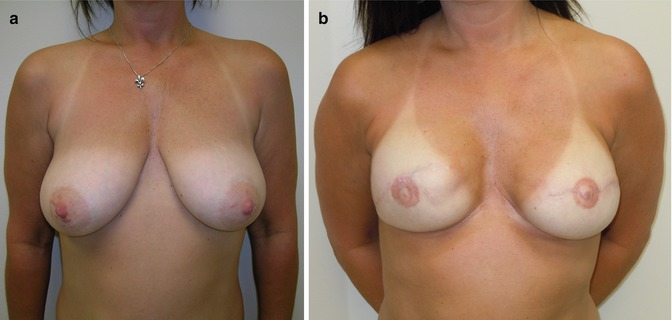
Fig. 18.1
Expander reconstruction with acellular dermal matrix
Postoperative Course
The postoperative course of non-autologous reconstruction patients is straightforward. It consists of an overnight stay in the hospital with drain-care teaching. Drains are removed 1–2 weeks postoperatively when output falls to <30 cc/day. It is extremely important to treat the drains as one would treat a central line, with meticulous site care. Infection arising from the drains is a serious problem and may well cause cellulitis, periprosthetic infection, or loss of the implant.
After healing of incisions (2–3 weeks), tissue expansion may begin. The magnetic port finder is used to locate the valve. The amount to sterile saline injected is surgeon dependent; amounts from 50 to 120 cc can be injected. Patient comfort often dictates the amount of saline injected at one time. Care must be taken to avoid overexpansion at a single setting, which can lead to skin flap necrosis. Expansions can occur weekly and last from 3 to 6 months, until the desired volume is achieved. In the unilateral setting, the contralateral breast size guides the expansion need. Some surgeons advocate overexpansion of up to 110–120 % over the patient’s desired size. This creates a natural ptotic result when a smaller implant is placed in the larger skin envelope.
Second Stage Reconstruction
Once appropriate volume is reached in the tissue expander, the patient returns to the operating room for implant placement. Cohesive silicone gel implants are used for a more natural feel and appearance. Cohesive gel also decreases the appearance of rippling of the reconstructed breast. During the past decade, continuing improvements in implant technology has made a tremendous improvement in outcomes. If the patient has had a shaped expander, a matching implant should be used. Preoperatively, with the patient standing, landmarks of the breast are marked. The capsule is assessed; areas in need of capsulorrhaphy or capsulotomy are appropriately marked. The base diameter is again confirmed. Several sizes of previously chosen implants should be available. The un-inflated tissue expander can add as much as 100 cc to the total volume needed. This needs to be taken into consideration when deciding upon the final volume of the implant, and not just the amount of fill.
A portion of the previous skin incision is opened. If the mastectomy was previously performed through a transverse incision and the breast has good contour and projection, another option is to utilize an inframammary incision along the lateral aspect of the breast rather than reoperating through a central transverse scar. This avoids flattening of the anterior breast with the additional surgery through the old scar. Occasionally, a Z-plasty must be performed to further release the central scar. Dissection is taken through the subcutaneous tissue to the pectoralis muscle. The muscle is split with the electrocautery and capsule is incised. Capsulorrhaphy or capsulotomy is performed as needed. Once hemostasis is achieved, the appropriately sized implant is placed in the pocket. The wound is then closed in multiple layers paying special attention to avoid piercing the newly placed implant. At this stage, patients may elect to undergo a symmetry procedure on contralateral breast. This can include reduction, mastopexy or augmentation, depending upon the patient’s need. This is performed as an outpatient procedure performed without need for drains. A soft bra is worn for several weeks. Nipple reconstruction is usually performed up to 2–3 months following implant placement and will be discussed later in the chapter on revision surgery.
Variations of Implant-Based Reconstructions
Delayed Reconstruction with Implants
When reconstruction is delayed, the challenges of using implants and expanders are much greater compared to immediate reconstruction. This is especially true when there has been a long period of time between the mastectomy and reconstruction. The skin is deficient and usually adherent to the underlying pectoralis. Frequently the inframammary fold is distorted or lost and providing adequate soft tissue becomes a challenge. This insufficient, thin, and scarred skin is very difficult to expand with an expander alone. Patients having delayed reconstruction are most effectively treated with an autologous reconstruction rather than implant based reconstruction. If implant based reconstruction is to be accomplished the deficiency can be remied. The deficiency can be remedied by adding tissue to the mastectomy site, in the form of regional flaps. The latissimus dorsi muscle transfer is the most common transfer (Fig. 18.2). Even with the improved soft tissue envelope, an expander may have to be used to provide space for an eventual prosthesis.
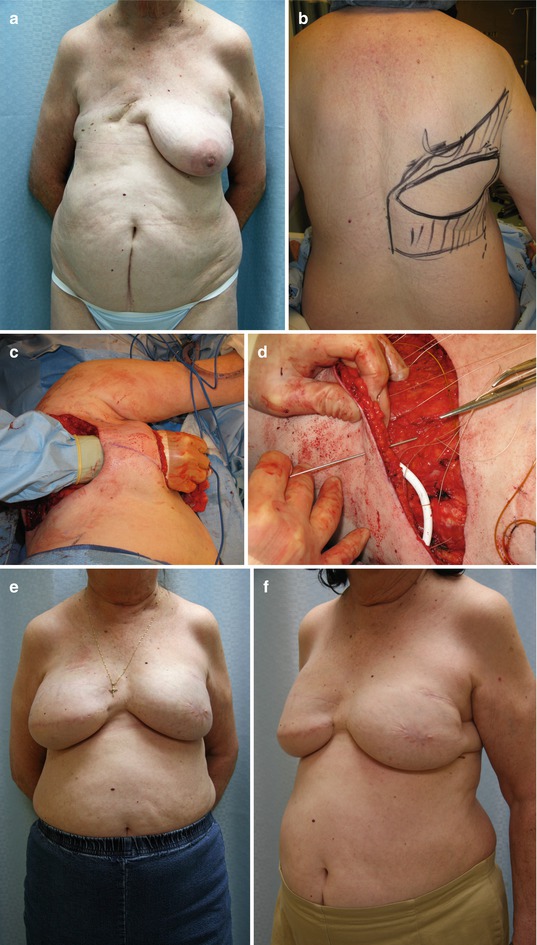
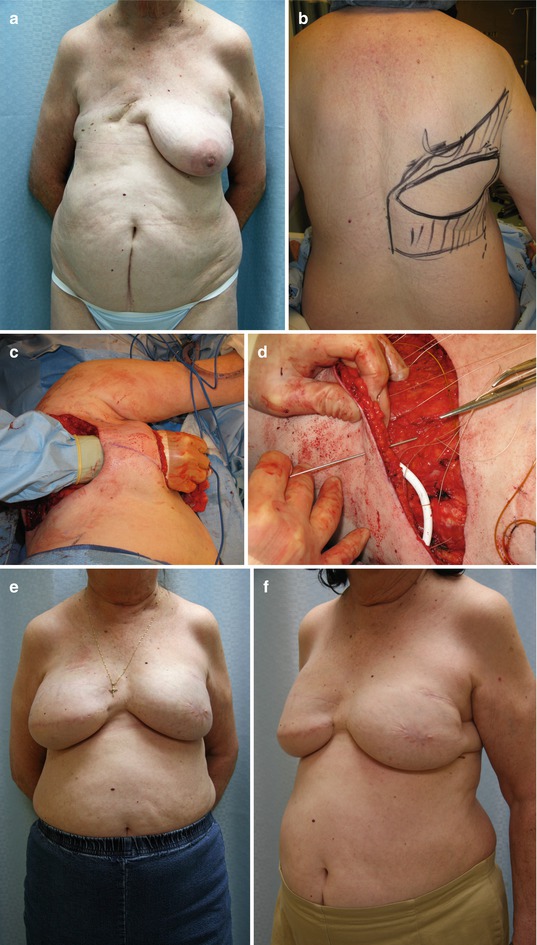
Fig. 18.2
Delayed reconstruction with latissimus dorsi myocutaneous flap and expander. (a) Preoperative view showing shortage of soft tissue. (b) Preoperative markings for latissimus myocutaneous flap. (c) Intraoperative view of tunnel through which the flap is passed. (d) Sewing the acellular dermal matrix to the lateral chest wall to shape pocket for expander. (e, f) Three postoperative result (Patient had opposite side mastectomy and implant reconstruction)
Direct-to-Implant Breast Reconstruction
The use of ADM has renewed interest in an old method of implant-based reconstruction. In the past, when implants were placed beneath thin mastectomy flaps without adequate soft tissue coverage, complications were common and the aesthetic results were suboptimal. With the scaffolding created by utilizing ADM, immediate implant-based reconstruction is now a feasible option.
This reconstruction may be done as a single-stage procedure. The ideal candidate for the single-stage direct-to-implant technique is a patient with a medium or small breast size, grade 0–1 ptosis, and good skin quality. A nipple-sparing mastectomy and the absence of skin resection make this procedure possible. The ideal incision in patients with small, well-shaped breasts is the inframammary incision. The ADM is placed the same as was previously discussed in the tissue expander section. Instead of an expander, the final implant is placed. The wounds are closed over two drains and kept in place for 7–14 days [5].
Patients who have resection of the nipple-aureola complex and skin, but who have mastectomy flaps which are adequate, in both size and vitality, may also be reconstructed with a direct-to-implant technique. They will require a secondary procedure to reconstruct the nipple.
The Effect of Radiation on Breast Reconstruction
Current recommendations for postmastectomy radiation are in T3 or T4 tumors, tumors involving the skin, and tumors with three or more positive lymph nodes or one lymph node with extracapsular invasion. There is much debate about the timing of reconstruction with respect to the initiation of radiation. In the delayed setting, implant-based reconstruction is often difficult. Radiated skin is fibrosed and fixated to the chest wall, making tissue expansion difficult and compromising the aesthetic quality of the reconstructed breast (Fig. 18.3). In this group of patients, problems with wound healing may occur, as well as higher rates of capsular contracture [6, 7]. Patients who have had postmastectomy radiation and still desire implant reconstruction may benefit from the use of a latissimus dorsi (LD) flap. The patient will have a large skin deficit, which will be hard to expand. The benefits of this flap are multiple. The fibrosed postradiation skin may be removed and replaced by the healthy skin paddle that the LD flap provides. Additionally, the bulky latissimus muscle provides for an optimal adjunct for implant coverage. It is the author’s practice to offer the patient with a previously radiated chest the option of autologous reconstruction, which provides optimal skin coverage and produces a more aesthetically acceptable breast in this type of patient. The author also feels strongly that chest wall radiation following flap reconstruction can cause fibrosis and loss of volume in the flap. We make every effort to avoid immediate reconstruction in patients who will have radiation therapy planned, whether with autologous or non-autologous procedures.


Fig. 18.3
Severe capsule contracture in implant reconstruction following radiation therapy
The choice is made to proceed with implant/expander reconstruction despite the inherent problems of wound healing and high rates of capsule contracture, and some protocol must be found to reduce complications. The key to successful implant-based reconstruction in the immediate reconstruction patient who faces radiation therapy is to maintain the natural breast skin envelope during radiation. Two published series have addressed these issues.
MD Anderson employs the “delayed immediate” reconstruction tactic for use in this setting. The patient undergoes placement of a completely filled tissue expander at the time of the mastectomy. Once the pathology is finalized and it is confirmed that the patient will not require radiation, immediate reconstruction may then be performed. If radiation will be needed, the tissue expander is deflated. Once radiation is complete, tissue expansion may commence, followed by definitive reconstruction [8, 9].
Memorial Sloan Kettering uses a different protocol. The treatment algorithm begins as a modified radical mastectomy with immediate placement of tissue expanders that are not fully expanded. At approximately 5 weeks postoperatively, chemotherapy is initiated with concurrent expander inflation. Four weeks following the completion of chemotherapy, patients undergo exchange of the tissue expanders for permanent implants. Postmastectomy radiation is usually initiated about 1 month following implant placement [10]. Their reported incidence of postradiation complications is more favorable than that reported by the MD Anderson series. Additionally, radiation delivery is more easily achieved with implants rather than expanders.
Kronowitz states “despite advances in reconstructive devices and materials, post-mastectomy radiation therapy still appears to have an adverse impact on outcomes of implant-based breast reconstruction.” In a review of the literature, he notes that most postmastectomy radiation therapy tissue expander reconstructions had a significant amount of unplanned or major corrective surgery. Approximately one-third of patients develop Baker grade III or IV capsular contracture, characterized by pain and distortion. Despite the complications and additional surgery, the majority of patients who undergo implant-based reconstruction and postmastectomy radiation therapy ultimately keep the implant-based reconstruction (Figs. 18.4 and 18.5) [11]. There is some evidence that acellular dermal matrix may have protective effects to avoid complications, this topic is being researched extensively.