Biopsy of Musculoskeletal Tumors
Edward A. Athanasian
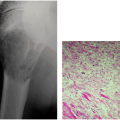
Biopsy of musculoskeletal bone and soft tissue tumors may appear to be a deceptively easy technical surgical procedure. Patients may also perceive biopsy as a relatively straightforward, low-risk procedure. While many aspects of the biopsy procedure require only basic technical skills, the proper execution of biopsy of extremity lesions requires careful preparation and planning, plus exacting technique. Errors made at the time of biopsy may not become apparent until the time of surgical resection or recurrence.
Risks of Improper Biopsy
Most extremity bone and soft tissue tumors are benign. Fortunately, the risks of suboptimal biopsy when performed on benign lesions are minimal. The risks of biopsy of malignant lesions are much greater. Insufficient planning and poor execution have the potential to complicate subsequent definitive treatment if the lesion under consideration must be definitively treated surgically. Inadequate biopsy has the potential to increase the risk to the patient’s life, as demonstrated in studies performed by the American Musculoskeletal Tumor Society. If the risks of biopsy are carefully considered, it becomes very clear that fundamental understanding of planning and executing a biopsy is imperative to maximize the ability to perform limb salvage surgery and maximize patient survival.
Improper incision placement or orientation
May compromise and complicate attempts at subsequent limb salvage
May result in need for performing amputation specifically as a result of the biopsy
In studies reported by the American Musculoskeletal Tumor Society, amputation was required specifically because of improper biopsy placement in as many as 18% of patients.
May result in need for more extensive amputation than otherwise might have been necessary
Improper excisional biopsy
Associated with greater risks than incision biopsy or needle biopsy
Specific anatomic regions such as the axilla, antecubital fossa, carpal tunnel, groin, and popliteal fossa are specifically at risk for contamination when excisional biopsy is performed.
Soft tissue contamination produced following marginal excision of malignant lesions must be excised at the definitive surgical excision.
Extensive contamination increases the amount of soft tissue that needs to be resected.
Results in a greater need for soft tissue coverage to close wounds
Indications for Biopsy
Lesions That Do Not Require Biopsy
Many benign bone and soft tissue tumors can be readily recognized clinically or radiographically and do not require biopsy to establish a diagnosis (Table 3-1).
Lesions That Require Biopsy
Lesions that are not readily recognized based on clinical examination or radiographic assessment should be considered for biopsy. Even innocuous-appearing soft tissue lesions that are painless and may have been present for a long period of time without growth must be considered for biopsy if a differential diagnosis limited to benign lesions only cannot be made. The rule of thumb is that if the clinical and radiographic diagnosis cannot be limited to benign lesions only, biopsy or referral to a specialist is indicated.
Soft tissue sarcomas frequently present as painless masses that have been present for a long period of time with recent change in size. Synovial sarcomas are notorious for this sort of behavior.
Types of Biopsies
Box 3-1 lists the types of biopsies used for musculoskeletal tumors, some of which are discussed in detail below.
Table 3.1 Soft Tissue and Bone Lesions That Can Usually be Recognized Clinically or Radiographically | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Box 3-1 Biopsy Types Employed for Musculoskeletal Tumors
Fine-needle aspiration/biopsy
Core-needle biopsy
Open incisional biopsy
Open excisional biopsy
Primary wide excision
Fine Needle Aspiration (FNA)/Biopsy (Skinny Needle)
Setting
In the office under local anesthetic
In the radiology suite
Under ultrasound guidance for soft tissue biopsy
Under computed tomography (CT) guidance for bone lesion biopsy
Technique
Soft tissue
Small-gauge needle on syringe used to aspirate cells during multiple passes in several directions via single entry site
Cells collect in syringe or hub of needle and are examined on glass slides, often immediately after biopsy performed
Bone
Fine-needle aspiration biopsy of bone tumors may require additional anesthetic, depending upon site and need to enter bone.
If no soft tissue extension of process from bone, may require larger-gauge needle or drill to enter bone
Usually done under CT guidance
General Principles
Provides cells (cytology) but no true pattern of organization
Site and pathway for the needle need to be planned such that they can be incorporated into a standard limb salvage incision in the event wide excision of the tumor is subsequently required.
Needle placement must not compromise amputation flaps in the event amputation is chosen as the most appropriate treatment for the lesion in question.
Advantages
Principal advantage is the rapidity with which lesional tissue can be obtained and the histologic diagnostic process started.
Less costly than a hospital-based procedure
Limited discomfort for the patient
Limited soft tissue contamination
Limited risk as long as the biopsy site, needle entry point, and needle course are carefully planned
Disadvantages
Limited material to examine means lower likelihood of achieving specific diagnosis.
Usually performed by radiologist without detailed knowledge of need for appropriate placement of needle tract
Negative biopsy does not reliably exclude neoplasm.
Negative result often requires repeat aspiration or biopsy by another technique.
Indications
Relatively inaccessible lesions of bone and soft tissue
Confirmation of strong clinical suspicion of metastatic disease or sarcoma recurrence
Results
Diagnostic accuracy rate 64% to 88% for musculoskeletal tumors
Diagnostic accuracy is lower for benign tumors.
Needle Biopsy (Core-Needle Biopsy)
Setting
Same as for fine-needle biopsy
Technique
Soft tissue
A special hollow needle with a cutting mechanism retrieves a cylindrical core of tissue approximately 2 mm in diameter and several millimeters in length, depending upon the specific type of needle used.
Typically two or three passes of the needle are made.
Bone
Core-needle biopsy of bone tumors usually requires a heavier anesthetic.
Performed with a hollow trephine-type needle with much larger diameter (4 to 7 mm)
Usually done under fluoroscopic guidance, often with frozen section analysis done to confirm the presence of lesional tissue
General Principles
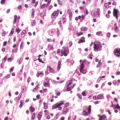
Provides for evaluation of pattern of tissue organization and cellular features
Placement of needle should follow same principles as for skinny needle.
Advantages
Provides more tissue for evaluation than fine-needle aspiration, with additional component of the pattern of organization
Otherwise same advantages as for fine-needle aspiration/biopsy (rapidity of diagnosis; limited cost, discomfort, contamination, risk)
Disadvantages
Principal disadvantage pertains to the limited size of the tissue sample obtained, which has the potential to reduce accuracy and result in sampling error.
Molecular diagnostic testing, which can be particularly useful in difficult cases, may not be able to be done if inadequate tissue has been obtained to allow initial processing to prepare for this potential need.
Indications
Core-needle biopsy is most often indicated for superficial or accessible deep extremity lesions that are of sufficient size to allow needle placement (>3 cm) and that do not involve major neurovascular structures.
Results
Diagnostic accuracy rate 83% to 93% for musculoskeletal tumors
Diagnostic accuracy is lower if the lesion is thought to be benign.
Open Biopsy (Incisional or Excisional)
Setting
Typically in the operating room under general anesthetic with pathologist standing by for frozen section analysis to confirm adequacy of tissue
Advantages
Principal advantage relates to the larger size of the tissue sample obtained, reducing the risk of sampling error and allowing for more extensive histologic assessment as well as molecular diagnostic assessment when needed.
Gold standard in achieving high diagnostic accuracy
Disadvantages
Principal disadvantage of open biopsy is potential for improper execution by surgeon.
Potential adverse consequences of tissue contamination/exposure during open biopsy
Any tissue exposed or manipulated at the time of biopsy is potentially contaminated with tumor cells.
Any hematoma or seroma that develops has the potential to further contaminate local soft tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree