III.A.001 Anaplasmosis (Ehrlichosis)
III.A.001
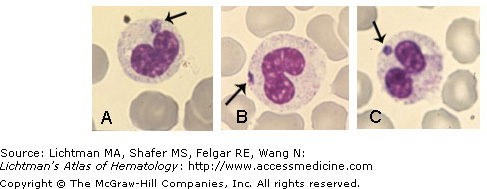
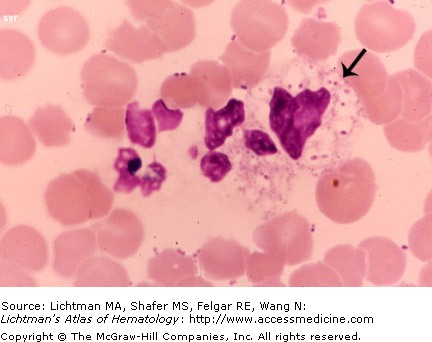
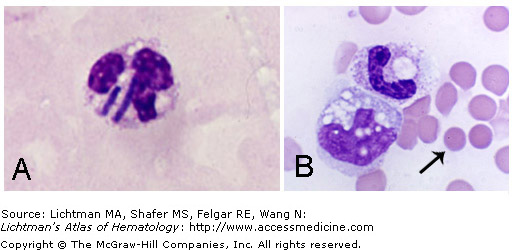
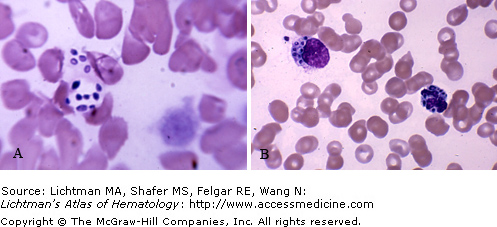
Anaplasmosis (Ehrlichosis). Blood film showing intracellular Anaplasma (arrows). Anaplasmosis is caused by the bacterium Anaplasma phagocytophilum, a genus assigned to the family Rickettsiae. The organism was previously called Ehrlichia phagocytophilum and the disease Ehrlichosis before the names were changed. Human Granulocytic Ehrlichiosis is now called Human Granulocytic Anaplasmosis. The bacterium is transmitted to humans by the bite of a tick. Headache, fever, chills, malaise, and muscle aches are the most common symptoms. Rash is very uncommon. These symptoms occur within 1 to 2 weeks of a tick bite. Anaplasmosis can be suspected based on the clinical presentation, a history of a tick bite (often this is not recalled), a low white blood cell count and low platelet count (present in half the cases), and elevated levels of liver enzymes. Severe clinical presentations may include difficulty breathing, hemorrhage, renal failure or neurological problems. Anaplasmosis can be a serious illness that can be fatal if not treated correctly. The organism is an obligate parasite of neutrophils as shown in this image and undergo their life cycle in leukocytes and platelets. A firm diagnosis is made using the polymerase chain reaction or by immunostaining.
III.A.002 Aspergillosis
III.A.002
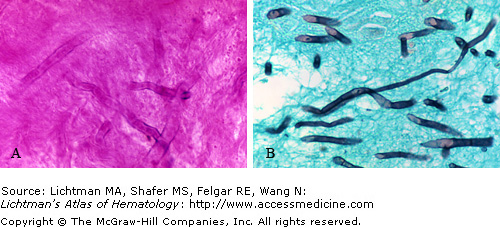
Aspergillosis. Periorbital skin biopsy. (A) Hematoxylin and Eosin stain. (B) Gomori methenamine-silver stain. Note hyphae of Aspergillus sp. (probably fumagatum). This ubiquitous organism may infect patients receiving allogeneic stem cell transplantation or chemotherapy for acute leukemia. The sinuses and lungs are common sites of infection.
III.A.003 Babesiosis
III.A.003
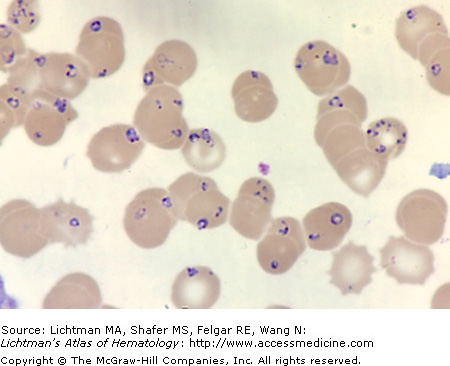
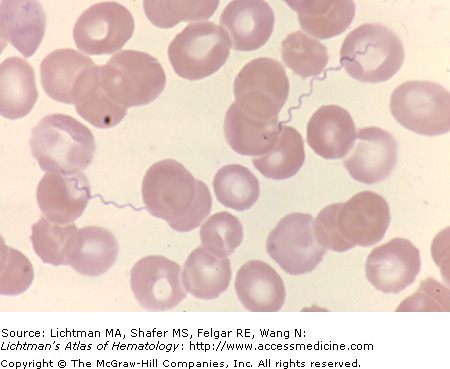
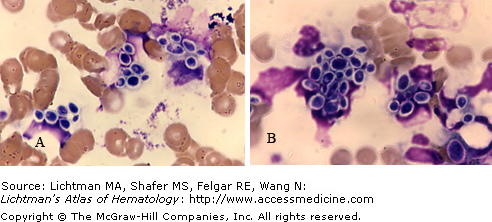
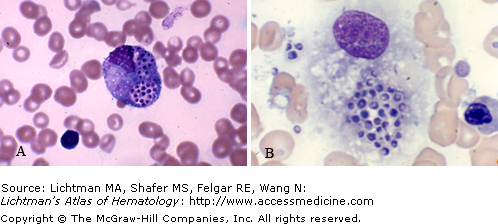
Babesiosis. Blood film. Babesia microti. A protozoan infection by the organism Babesia sp., usually Babesia microti in humans. The organism parasitizes red cells as shown in this blood film. Careful examination of this slide did not show schizonts or hematin pigment as would be expected in heavy infection by P. falciparum. Moreover the very intense parasitemia is more characteristic of Babesiosis. Microorganism nuclei in pairs or tetrads, some in cross configuration, are common in the red cells in Babesiosis, distinguishable from malarial ring forms.
III.A.004 Babesiosis microti
III.A.004
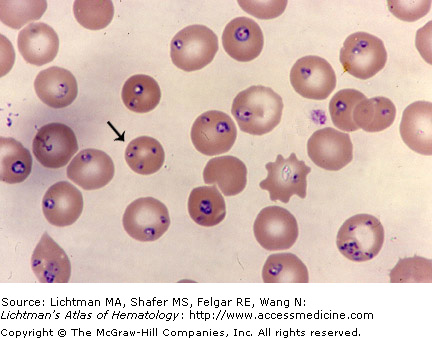
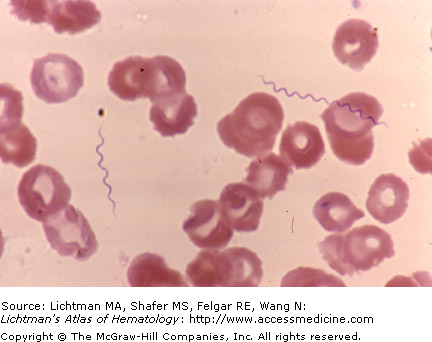
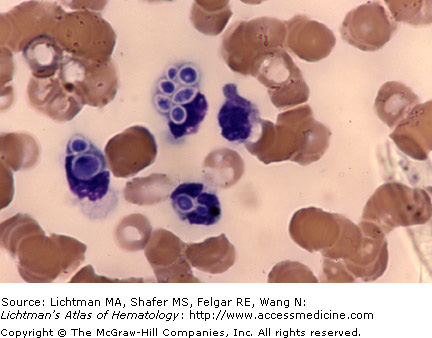
Babesiosis. Blood film. A protozoan infection by the organism Babesia, usually Babesia microti in humans. The organism parasitizes red cells as shown in this blood film. The arrow points to one of many parasitized cells. The field shows a very high level of parasitemia with numerous ring forms very similar in size and configuration to Plasmodium falciparum. Careful examination of this slide did not show schizonts and hematin pigment as would be expected in heavy infection by P. falciparum. Moreover the very intense parasitemia is more characteristic of Babesiosis. Microorganism nuclei in pairs or tetrads, some in cross configuration, are common in the red cells in Babesiosis. The arrow indicates a Babesial tetrad.
III.A.005 Bacterial Infection
III.A.006 Borreliosis
III.A.007 Borreliosis (Lyme Disease)
III.A.008 Candidiasis
III.A.009 Clostridial Sepsis
III.A.009
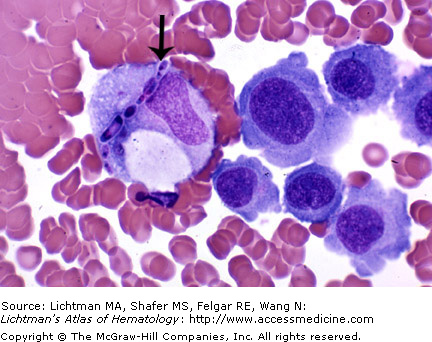
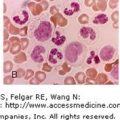
Clostridial sepsis. (A) Blood film. Clostridia perfringens. Organisms in a neutrophil in a case of Clostridial sepsis. (B) Vacuolated band neutrophil and multivacuolated monocyte in the same case of Clostridial sepsis as in (A). Note spherical red cells characteristic of this endotoxemia (arrow).
III.A.010 Cryptococcosis
III.A.010
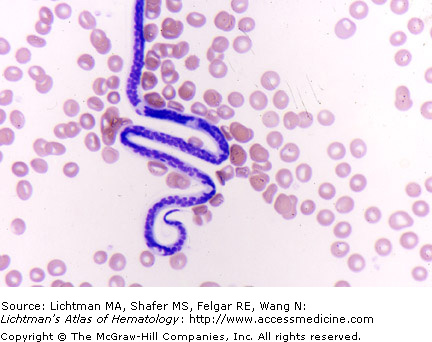
Cryptococcosis. Blood films (A, B). Aggregates of Cryptococcus neoformans in phagocytes or free in plasma. Cryptococcus neoformans grows as yeast and replicates by budding. C. neoformans makes hyphae during mating, and eventually creates basidiospores at the end of the hyphae before producing spores. The cells produce a characteristic polysaccharide capsule. The clear zone around each yeast form in these images represents the capsule. India ink, which does not penetrate the capsule but does the body of the yeast, is used to diagnose the organisms in cerebrospinal fluid in cases of meningitis or meningoencephalitis. The organisms take on a dark appearance with a clear halo. The cryptococcal antigen test of blood or cerebrospinal fluid can confirm the diagnosis.