Fig. 1
Four global maps illustrating the four main factors associated with the epidemiological profile of skin cancer in the tropics: (a) more intense ultraviolet radiation (http://www-med-physik.vu-wien.ac.at/uv/uv_online.htm); (b) a higher proportion of dark-skinned inhabitants (Reproduced from http://anthro.palomar.edu/vary/ by permission of Dennis O’Neil); (c) low incomes in association with limited healthcare resources (Illustrated with a map of the Human Development Index: World map indicating the categories of Human Development Index by country based on 2013 data; http://hdr.undp.org/en/2014-report); and (d) high biodiversity including oncogenic microbial pathogens (Illustrated by map of mammal diversity: Jenkins et al. [1]; http://biodiversitymapping.org/)
UV radiation is more intense in the tropics because the rays from the sun being perpendicular have a shorter path through the atmosphere and are therefore less absorbed by the atmosphere’s layers. In fair-skinned populations, the incidence of three major UV-induced cancers – basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma (MM) – increases with diminishing latitude.
Skin pigmentation varies substantially across human populations. In the skin, melanin acts as an optical and chemical photoprotective filter which reduces the penetration of UVR into epidermal and subepidermal tissues. Melanin is synthesized in melanosomes, which are distributed to keratinocytes by the dendritic processes of melanocytes. The superior photoprotection of highly melanized skin (dark skin) is due to the high density and distribution of melanosomes within keratinocytes in the epidermis. In 1988, Fitzpatrick describes a scale of 6 phototypes that takes into account both the color of the skin, the susceptibility to sunburn, and the ability to tan after exposure to UVR [2]. Individuals with phototype I (generally with red hair) and II (generally with blond hair and blue eyes) tan little or not at all. The risk of photo-induced skin cancer is very high. People with phototypes III (generally brown hair) and IV (generally dark hair, brown eyes) tan easily. Sunburns are rare. Individuals with skin types V and VI have, respectively, brown or black skin, tan deeply, and rarely or never burn. Relationship between skin pigmentation in indigenous human populations and latitude is traceable to the strong correlation between skin color and UV radiation intensity. The clinal gradation of skin coloration observed among indigenous peoples is correlated with UV radiation levels and represents a compromise solution to the conflicting physiological requirements of photoprotection and vitamin D synthesis [3].
Low- and middle- income countries predominate in the tropics. Limited healthcare resources and limited access to healthcare are very frequent. The main consequences are diagnostic delays, imprecise diagnoses, and limited therapeutic means. As with other cancers, limited access to pathological examinations, radiotherapy, and chemotherapy complicates the management. However, more than other cancer types, skin cancers can be diagnosed early by clinical examination and can in most cases be treated with surgery under local anesthesia.
Viral infectious agents are responsible for primary cutaneous cancers or cancers with cutaneous focus more often in low latitudes than in high latitudes. The main viruses involved are HHV8, oncogenic HPVs, HIV, and HTLV-1.
2 Epidemiology of Skin Cancer in the Tropics
Despite their frequency, BCC and SCC are not usually recorded by cancer registries due to their high frequency and low to very low case fatality rate. However, it is estimated that the five most common skin cancers in the world are in decreasing order of frequency: BCC, SCC, MM, Kaposi sarcoma (KS), and cutaneous lymphomas. The geographical distribution of these skin cancers shows variations. The first three are most often UV induced, reaching extremely high standardized incidence rates in tropical and subtropical areas where people mostly have fair skin (phototypes I and II). In Australia, a partially tropical country where the population is mainly fair skinned, every year 80 % of new cancers are skin cancers, especially BCC and SCC, respectively, 20 and 10 times more common than MM [4]. Nevertheless, MM is the fourth most common cancer in men (when excluding BCC and SCC) in Australia [4]. Table 1 summarizes and compares the Australian data and shows the influence of environmental ultraviolet radiation (latitude) and constitutional defense ability from ultraviolet radiation in white skin (tan ability) and black skin (indigenous, i.e., Australian Aborigines) [4–7].
Table 1
Age-standardized WHO incidence rates (per 100,000 in habitants/year) for the three principal skin cancers occurring in Australia and associated factors (latitude, skin type categories, ethnic group). Impact of environmental ultraviolet radiation (latitude) and constitutional defense ability from ultraviolet radiation in white skin (tan ability) and black skin (indigenous, i.e., Australian Aborigines)
BCC | SCC | MM | All cancersa except skin cancers | ||
|---|---|---|---|---|---|
884 | 387 | 40 | 313 | ||
High, nontropicalc | 547 | 232 | 36 | ||
Median, partially subtropicald | 959 | 432 | 47 | ||
Low, partially tropicale | 1,662 | 794 | 65 | ||
Skin type categoriesb [4] | Tans deeply | 585 | 215 | ||
Tans moderately | 722 | 319 | |||
Does not tan | 1,271 | 611 | |||
Ethnic groupf [7] | Indigenousg | 8 | |||
Non-Indigenous | 32 |
In people with dark skin, the incidence of all UV-induced skin cancer is considerably lower. Thus, in the tropics, the incidence of MM is very high among people with fair skin and low in patients with dark skin. The main location of MM is the sole of the foot in these populations from Africa, Asia, and among the Australian Aborigines. This is a variety of MM called acro-lentiginous melanoma (ALM), which is not photo-induced unlike the other forms of cutaneous MM [8].
Kaposi sarcoma (KS) is due to HHV-8, a virus of the herpes virus group, and its incidence increases dramatically when there is a coinfection with HIV. The incidence of KS is very high in countries where these two viral diseases exist simultaneously with high incidence rates. Thus, KS is the most common cancer in several East African countries [9, 10].
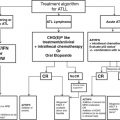
In the tropics, the most common lymphoma involving the skin are the adult T-cell leukemia/lymphoma (ATLL) associated with HTLV-1 and mycosis fungoides.
The dermatofibrosarcoma protuberans is rare but could be a bit more frequent in black skin.
3 Risk Factors and Pathogenesis
UV radiation is strongly associated with the three most frequent skin cancers: BCC, SCC, and MM. Schematically, UVB radiation can directly alter the DNA of epidermal cells, while the oncogenesis due to UVA radiation is more indirect. Spatiotemporal and meteorological factors affect the intensity of radiation: latitude, altitude, environment (sand, snow, water), time of day, period of the year, clouds, air humidity, ozone layer’s density, etc. Latitude is an important factor affecting the risk of photo-induced skin cancers; the greatest risk is in the tropics (see Table 1). The temporal profile of the UV radiation dose influences the type of cancer: acute intermittent exposures (with sunburn) are rather involved in BCC and superficial spreading melanoma (SSM), whereas chronic exposure is rather associated with SCC and lentigo maligna (LM). Individual and collective behavioral factors (work, leisure activities and sports, fashion, knowledge of the sunbeam’s risks, sunbed room) modulate exposure to UV radiation [11].
The pigmentation of the skin is mainly due to melanin. In the tropics, particularly in Africa, people with dark skin (phototypes V and VI) predominate. This dark pigmentation provides excellent protection against UV-induced cancers. This protection is abolished in melanocytic pathologies: genetic diseases like albinism or acquired diseases like vitiligo [12].
Age is a factor strongly associated with skin cancer, whether it is UV induced (BCC, SCC, MM) or not (classical or endemic KS). For UV-induced cancers, it is difficult to distinguish between the real influence of age and the cumulative dose of UV radiation-related to a longer exposure time. Overall incidence rises sharply from the fourth decade onward. In tropical regions, populations are generally young; with the demographic transition expected in the coming years, we may see an aging of the population which will cause increased incidence of skin cancer.
Sex is an important risk factor in KS (especially for non-HIV-associated forms with a sex ratio of around 10:1) and a relative factor concerning the location of MM (back in men, lower limbs in women). Moreover BCC and SCC are slightly more common among men (probably due to gender differences in exposure to the sun).
Genetic predisposition to skin cancer may exist. Some genetic diseases are accompanied by a specific gene mutation that constitutes a high-risk factor for skin cancer. This applies, for instance, to xeroderma pigmentosum (BCC, SCC, MM), Gorlin syndrome (BCC), or the most common mutations demonstrated in approximately 30 % of familial melanoma (CDKN2A gene mutation) [13]. Other predispositions are not yet clearly identified but likely involve genetic polymorphism predisposing as having a large number of nevi (MM). Skin phototype is also genetically determined.
Some viruses can cause skin cancers: HHV8 and KS especially when there is HIV coinfection, oncogenic HPV types and anogenital cancers (increased risk in case of HIV coinfection), HTLV-1 and adult T-cell leukemia/lymphoma (ATLL), Epstein-Barr virus (EBV) and Epstein-Barr virus-associated B-cell lymphomas, and Merkel cell polyomavirus and Merkel cell carcinoma (MCC). The pathophysiology of viral oncogenesis is described in the relevant chapters of this book. All, except perhaps MCC, are frequently described in the tropics.
Immunosuppression induced by immunosuppressive therapy in organ transplant recipients or caused by prolonged CD4+ lymphopenia in patients HIV+ promotes oncogenesis and skin cancers. In organ transplant recipients, UV-induced skin cancers are increased, especially SCC. In the tropics the risk could be higher because the UV radiation is more intense.
Some medications induce SCC: B-RAF inhibitors (vemurafenib) and voriconazole. These expensive drugs are currently not readily available in the tropics.
Various situations can promote the occurrence of skin cancer: chronic inflammatory conditions (chronic infectious dermatoses, ulcers or old burn scars) and predisposing or precancerous dermatologic lesions (actinic keratosis, lichen sclerosus, discoid lupus). Because mutagenic natural substances exist, plants applied on ulcers in the context of traditional medicine could be at risk, but data are lacking. Carcinogenesis is then of the SCC type.
4 Major Types of Skin Cancer in the Tropics
Connectivity – Internet or mobile phones – being rapidly expanding into many of low- and middle-income countries, a quick access to information and to guidelines could become easier, with updated classifications and updated therapeutic indications for skin cancers. For example, this information is freely available in English or Spanish languages on the website “http://www.cancer.gov” or in French language on the website “http://www.sfdermato.com.” The challenges are rather to establish correct diagnosis and to access to treatment options. Here we briefly describe main skin cancers. Table 2 provides guidance on the available treatment options in cases of limited healthcare resources.
Table 2




First-line treatment for invasive skin carcinomas, invasive skin melanoma, and Kaposi sarcoma in the context of limited healthcare resources when standard treatment is not available
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree