Reduction mammaplasty for women with breast cancer has become a reliable option and adjunct following partial or total mastectomy.1–3 In the setting of partial mastectomy, reduction mammaplasty can be performed on the ipsilateral and contralateral breast and is commonly referred to as oncoplastic breast surgery. In the setting of unilateral total mastectomy followed by autologous or prosthetic reconstruction, reduction mammaplasty can be performed on the contralateral breast for symmetry. In the setting of breast conservation, reduction mammaplasty following radiation therapy can be performed safely and effectively albeit with some technical modification.
Reduction mammaplasty in the setting of breast cancer has been demonstrated to enhance patient satisfaction and to improve reconstructive outcomes by achieving symmetry, contour, and desired shape.4 This chapter reviews the indications and salient aspects of reduction mammaplasty in the setting of breast conservation, oncoplastic surgery as well as ipsilateral total mastectomy with contralateral mammary hypertrophy.
In patients that are candidates for partial mastectomy, oncoplastic reconstruction is commonly used to preserve breast shape and contour. For some women, a volume displacement procedure will suffice and for other women, a volume replacement procedure will be necessary.3,5 Volume displacement procedures include adjacent tissue rearrangement, mastopexy, and reduction mammaplasty. Reduction mammaplasty is generally considered in women with large or excessively ptotic breasts. The author’s indications for a reduction mammaplasty following partial mastectomy include women with mild, moderate, and severe hypertrophy who are typically defined as requiring excision of 300 to 600 g, 600 to 1200 g, and greater than 1200 g of tissue, respectively.
Following partial mastectomy, a reduction mammaplasty can be performed on the ipsilateral as well as contralateral breast. Oncoplastic reduction mammaplasty can be performed immediately or as a staged-immediate procedure that typically occurs 1 to 2 weeks following the ablative procedure that coincides with the discovery of the final pathology. The goal of immediate and staged-immediate reduction mammaplasty is to optimally contour the breast prior to the initiation of radiation therapy in order to minimize the incidence of contour abnormalities.
Another group of patients that may benefit from reduction mammaplasty are those that have had breast conservation in the setting of mammary hypertrophy.6 Performing a reduction mammaplasty in a previously radiated breast poses additional challenges because the radiated tissues have compromised vascularity, increased fibrosis, and are more prone to adverse events such as fat necrosis and delayed healing. Technical modifications are necessary to ensure predictable outcomes.
In patients who have had unilateral total mastectomy with reconstruction, the desire to achieve symmetry with the opposite breast is common.7–9 In situations where the opposite breast is hypertrophic, a reduction mammaplasty is usually indicated. In a review of the various symmetry procedures following unilateral mastectomy and reconstruction, the performance of a contralateral reduction mammaplasty was the most common.7,9 Reduction mammaplasty can be performed using a variety of techniques depending on the characteristics of the breast. There are various incisional patterns and parenchymal resection techniques that this author considers based on the amount of tissue to be resected and the length that the nipple-areolar complex (NAC) is elevated. In general, breast parenchymal resection volumes less than 300 g are typically reduced with vertical incisional patterns. When resection volume is 300 to 600 g, an inverted T incisional pattern with a superomedial or central mound pedicle technique is commonly utilized. When the resection volume exceeds 600 g, an inverted T incisional pattern with a medial, lateral, or inferior pedicle technique is considered. These represent the author’s preferred techniques.
Knowledge of the normal anatomy of the breast is essential when considering a reduction mammaplasty. Breast tissue is composed of lobules and ducts arranged in a segmental fashion. A thin and inconspicuous layer known as the investing fascia of the breast encapsulates the parenchyma. Between the investing fascia and the skin is the subcutaneous fat. This subcutaneous layer varies in thickness from a few millimeters to 2 or 3 cm. The breast is innervated via the second to sixth intercostal nerves. The NAC is typically innervated via the fourth intercostal nerve. The vascularity to the breast is derived from multiple sources and includes branches from the internal mammary, lateral thoracic, intercostal, and pectoral vessels. Most studies have suggested that the internal mammary perforators are the dominant blood supplier to the breast, although the lateral thoracic and intercostal perforators also have a significant contribution.
The indications for a reduction mammaplasty in the setting of breast cancer apply to patients who have had unilateral mastectomy and total reconstruction and need contralateral reduction, to patients who have mammary hypertrophy and are considering partial mastectomy, and to patients who have mammary hypertrophy and have had prior breast-conservation therapy. In the case of a partial mastectomy, an ipsilateral and contralateral reduction mammaplasty is an excellent option to achieve natural breast shape, contour, and symmetry. This is performed before the radiation therapy in order to avoid the contour abnormalities that are typically observed following radiation. Without glandular rearrangement to fill the partial breast defect, the likelihood of a contour abnormality is high and exacerbated following radiation therapy. This is sometimes observed in patients following breast conservation.
With oncoplastic surgery, the contralateral breast is usually reduced concurrently with the ipsilateral breast. When considering oncoplastic surgery and bilateral reduction mammaplasty, there are several factors that should be appreciated prior to proceeding. A thorough evaluation of the breast should be performed to confirm the absence of malignancy that includes physical examination and breast imaging. Patient expectations must also be appreciated with regard to size and shape of the postoperative breast.10
The contraindications for a reduction mammaplasty are based on breast size, breast abnormalities, and comorbidities. In women who lack sufficient breast volume, a reduction mammaplasty may not be the best option. In these patients, a mastopexy or adjacent tissue rearrangement may be more appropriate. The biplanar technique can be considered as an alternative in women who are not candidates for reduction mammaplasty and includes placement of a small prosthetic device as well as mastopexy.11 The ablative portion of the operation is usually performed through a circumvertical incision followed by glandular rearrangement and placement of a small tissue expander or implant in the subpectoral space.
The presence of an abnormality on breast imaging may preclude performing a reduction in favor of a more aggressive approach. Contralateral malignancy has been demonstrated to occur in 3% to 4% of women.12,13 These tumors can be synchronous and defined as occurring within 4 months of the initial diagnosis or as metachronous that is defined as occurring later than 4 months following the initial diagnosis.12 Prognostic factors associated with an increased risk for a metachronous breast cancer include younger women (less than 45-year-old) and tumors with lobular histology located in the central or inner quadrants.13,14
The preoperative assessment of patients with breast cancer that are considering reduction mammaplasty requires a thorough history and physical examination, breast imaging, as well as a discussion regarding expectations. The timing of oncoplastic surgery includes immediate and staged-immediate and will be reviewed and explained in the forthcoming sections. In patients who have had breast conservation and radiation in the setting of mammary hypertrophy, performance of a reduction mammaplasty may pose additional challenges and has the potential for morbidity. The various reduction mammaplasty techniques are discussed and decisions are made with regard to the various incisional patterns.
Risk factors for poor outcomes, such as obesity, poorly controlled diabetes mellitus, prior radiation therapy, and tobacco use, should be addressed and appropriately managed. Patients should also be informed that because of the recurrence potential and because subsequent cancers may occur, continued surveillance of both breasts is recommended.
In patients considering immediate bilateral reduction mammaplasty following unilateral oncoplastic surgery, several factors should be noted. The first is that the specific reduction technique may be different for the two breasts and based on the specific location of the resected tumor. This may alter the orientation of the pedicle. The plastic surgeon should have a general idea of how the breast will appear following the procedure. The contralateral breast will serve as a template for the oncoplastic breast. Another important factor is that the cancer breast will be radiated and the contralateral breast will not. This may cause the oncoplastic breast to shrink; therefore, the cancerous breast should be slightly larger than the noncancerous breast. In the setting of immediate or staged-immediate oncoplastic reduction mammaplasty, it is usually recommended to leave the cancerous breast 5% to 10% larger based on volume of resection. In the setting of delayed reduction mammaplasty, it is best to wait at least 1 year following the radiation to perform the contralateral reduction. Both of these strategies can result in improved breast symmetry.
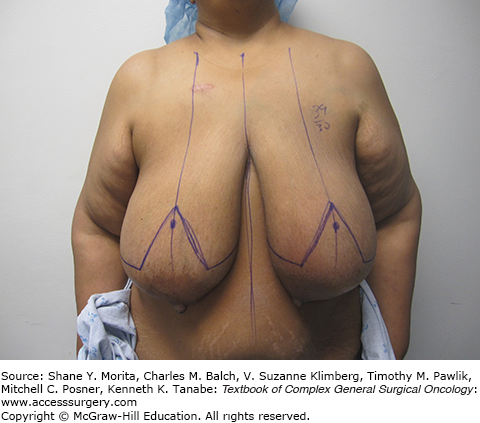
There are several important measurements and landmarks that are considered prior to the reduction mammaplasty that will assist with surgical planning. Basic measurements include the sternal notch to nipple distance, the base width of the breast, the nipple to inframammary fold (IMF) distance, and the nipple to mid sternal distance. These measurements will serve to a guide regarding breast symmetry. There are certain landmarks that also require delineation. These include the sternal midline, the IMF, and the breast meridian. The breast meridian is delineated by marking the mid-clavicle point and then extending this along the midline of the breast (Fig. 153-1). Usually this will bisect the NAC; however, when the NAC is medially or laterally displaced, the meridian will be displaced to the right or left of the NAC. The author’s ideal location for the NAC is at the level of the IMF and is vertically adjusted to lie at the breast meridian. Depending on breast volume and degree of ptosis either an inverted T or a circumvertical pattern is delineated. An inverted T is used for severe mammary hypertrophy and the circumvertical pattern is sometimes used for moderate mammary hypertrophy. The orientation of the pedicle is an important consideration for NAC transposition. This is usually achieved using a pedicle that is oriented 180 degrees away from the defect. For upper pole tumors, an inferior pedicle is considered. For lower pole tumors, a superior, superomedial, or medial pedicle is considered. For medially or laterally based tumors, the pedicle is oriented such that the resulting deformity can be adequately filled.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree