Cancer Immunology
CANCER IMMUNOBIOLOGY
Gabriela Soriano Hobbs
Alexander M. Lesokhin
Cancer Immunology Basics
The immune system plays an important role in CA surveillance; Rx that modulate & amplify the immune system are referred to as immunotherapies
Innate immunity: 1st line of defense, include Mφ, DC & NK cells, express pattern recognition receptors (eg, toll-like receptors) that recognize conserved molecular patterns on microbes; recognition via these receptors leads to cytokine production, recruitment & activation of additional immune cells, resulting in killing of pathogens; microbial & cellular fragments are then produced & taken up by Ag-presenting cells (Mφ, B-cells, & DC), ultimately activating the adaptive immune system
T Cells
Cell
Activated by
Effect
Cytokines Produced
CD4+ (eg helper T cell)
Regulate either Th1, Th2, Th17, Treg
Th1-IFN-γ, IL-2
Th2-IL-4, IL-5, IL-10
Th17—IL-17, IL23
CD8+ (CTL)
MHC class I (HLA-A, B, C) on all cell types
Once active can directly kill cells
IFN-γ, IL-2, granzyme, perforin
CD4+ cells: Regulate the immune response, activate Th1, Th2, Th17, or Treg responses depending on cytokine milieu when they see Ag on class II MHC; can also activate Mφ & NK cells, w/c mediate effector functions of T cell subsets → IL-2 regulates their proliferation & activation role in tumor immunology; both preclinical models & pts w/↓CD4 function (ie, HIV pts) show ↑ rates of malignancies
Cytokines—activated by IFN-γ, inhibited by IL-10 & IL-4
Th2 response: (Humoral immune response) leads to B-cell activation, Ab class switching & Ab production, & activation of eosinophils
Cytokines—activated by IL4 & IL-10. Inhibited by INF-γ.
Th17 cells—activated by IL-1, TGF-β, & IL-6, produce IL-17; found in a variety of malignancies & a/w both pro- & antitumor effects (Am J Pathol 2013;182(1):1-10)
Treg—maintain self-tolerance by suppressing expansion of cells directed against self-Ag; Tregs may also play a role in inhibiting tumor-reactive cells (JCO 2006;24:5373-5380); Tregs are activated in the same milieu as effector cells & specific subsets develop to suppress specific arms of immunity based on environmental cues (Science 2009;326(5955):986-991)
Type 1 Tregs are activated by IL-10 then produce further IL-10 & TGF-β (Clin Cancer Res 2008;14(12):3706-3715)
Natural Killer (NK) Cells
Part of innate immune response. NK cells express inhibitory & activating KIRs that mediate NK function & play an important role in preventing relapse after allogeneic transplantation in AML (NEJM 2012;367:805-816); NK cells express Fc receptors & play a role in mediating ADCC
Cytokines: Produce INF-γ, activated by IL-2
Dendritic Cells (DC)
Stimulated by microbes via pattern recognition receptors, cytokines and/or T-cell signals → they then differentiate & migrate to different tissues & become active APCs
Two main types (though others exist)
CD11c positive-myeloid DC: Respond to GM-CSF, & are the most efficient APCs, esp for activation of naïve T cells & play a role in activating tumor-specific CTLs via IL-12
CD11c negative-plasmacytoid DC: Express IL-3 receptor, circulate in the peripheral blood & help mediate innate immune responses, particularly against viruses
Macrophages
Derived from monocytes, specialized phagocytes, function as APCs, recognize cell surface receptors for C′, & Fc receptors for immunoglobin, thus can mediate Ab-dependent cellular uptake
Two main activation states, M1 & M2
Immune Surveillance and Immunoediting
Immunodeficiency is a/w malignancy, as seen in organ transplant recipients, HIV pts, pts w/rheumatic diseases & pts treated w/immunosuppressants; this supports the role of the immune system in CA prev
The three E’s of CA immunoediting: Explanation for the immune system’s role in CA elimination & growth (Review: Nat Immunol 2002;3(11):991-998)
Elimination—the innate immune system (NK & Mφ) is activated by inflammatory cytokines (produced by tumors); innate system activation leads to ↑ secretion of inflammatory cytokines (IL-2 & INF-γ), activating DCs & Mφ resulting in Ag presentation, T-cell activation (both CD4+ & CD8+) & production of CTLs leading to cell death & eradication of developing tumors
Equilibrium—elimination of tumor cells leads to selection of less immunogenic cells; this period of selection & elimination can lead to transient control of tumor growth
Escape—tumors escape the immune system via loss of molecules on tumor cells important for immune activation; tumors can secrete immunosuppressing cytokines (IL-10 & TGF-β) & downregulate INF-γ; in addition, tumors often express non-mutated self-Ag, w/c the immune system will, by definition, not react against; tumors can express molecules that inhibit T-cell function, eg, PD-L1/B7-H1, w/c binds an inhibitory receptor on T cells (PD1) & leads to their inhibition (Immunology 2007;450(7171):903-907)
Tumor microenvironment—immune cells are found in tumors, the exact composition of these cells has been a/w pt outcomes; eg, high concentration of tumor-infiltrating lymphocytes (CD8+ cells) are a/w better outcomes & ↑ response to chemotherapy, Tregs & myeloid-derived suppressor cells are a/w worse outcomes, the exact role of Th17 in tumors is still being elucidated; the milieu of cytokines & chemokines also plays a role in outcome; some cytokines (VEGF, IL-1, IL-8) lead to endothelial cell proliferation, migration, & activation; tumor associated Mφ help promote tumor cell invasion & mets (Nat Rev Cancer 2012;12(4):298-306, Immunology 2011;121(1):1-14)
IMMUNOREGULATORY ANTIBODY THERAPY
Dmitriy Zamarin
Jedd D. Wolchok
Background
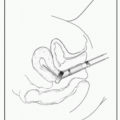
Activation of T cells
Requires two signals: Signal 1: TCR-MHC, Signal 2: CD28-B7-1/B7-2. Interaction of additional receptors & ligands provides either inhibitory (checkpoint) or stimulatory signals regulating T cells activation (Figure 6-1).
Role in CA
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree