Breast Reconstruction
Babak J. Mehrara
Alice Y. Ho
Breast reconstruction is an important component of breast cancer management and improves quality of life and psychosocial well-being (1). Improvements in techniques have resulted in more natural reconstructions, decreased morbidity, and improved outcomes. Breast reconstruction has traditionally been considered reconstruction after mastectomy, however, more recent studies have reported improved outcomes even after segmental resection in some circumstances. Therefore, plastic surgeons are important members of a multidisciplinary breast team and by working closely with breast surgeons, medical oncologists, and radiation oncologists, they can help individualize and optimize breast cancer care.
In general, most women who undergo breast surgery for cancer treatment are candidates for reconstruction and there are no absolute contraindications. However, most reconstructive surgeons consider inflammatory breast cancer requiring massive skin resection and significant medical comorbidities that increase risk of medical complications as relative contraindications. In addition, reconstruction in women who will require postmastectomy radiation therapy is hotly debated and the ideal approach remains unknown. However, even in these circumstances reconstruction is warranted in some cases and must be considered on an individual bases. For example, a patient with inflammatory breast cancer who requires extensive skin resection may need reconstruction as a component of her care simply to close the resulting mastectomy skin defect.
The type of reconstruction that is performed is dependent on a number of factors including oncologic considerations, patient desires and expectations, body habitus, and surgical risk factors. Patients should be evaluated by a qualified plastic surgeon who can evaluate these considerations and advise the patients on their best reconstructive option and the ideal time to initiate the process based on their individual circumstances.
IMMEDIATE VERSUS DELAYED RECONSTRUCTION
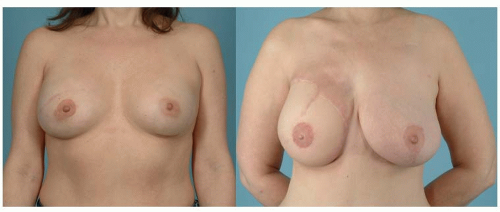
Reconstruction can be performed either at the time of mastectomy or segmental breast resection or in a delayed manner after adjuvant treatment is completed. The timing of reconstruction is dependent on oncologic considerations and patient factors. In general, the vast majority of patients are candidates for immediate reconstruction and this approach has a number of advantages. For example, reconstruction at the time of mastectomy is associated with improved aesthetic outcomes by preserving the breast shape and envelope (Fig. 36-1). Immediate reconstruction is also easier to perform technically since there is usually less scarring and contracture. Immediate reconstruction does not delay or hinder diagnosis of a recurrence and, in most cases, does not alter its treatment (2). In addition, immediate reconstruction has important psychological benefits resulting in decreased anxiety and improved selfimage, and enabling patients to cope with their diagnosis and treatment (3). From a practical standpoint, immediate reconstruction saves the patient an additional trip to the operating room.
There are, however, some potential disadvantages to immediate reconstruction. One consideration is an increased risk of complications associated with combining oncological treatment and reconstruction. Although this idea makes intuitive sense, very few studies have actually compared complication rates in the same patient cohorts. In addition, the majority of complications that occur in the setting of immediate reconstruction are minor in nature and rarely delay adjuvant therapy (4, 5). Mastectomy skin flap necrosis is much more common after immediate reconstruction and likely reflects the more extensive dissection that is performed at the time of mastectomy. Some patients are
also overwhelmed with the number of decisions they need to make for immediate reconstruction, leading to increased anxiety in some cases.
also overwhelmed with the number of decisions they need to make for immediate reconstruction, leading to increased anxiety in some cases.
IMPLANT VERSUS AUTOGENOUS RECONSTRUCTION
Breast reconstruction can be categorized broadly into implant based or autologous tissue (i.e., the patient’s own tissue) reconstruction (Table 36-1). Implant reconstructions make up the bulk of breast reconstructions that are performed annually in the United States. Implant reconstruction is simpler to perform, is associated with low rates of complications, and does not significantly increase hospital stay or recovery as compared with mastectomy alone. Although most patients are candidates for implant reconstruction, there are some relative contraindications including severe medical comorbidities, oncologic factors necessitating massive skin excision, severe immune deficiency, heavy smoking history, massive obesity, and history of breast irradiation. These circumstances increase the rates of complications associated with implant reconstruction, but do not preclude their use in select cases.
TABLE 36-1 Advantages and Disadvantages of Implant-Based or Autogenous Tissue-Based Breast Reconstruction | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
A disadvantage of implant reconstructions is that implants require maintenance and need to be replaced if they rupture or leak. Although implant technology has improved considerably over the past two decades, most modern implants have an average life span of approximately 10 years. A recent study demonstrated a 4-year leak rate of 4% to 15% in saline implants depending on the manufacturer used (6). In addition, because implants are a foreign substance and are placed underneath the pectoralis muscle, these reconstructions do not feel as natural as a normal breast. It is also difficult to obtain perfect or near perfect symmetry with implants in unilateral reconstructions even when contralateral symmetry procedures such as augmentation, reduction, or mastopexy are performed. Asymmetry of implant reconstructions with the normal breast tends to worsen over time, particularly if patients gain or lose weight, since the implant size does not change and the implant pocket does not sag. Thus, although aesthetic results have improved over the years, the primary goal of implant reconstructions is to have reasonable symmetry in clothes, a bra, or a bathing suit. By far the biggest disadvantage of implant reconstructions is the potential for developing capsular contracture. A capsule is a fibrous covering that develops around any prosthetic device that is placed subcutaneously. Capsular contracture develops when the capsule surrounding the implant becomes thickened and tight, causing patients to complain about tightness, pain, or implant malposition. The degree of contracture can be quantified using the Baker scale and uses a four-point scale based on physical exam and symptoms. Grade I is a normalappearing, soft breast; grade II refers to breast implants that are firm but appear normal; grade III includes implants that are firm and appear abnormal; grade IV capsular contracture is the most severe and includes breasts that are hard, painful, and appear abnormal often with severe distortion. Most women who undergo implant reconstruction have grade I or II capsular contracture (89.6%) (7).
Breast reconstruction can also be performed using a patient’s own tissues (autologous reconstruction). In these procedures, a combination of skin, fat, and muscle is transferred to the breast to reconstruct either the entire breast or a portion thereof. Tissues can be transferred from adjacent areas such as the back (latissimus flap) or abdomen or from sites located distant to the breast including the gluteal region or the inner thigh. Reconstruction can be performed either purely with autologous tissues or in combination with an implant. Autologous tissues are transferred to the breast site either by keeping their local blood supply intact (pedicled flaps) or by disconnecting and reconnecting the arterial and venous circulation using microsurgical techniques (microsurgical or free flaps). Similar to implants, autologous tissue reconstruction has high success rates and patient satisfaction.
Autologous tissue reconstruction is indicated in women who wish to avoid using implants, have failed implant reconstruction previously, or who are poor implant reconstruction candidates. For example, a patient who has undergone mastectomy and radiation is unlikely to have a successful reconstruction using an implant alone since the remaining mastectomy skin has been injured. In these circumstances, a portion of the damaged mastectomy skin is usually replaced by healthy tissues from a distant flap donor site and reconstruction is completed. Another example is a patient who has very large, ptotic breasts that are unlikely to be adequately matched with an implant reconstruction.
The main advantage of autologous tissues is the fact that reconstruction is performed with living tissues. These tissues age with the patient, changing over time to maintain symmetry with the contralateral breast. In contrast to implants, autologous tissues are tailored to the patient and more likely to have symmetry immediately after reconstruction. Tissue reconstructions feel and look more natural because, unlike implants, the tissues are placed in the subcutaneous plane simply replacing the breast rather than in a subpectoral position. Tissue reconstructions also do not develop fibrous capsules and can help replace damaged tissues to break up scar and relieve contracture. As a result of these advantages, tissue-based reconstructions are considered the gold standard for aesthetic reconstruction.
Of course, all good things come at a cost. The “cost” in the case of autologous tissues is donor site morbidity that increases recovery time and can have long-term consequences. At the minimum, patients reconstructed with their own tissues will have donor site scarring that in some cases may be unaesthetic. Chronic donor site pain and bothersome loss of sensation have also been reported for patients reconstructed with various types of autogenous tissues. Functional issues such as abdominal wall weakness, bulging, or hernia complicate abdominal tissue-based reconstructions in some patients. Similarly, patients reconstructed with latissimus flaps may have decreased upper extremity strength and range of motion that in some cases may necessitate physical therapy.
IMPLANT-BASED RECONSTRUCTION
In general, most patients are candidates for implant reconstruction including elderly patients and those with medical comorbidities that may preclude more complex forms of reconstruction. Absolute contraindications to implant reconstruction include severe tissue deficiency from resection or secondary to tissue damage from radiation. Relative contraindications for implant reconstruction are severe lifethreatening medical comorbidities, massive obesity, and possibly long-standing heavy cigarette smoking. Some surgeons also consider the need for postmastectomy radiation therapy as a relative contraindication; however, this concept has been debated and there is no uniform consensus.
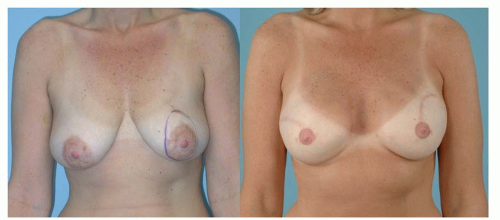 FIGURE 36-2 Pre- (left) and postoperative (right) photographs of a patient 1.5 years following reconstruction with bilateral silicone implants. |
The ideal patient for implant reconstruction is thin, has moderate-sized breasts (B to C cup), minimal ptosis, and well-defined breast shape (Fig. 36-2). Although most women who undergo implant reconstruction do not have these characteristics, reasonable reconstructions with good symmetry in clothes, bra, or bathing suits is possible, particularly if contralateral breast symmetry procedures are performed. These issues are less critical in bilateral reconstructions since a similar implant is used for the contralateral breast, resulting in even better symmetry, and likely contributes to the higher rates of satisfaction in this cohort (8).
It is difficult to achieve symmetry with implant-based reconstructions in women with either very small or very large breasts. Reconstruction of very small breasts is complicated by the fact that low-volume implants needed in these cases typically have a small base diameter (the width of the implant). This issue makes it difficult to simultaneously match the volume and diameter of the breast, resulting in a wide space between the breasts. An alternative approach for improved symmetry in these cases may be contralateral augmentation to increase the volume of the normal breast.
Reconstruction of massive breasts or very obese patients with implants is also difficult due to the fact that the largest implant currently available in the United States is 800 to 850 cc. Although this is a large size, and suitable for most large-breasted women, in some women with massive breasts or those who are morbidly obese, these large implants are simply inadequate volume to achieve sufficient projection for an aesthetic outcome or to match the contralateral breast. Even if a large reduction is performed in the contralateral breast, these procedures may be inadequate to sufficiently decrease the volume, projection, or base diameter of the remaining breast, resulting in a reconstructed breast that is too small, flat, or narrow, respectively, to fit the patient’s chest wall. In these cases, patients may require a small external prosthesis for improved symmetry or may be advised to undergo reconstruction with alternative measures.
Implant reconstruction can be performed either immediately after mastectomy or in a delayed fashion. The ideal incision for implant reconstruction is debated; however, incisions placed along the lines of relaxed skin tension lines (i.e., Langer’s lines) are selected by most surgeons since these incisions enable maximal skin expansion. Skin-sparing
mastectomies in appropriate candidates preserve the breast envelope and enable more rapid expansion. Skin preservation is important even in non-skin-sparing procedures since there is a limit to the amount of expansion that can be performed. Overexpanded skin may become thin, shiny, and lose elasticity, resulting in impaired aesthetics, discomfort, and implant exposure. Although the oncologic risks of nipple-sparing mastectomy is still undefined and remains a source of debate, there is little doubt that these techniques have excellent cosmetic outcomes in appropriately selected patients.
mastectomies in appropriate candidates preserve the breast envelope and enable more rapid expansion. Skin preservation is important even in non-skin-sparing procedures since there is a limit to the amount of expansion that can be performed. Overexpanded skin may become thin, shiny, and lose elasticity, resulting in impaired aesthetics, discomfort, and implant exposure. Although the oncologic risks of nipple-sparing mastectomy is still undefined and remains a source of debate, there is little doubt that these techniques have excellent cosmetic outcomes in appropriately selected patients.
The majority of implant reconstructions are performed as a two-step procedure with placement of a tissue expander initially and then conversion to a permanent implant at a later time. Tissue expander sizing is based on the dimensions of the breast pocket (width and height) and to a lesser degree the volume of the breast. With popularization and wide adoption of skin-sparing and nipple-sparing mastectomies, several groups have reported single-stage direct to implant reconstructions that avoid expander insertion (since the skin does not need to be expanded). In general, these studies have reported good to excellent results with reasonable safety profiles; however, the vast majority of these reports maintain that careful patient selection is important. These studies require validation in large prospective studies as most reports have been on limited numbers of patients and performed in a retrospective manner.
Implants and expanders for breast reconstruction are placed underneath the pectoralis major muscle. Total submuscular coverage of the implant can be obtained by elevating a portion of the rectus abdominis fascia inferiorly and serratus anterior muscle or fascia laterally to completely cover the expander. This technique is thought to decrease implant infections by providing vascularized coverage (7).
Some surgeons have criticized the total submuscular coverage technique with concerns about lower pole expansion, implant projection, and maintenance of the inframammary fold. These concerns have led to a variety of techniques including dis-insertion of the inferior insertion of pectoralis major muscle or the use of acellular dermal matrices. Over the past 10 years or so, the use of acellular dermal matrices such as AlloDerm or FlexHD to provide lower pole coverage of the expander/implant have gained significant popularity. In these procedures, the pectoralis major muscle is elevated and dis-inserted inferiorly. The lower/lateral portion of the implant is then covered with acellular dermis sutured inferiorly to the inframammary fold/lateral chest wall, and superiorly to the elevated pectoralis major muscle. Although some authors have reported excellent cosmetic results with low rates of complications (9), other reports have suggested that the use of acellular dermal matrices is associated with small, though statistically significant increases in the risk of implant infection and reconstructive failure (10). Large, prospective studies will be necessary to resolve this debate.
Once the expander is placed in the subpectoral pocket, the expander is filled intraoperatively with the final volume determined by tension on the skin and muscle. Expander filling in the office starts usually 2 weeks after surgery with 30 to 120 cc of sterile normal saline per expansion until the final volume is reached. If chemotherapy is not needed, then exchange to permanent implant is performed once the mastectomy skin flaps have completely healed. These procedures are usually performed 4 to 12 weeks following completion of chemotherapy in patients who required adjuvant treatments. The second stage of reconstruction is usually performed in an outpatient setting.
The main advantage of saline implants is the fact that if they leak, then the saline solution is simply absorbed and the implant is exchanged. However, saline implants tend to have more visible rippling and are not as comfortable as silicone implants. This latter contention is supported by recent studies utilizing validated quality of life questionnaires showing that patients with silicone implants have higher quality of life and increased satisfaction as compared with saline implants (11).
The main disadvantage of silicone implants is that leaking silicone is not absorbed and requires surgical removal. The leaking silicone is usually contained in the breast implant pocket; however, silicone extravasation can cause inflammation and capsular contracture and may be taken up by regional lymph nodes. Anecdotal reports in the late 1980s linked leaking silicone implants with a variety of ailments including autoimmune disorders and increased risk of malignancies, leading to the withdrawal of these implants by the Food and Drug Administration (FDA) in 1992 (except for procedures performed as a part of an FDA-approved research protocol). However, large-scale studies performed both in the United States and in Europe failed to find a statistically significant relationship in these outcomes and the implants are now approved by the FDA both for reconstructive and cosmetic procedures. Recent reports have suggested that textured implants in general (both saline and silicone) may be associated with a rare form of lymphoma, with an estimated incidence of 1 in 1 million; however, these reports need further study and validation (12).
Advancements in implant technology have introduced newer silicone implants filled with a silicone gel that is semisolid and therefore thought to be less likely to leak. These implants, referred to as form-stable, cohesive, or “gummy bear” implants, have some advantages including better shape in some patients and possibly a lower risk of leakage; however, long-term studies are needed to confirm these concepts.
Implant reconstructions are safe and well tolerated with low rates of major and minor complications (5). There were no cases of life-threatening complications (pulmonary embolus, myocardial infarction, major systemic complication) in a recent review of over 1,170 consecutive reconstructions performed at Memorial Sloan-Kettering Cancer Center (5). The majority of complications that did occur were minor and included skin necrosis (8.7%), infections (3.4%), infection requiring implant removal (1.5%), and seroma/hematoma (3.2%).
Capsular contracture is the most significant long-term risk with implant reconstructions and remains a problem even with improvements in implant technology and surgical techniques (7). The reported rates of capsular contracture vary significantly likely due to the fact that the diagnosis of this complication is somewhat arbitrary and not uniform. Most studies use the Baker scale as noted above; however, this scale has been criticized since it is not quantitative and primarily dependent on subjective assessment of “normal” or “abnormal” breast shape. This subjective assessment is likely responsible for the significant variability in the reported rates of capsular contracture and overall success rates of implant reconstructions in the plastic surgery literature.
Another important issue in comparing aesthetic outcomes in implant reconstruction is the methods used for analysis. By far the vast majority of previous studies have relied on photographic analysis by surgeons or laypeople to analyze various measures including symmetry, scars, volume, shape, and so on. Although these results are important and provide useful information, they do not address patient perceptions and may either over-or underestimate the success rates of various reconstructive needs. This deficiency
has been addressed recently with the use of validated patient reported outcome studies such as the Breast-Q, which aim to analyze how patients perceive their reconstruction in terms of physical, psychosocial, and sexual well-being as well as satisfaction with breast, outcomes, and care (13). The addition of these measures is exciting and provides surgeons with better insight about how patients perceive their reconstruction. This information can therefore help guide reconstructive techniques, preoperative teaching and preparation, and critical analysis of outcomes that can be standardized across centers.
has been addressed recently with the use of validated patient reported outcome studies such as the Breast-Q, which aim to analyze how patients perceive their reconstruction in terms of physical, psychosocial, and sexual well-being as well as satisfaction with breast, outcomes, and care (13). The addition of these measures is exciting and provides surgeons with better insight about how patients perceive their reconstruction. This information can therefore help guide reconstructive techniques, preoperative teaching and preparation, and critical analysis of outcomes that can be standardized across centers.
In the past, a major concern limiting access of patients to immediate reconstruction was a hypothetical increase in the risk of breast cancer or delay of diagnosis of a recurrence in this setting. However, several large-scale studies have shown that immediate reconstruction with implants has little effect on recurrence, survival, or diagnosis of recurrence (5). The majority of recurrences in these cases were skin or subcutaneous in nature and identified by routine physical exam or serological markers. For this reason, follow-up of patients with implant reconstruction is usually limited to careful physical exams rather than mammography or other radiological measures. Even when patients were discovered to have a recurrence, implant reconstruction in the majority of cases did not alter additional treatment (5).
A number of risk factors predict complications after implant based breast reconstruction. In a study of 1,170 consecutive reconstructions using multivariate analysis, McCarthy and colleagues demonstrated that obesity, hypertension, age greater than 65, and smoking were independent predictors of complications (2). The adjusted odds ratio of these factors ranged between 1.8 (obesity and smoking) to more than 2 (hypertension and age over 65). Univariate analysis of reconstructive failure demonstrated that obesity, smoking, and hypertension significantly increased the risk of reconstructive failure (i.e., implant removal).
Several studies have reported satisfaction with implant reconstructions and most have reported high rates of satisfaction in the early years following reconstruction. However, a consistent theme is decreasing satisfaction over time that may be attributable to a number of factors including lack of change in the implant over time, the need for implant maintenance (either for symmetry or due to rupture), and capsular contracture. Many of the reported studies have used nonvalidated questionnaires, thereby making their findings somewhat less useful. However, recent reports have begun to use validated patient reported outcomes in large populations of patients enabling us to better understand the factors that contribute to patient satisfaction AND dissatisfaction after mastectomy and implant reconstruction.
LATISSIMUS FLAP
The latissimus flap is a commonly used method for breast reconstruction and involves subcutaneous tunneling of the ipsilateral latissimus dorsi muscle with or without skin or subcutaneous tissues to the breast area (Fig. 36-3). In most patients the latissimus flap does not have enough volume for a full breast reconstruction, and for this reason, it is usually combined with an immediate implant or expander placement.
The latissimus flap can be used in primary breast reconstruction after mastectomy or as a salvage procedure for patients who have failed other forms of breast reconstruction. Although most surgeons use the latissimus flap for unilateral reconstructions, bilateral reconstructions have also been reported. The use of the latissimus flap enables the plastic surgeon to transfer a considerable amount of soft tissues to the breast and can result in excellent reconstructions particularly in women who have large, ptotic breasts, or those who have undergone a previous subglandular
breast augmentation. The latissimus flap is an excellent option in morbidly obese patients with massive breasts (14) and in smokers, although the risk of minor wound healing complications in this population remains elevated as compared with normal weight women and nonsmokers, respectively.
breast augmentation. The latissimus flap is an excellent option in morbidly obese patients with massive breasts (14) and in smokers, although the risk of minor wound healing complications in this population remains elevated as compared with normal weight women and nonsmokers, respectively.
The main contraindication to the latissimus flap is a previous thoracotomy operation that transects the latissimus muscle/pedicle, or a history of pedicle ligation. The blood supply or pedicle for the latissimus dorsi flap is the thoracodorsal vessels, which may on occasion be injured during the course of axillary lymph node biopsy or dissection. Testing the ability of the patient to flex the latissimus dorsi muscles is a simple way to test the integrity of the pedicle vessels since the thoracodorsal nerve, artery, and vein are intimately associated. Therefore, if the thoracodorsal nerve function is preserved it is likely that the vessels are likewise preserved. Even if the thoracodorsal vessels have been ligated, the latissimus flap can be transferred based on retrograde flow from the serratus anterior muscle-long-thoracic vessels, although these procedures increase the risk of venous hypertension.
A variety of skin paddle designs have been reported for the latissimus transferring a variable amount of skin and soft tissues to the breast. In some cases, no skin is necessary in which case the muscle can be harvested through several short incisions to decrease the donor site scarring. The horizontal (bra-line incision) is commonly performed and best for skin-sparing mastectomies in which the latissimus skin paddle is used to reconstruct the defect that remains after resection of the nipple-areola complex. The oblique flap design has a more noticeable donor site scar but is more useful if a larger skin paddle, such as may be needed in a delayed reconstruction, is necessary. The Fleur-de-lis modification combines both vertical and horizontal components and enables transfer of a large amount of tissues in many cases obviating the need for an implant (15). However, this flap design results in a T-shaped scar with a confluence of three incisions at the point of maximal tension and can be, as a result, associated with increased rates of donor site wound healing complications and contour deformity. Harvesting subcutaneous fat located below Scarpa’s fascia and transferring parascapular and lumbar fat together with the latissimus dorsi muscle can increase the volume of the latissimus flap and may obviate the need for an implant in some cases.
In most cases an implant is also necessary to obtain the necessary volume and projection of the contralateral breast. In some cases (i.e., skin-sparing mastectomy with good skin flaps) it is possible to place an immediate implant for reconstruction. However, most commonly, a tissue expander is placed in order to adjust for latissimus muscle atrophy and to more slowly expand the breast pocket. This expander is replaced as an outpatient procedure 3 to 5 months later with a permanent implant.
The latissimus flap has low complications rates with a very low reported incidence of total flap loss even in highrisk patients (e.g., obese) (14). However, partial necrosis of the distal portions of the flap does occur on occasion, particularly in smokers and obese patients. This region can usually be excised during the course of the procedure with limited consequences. The most commonly reported early complication of the latissimus flap is donor site seroma formation, resulting in prolonged need for subcutaneous drains. The incidence of this complication can be greatly decreased with quilting sutures placed in the subcutaneous tissues to close off the dead space that is created from wide skin flap elevation (16). Hematomas can also be problematic if care is not taken to securely ligate intercostal perforators to the flap.
Late complications of the latissimus flap include donor site pain or tightness, widened scar, decreased range of motion, and implant-related complications (17). Surprisingly, most patients do not complain of long-term weakness from latissimus harvest, although careful pre- and postoperative quantitative analyses of back muscle function have been performed only in relatively small studies (18). Widened scars may also occur as a consequence of these factors and is particularly problematic in oblique incisions since these incisions crosa relaxed skin tension lines. Unfortunately, these incision patterns are necessary in some patients because they provide the greatest amount of skin on the breast for reconstruction. Limitation of ipsilateral arm range of motion and frozen shoulder may be problematic in some patients (19). This is of particular concern in elderly patients, those previously treated with axillary lymph node dissection and radiation, and patients with preexisting shoulder pathology. Aggressive physical therapy and rehabilitation may be necessary in these cases.
Implant-related issues (infection, rupture, capsular contracture) are also a source of complications in latissimus flap reconstruction. The reported rates of infection after latissimus flap reconstruction are variable; however, most studies report low single digit rates of infection and implant/expander loss (20). The rates of capsular contracture after latissimus flap transfer have been reported by only a few studies and, although somewhat variable, the incidence of severe capsular contracture (Baker grade III or IV) is low (3.6%) (21). The rate of significant capsular contracture is increased in women with a history of prior breast irradiation even when reconstruction is performed with a latissimus dorsi flap. For example, in a retrospective study of 35 patients with prior breast irradiation treated with salvage mastectomy and latissimus dorsi flap reconstruction, Disa et al. found that 17% of patients developed grade III capsular contracture after a mean follow-up of 4.1 years (22).
ABDOMINAL FLAPS
In 1982, Hartrampf and colleagues pioneered the use of abdominal-based flaps for breast reconstruction and, in doing so, revolutionized modern breast reconstruction techniques (23). These authors demonstrated for the first time that large amounts of skin and subcutaneous fat can be transferred based on the blood supply of the rectus muscle, thereby enabling surgeons to reconstruct breasts without implants. More importantly, development of the transverse rectus abdominis myocutaneous flap (TRAM) flap demonstrated that it is possible to combine reconstruction with aesthetic principals and elevated the goals of reconstruction from “restoration of a breast mound” to a natural looking and feeling reconstruction that ages with the patient and in some cases is indistinguishable from a normal breast (Fig. 36-4). These concepts also applied to the donor site of the TRAM flap that, contrary to other options available at the time (i.e., latissimus dorsi flap), could actually improve the contour of the abdomen rather than create unsightly scars. Over the years, the techniques of TRAM flap reconstruction have evolved to limit donor site morbidity by decreasing the amount of rectus muscle and fascia that is harvested and improving the blood supply of the tissues. As a result of these advancements, the TRAM flap is considered the gold standard for aesthetic breast reconstruction by which all other forms of reconstruction are judged.
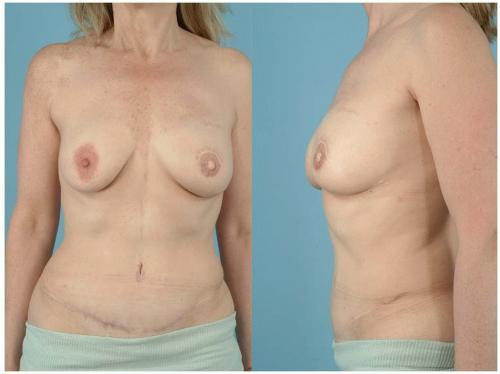 FIGURE 36-4 One-year postoperative photographs of a patient reconstructed with a left unilateral DIEP flap. |
The TRAM flap is indicated for unilateral or bilateral breast reconstruction in patients who have an appropriate body habitus and are motivated to have autologous reconstruction. The ideal patient for a TRAM flap has enough tissues in the lower abdominal areas to aesthetically replace the volume of the breast with adequate skin laxity to enable closure of the abdominal defect. TRAM flaps can also be used in some patients with adequate skin laxity but insufficient volume; however, in these cases an implant is usually needed to restore the projection of the breast.
Absolute contraindications for TRAM flap reconstruction are previous abdominal operations that have disrupted the blood supply of the TRAM flap. For example, the TRAM flap cannot be performed in patients who have previously undergone abdominoplasty. Relative contraindications for TRAM flap include smoking, the need for postmastectomy radiation therapy, severe medical comorbidities that may increase the risk of prolonged anesthesia or the risk of wound healing complications, and a desire for future pregnancy. A history of neoadjuvant chemotherapy (chemotherapy within 6 weeks of surgery) is associated with an increased rate of wound healing complications; however, in most cases these complications are minor and rarely cause significant morbidity (4).
In the past, many surgeons advised against TRAM flap reconstructions in patients who require postmastectomy chemotherapy; however, several large-scale studies have recently shown that adjuvant therapy is rarely significantly delayed in these patients. For example, in a 10-year retrospective study of 170 patients with stage IIB or worse breast cancer treated at UCLA Medical Center with microsurgical breast reconstruction, chemotherapy was delayed in only 8 patients (4.7%) with a maximal delay of 3 weeks (24). However, these conclusions have been debated depending on the definition of delay that is used. For example, in a relatively small study, Kontos and colleagues compared 27 patients who had immediate breast reconstruction with TRAM flaps with 139 patients who did not and found that the mean time to the start of adjuvant chemotherapy was delayed by 15 days (55 vs. 40) in patients who had immediate breast reconstruction with TRAM flaps (25). In addition, the authors found that fewer patients who had TRAM flap reconstruction initiated their adjuvant treatment within 6, 8, or 10 weeks. Similarly, Lewis and Kontos reviewed the current literature and found that the delivery of adjuvant therapy is delayed in 3% to 72% of patients who undergo autologous tissue reconstruction with an increase of 13% to 36% in the period of time needed to start chemotherapy as compared to patients treated with mastectomy alone (26). Whether or not these delays are clinically significant or if there is a difference when compared to other forms of breast reconstruction (i.e., implants) remains unknown. Nevertheless, patients who will require chemotherapy postoperatively should be advised of this risk in order to make an informed decision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree