urea and electrolytes or U&Es), a patient with dysfunctional renal output (as shown by a reduced estimated glomerular filtration rate (eGFR) of less than 60) may be less able to resolve a fracture and may be more predisposed to bone conditions. The PTH/VitD3 complex induces increased osteoclast activity in the bone, enhances Ca uptake in the gut and increases reabsorption of Ca in the kidney. The increased calcium (as a result of the PTH/VitD3 complex) is reabsorbed into the bone by the osteoblasts (B). The speed and frequency of this process is partly suppressed by the action of the hormone oestrogen (green circle).
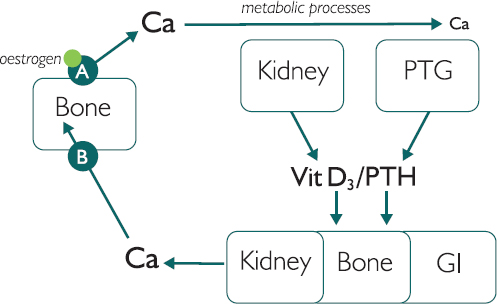
Figure 14.1: Normal bone turnover
In post-menopausal patients or those receiving long-term anti-oestrogen/progesterone treatments, this process is less regulated and more likely to result in frequent fractures, as the bone remodelling increases. This condition is called osteoporosis, and initial pre-menopausal bone mineral density (which is in turn controlled by diet, lifestyle and genetics) is an important factor in disease risk and progression. As the process is speeded up, variations in the blood components are difficult to observe. Thus, bone profile is not usually used in practice to diagnose or monitor osteoporosis. In elderly patients with chronic kidney disease, osteoporosis can be exacerbated. In addition to not being able to sustain VitD3 production, these individuals have compromised reabsorption of Ca, which increases their risk of fracture and the time needed for any fractures to heal.
Paget’s disease
In Paget’s disease there is a dysfunctional regulation of the osteoclast and osteoblast pathway. This leads to imperfect removal and reabsorption of Ca.
Storytelling: Imagine repairing a road. Team A (osteoclasts) remove two buckets of rubble (Ca) from the road (bone) and dispose of the Ca by using it to make muscle, nerves and teeth. But they tell Team B that they have taken out 20 buckets of rubble. The foreman (PTH) therefore insists that Team B (osteoblasts) use 20 buckets to refill the hole (even though there is only room for two buckets of rubble). Thus, the road will not return to its original flat surface. Instead, a bump will be left.
In practice, this process leads to bone protrusions and pain. A raised Ca level is sometimes seen in patients with immobility due to joint degradation, as the sockets and joints are ill formed.
Drugs like bisphosphonates work by binding to calcium in the bone, which then suppresses osteoclast activity, thus improving and maintaining bone mineral density. Bisphosphonates are therefore often used to treat osteoporosis and Paget’s.
Osteomalacia
Patients with a vitamin D deficiency can be predisposed to osteomalacia, known as rickets in children. Vitamin D is obtained from the diet and stored in the skin. There, under the action of UV light, it is converted into vitamin D2 (calcidiol), which is stored in the liver. Vitamin D2 is then transported to the kidney, where it is converted, by a parathyroid hormone (PTH) induced enzyme, into vitamin D3 (calcitriol 1,25 (OH)2D). Inadequate production of vitamin D3 often results in hypocalcaemia, leading to dysfunctional bone remodelling and eventually weak bones that ‘bend’ under the weight of the trunk. Causes of vitamin D3 deficiency may be a lack of UV light, too little vitamin D in the diet, or the presence of chemicals in the diet that can block vitamin D3 absorption in the gut (seek advice from dietetics), or renal impairment as in chronic kidney disease. Blood test results in osteomalacia are often low Ca, high PTH, as the parathyroid attempts to correct the low Ca, and low phosphate, as PTH increases excretion in the urine ( eGFR for renal status).
eGFR for renal status).
Magnesium
Other tests that may be returned are magnesium (Mg), alkaline phosphatase and phosphate. Magnesium is required to produce PTH so a magnesium deficiency will restrict PTH and thus the availability of free Ca. Hypomagnesaemia is common in alcoholic patients, due to malnutrition, diarrhoea and increased excretion; the latter is also seen in diabetic keto-acidosis. Some thiazide and loop diuretics, antibiotics, proton pump inhibitors, pancreatitis and gastrointestinal (GI) disorders (such as Crohn’s) may also lead to low Mg levels.
Alkaline phosphatase
Alkaline phosphatase (Alk Phos) is an enzyme found within the bone, liver, kidney and placenta and is a helpful differential. For example, if a patient has a raised Alk Phos under the LFT, but all other LFT values are normal (as are the U&Es), this could suggest that the cause of the raised Alk Phos could be bone – especially with a raised Ca.
Phosphate
Phosphate forms a complex with Ca to provide the structure of bone. Phosphate levels are mainly controlled by renal output and impairment. Low levels can be a red flag, as this can lead to respiratory failure – given the control of muscle by Ca and Phosphate.
Calcium
Whilst 99% of calcium is stored in the bone, the remaining 1% is bound to albumin as a transport protein and free, biologically active Ca. Therefore, a low albumin level, as in malnutrition or liver damage ( LFT), may cause an artificially low Ca. Hence, ‘corrected’ calcium is used, which corrects the Ca for the levels of albumin. Generally, corrected Ca is used in clinical practice. Ca levels are controlled by osteoclasts, osteoblasts, parathyroid hormone, vitamin D (from UV light and the kidney) and the negative feedback hormone calcitonin. Bone profiles are helpful in order to assess some dysfunctional bone conditions such as osteomalacia; as a differential of bone pain as seen in myeloma; and to assist in determining a secondary bone metastasis (bony mets), which would be an unregulated increase in Ca.
LFT), may cause an artificially low Ca. Hence, ‘corrected’ calcium is used, which corrects the Ca for the levels of albumin. Generally, corrected Ca is used in clinical practice. Ca levels are controlled by osteoclasts, osteoblasts, parathyroid hormone, vitamin D (from UV light and the kidney) and the negative feedback hormone calcitonin. Bone profiles are helpful in order to assess some dysfunctional bone conditions such as osteomalacia; as a differential of bone pain as seen in myeloma; and to assist in determining a secondary bone metastasis (bony mets), which would be an unregulated increase in Ca.
Raised calcium (hypercalcaemia) may be caused by a primary hyperparathyroidism, a tumour secreting a PTH-like compound (for all PTH investigations, these are diurnal, so check the timing of the test), over-supplementation of calcium and vitamin D, renal failure, sarcoidosis, myeloma, bone fractures and bone cancer (primary and secondary). It may also be due to inappropriate blood collection.
Low calcium (hypocalcaemia) can therefore be due to low albumin, vitamin D deficiency, renal failure, or damage to the parathyroid gland as is sometimes seen after thyroid surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree