postoperative laryngoscopy that was performed only in patients with persistent and severe voice changes. Administrators of these two national databases deem the rates of temporary and permanent RLN palsy to be severely underestimated (78,79). Bilateral thyroidectomy is a unique offering in cervical procedures in that both left and right cranial nerves that innervate the airway introitus are subject to risk. Though extremely rare, bilateral nerve injury is a risk in every patient, and has the potential to require temporary or permanent tracheostomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree