Cancer Genetics
BRCA1/2
Payal D. Shah
Kenneth Offit
Mark Robson
Biology
Epidemiology
Clinical Presentation
Pathology
BRCA1-associated breast CA: More likely hormone receptor- & Her2-negative (basal-like subtype, 80%), higher grade; ˜15% medullary carcinomas
BRCA2-associated breast CA: More varied pathology, spectrum more similar to sporadic CA; more hormone receptor-positive (luminal subtype), lobular carcinomas (Cancer Epidem Biomar 2012;21:134)
A/w ovarian serous carcinoma
Risk Assessment
Consider genetic risk evaluation: 2+ breast primaries in 1 individual or in 2 individuals from same side of family; >1 ovarian 1° from the same side of family; self, 1st or 2nd-degree relative w/BC ≤age 45; triple negative <age 60; family member w/known BRCA Mt; male BC, BC + BRCA-related malignancies on same side of family; modify criteria for higher risk populations (eg, AJ) (NEJM 2007;357:154)
Risk assessment models:
Empirical models: Estimate probability that testing will detect a BRCA1/2 Mt (NCI, Myriad, University of Pennsylvania models)
Genetic counseling: Important before genetic testing to ensure that Pt warrants testing, understands benefits as well as risks & potential unanticipated findings from testing; important following testing to guide interpretation, reproductive options
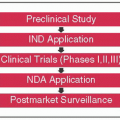
Genetic Testing
Most commercial testing occurs through Myriad Genetics
Components: Comprehensive clinical testing includes full sequencing of BRCA1/2 & testing for specific large genomic rearrangements
NCCN recommendation is to test all at risk for large genomic rearrangements (LGRs) if negative sequencing
| ||||||||||
Screening
Self-breast exam: NCCN recommends education & training on SBE beginning age 18 to promote breast self-awareness
Breast CA screening: CBE q6-12mo beginning age 25, annual mammogram + annual breast MRI beginning age 25 or younger based on earliest onset in affected family member; consider U/S as adjunct to mammography for women w/dense breasts, w/c limits Se of mammography, though questionable utility if performing MRI
Ovarian CA screening: No definitive evidence supporting screening, but can consider transvaginal U/S + CA-125 q6mo beginning age 30 or earlier depending on earliest onset in family
Other malignancies (endometrial, prostate, pancreas): Age-appropriate malignancy screening, to be initiated early depending on FHx
Male carriers: Breast self-exam training & education beginning age 35; CBE q6-12mos beginning age 35; consider mammogram age 40, prostate evaluation starting at 40
Recommendations for relatives: Encourage genetic counseling & possible genetic testing
Risk Reduction
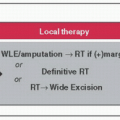
Risk-reducing mastectomy: ↓ breast CA risk by ≥90%; recommend discussing w/all known BRCA Mt carriers
Risk-reducing salpingo-oophorectomy: ↓ ovarian CA risk by 85-90% & breast CA risk by approximately 50% if performed premenopausally; a/w lower all-cause, breast CA-specific, & ovarian CA-specific mortality (JAMA 2010;304:967); guidelines recommend RRBSO after completion of child-bearing, ideally between ages 35-40
Chemoprevention: If risk-reducing medical intervention is desired, can consider tamoxifen, though limited evidence
Treatment
Surgery: Same as for non-Mt carriers, though may more strongly consider bilateral (risk-reducing) mastectomy during surgical tx
Chemotherapy: Agents, indications & dosing same as for nonMt carriers; evidence suggests anthracycline/taxane combination w/benefit in BRCA1 Mt carriers as in sporadic triple-negative carriers; BRCA-associated breast CA may be particularly sensitive to platinum compounds (investigational question)
PARP inhibitors: Promote synthetic lethality in BRCA-associated breast CA (deficient in homologous repair) (Lancet 2010;376:235); studies pending
Endocrine Rx: Agents, indications & dosing same as for nonMt carriers
Her2-targeted Rx: Agents, indications & dosing same as for nonMt carriers
LYNCH SYNDROME & FAP
Payal D. Shah
Zsofia K. Stadler
LYNCH SYNDROME (LS, FORMERLY HNPCC)
Biology
Caused by germline Mt in DNA MMR gene (MLH1, MSH2, MSH6 >> PMS2) or 3′ del in EPCAM/TACSTD1 gene (leads to MSH2 silencing)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree