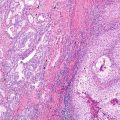
Fig. 16.1
A primary lung cancer (left panel) involving the lung of a non-smoker patient treated for recurrent NSCLC with multiple cycles of chemotherapy and radiation. The patient had involvement of multiple organs (liver, adrenal, and bone) that led to multiple organ failure and disseminated disease in multiple organs
Table 16.1
In the International Adjuvant Lung Cancer Trial IALT study, the incidence of either local or distant recurrence was significantly lower in the chemotherapy arm compared with the control arm. The brain was the most frequent site of metastasis (30%) and the incidence of brain metastasis (BM) was not significantly different between the two arms, whereas the incidence of metastases at other sites was significantly lower in the chemotherapy arm compared with the control arm
Total no. events | Cisplatin-based chemotherapy (n = 932) (%) | Control (n = 935) (%) | Hazard rate | P | |
|---|---|---|---|---|---|
Overall survival rate 5 years | 973 | 44.5 | 40.4 | 0.86 | 0.03 |
Disease-free survival rate | 1095 | 39.4 | 34.3 | 0.83 | 0.003 |
Local recurrence incidence | 379 | 24.3 | 28.9 | 0.72 | 0.003 |
Distant recurrence incidence | 655 | 40.8 | 44.3 | 0.84 | 0.03 |
Brain as first metastasis incidence | 227 | 18.1 | 16.3 | 1.07 | 0.61 |
Non-brain as first metastasis incidence | 456 | 29.4 | 34.9 | 0.75 | 0.003 |
Second primary incidence | 78 | 6.0 | 6.9 | 0.90 | 0.64 |
Liver Metastases
Symptomatic hepatic metastases are uncommon early in the course of the disease; asymptomatic liver metastases may be detected at presentation by liver enzyme abnormalities, CT or PET imaging. Among the patients with otherwise resectable NSCLC in the chest, CT evidence of liver metastases has been identified in approximately 3% of the cases. Newer imaging techniques (PET or integrated PET/CT) identify unsuspected metastases in the liver or the adrenal glands respectively in about 4% of the patients. The incidence of liver metastasis is much higher later in the course of disease once the tumor progresses and spreads to distant organs. Autopsy studies have shown that hepatic metastases are present in more than 50% of the patients with either NSCLC or small cell cancer.
Adrenal Metastases
The adrenal glands are a frequent site of metastasis but are rarely symptomatic. Only a fraction of adrenal masses detected on staging scans represent metastases. In a series of 330 patients with operable NSCLC, 10% had isolated adrenal masses [10]. Only 8 out of 32 (25%) were malignant, while the remainder had benign lesions like adrenal adenoma, adrenal nodule hyperplasia, or hemorrhagic cysts. Conversely, negative imaging studies do not exclude adrenal masses and a study of patients that had SCC found that at least 17% of adrenal biopsies showed metastatic involvement despite normal CT scans [11]. The lack of specificity of initial CT identifying an adrenal mass creates a special problem in patients with an otherwise resectable lung cancer. Involvement of the adrenal glands is more frequent in patients with widely disseminated disease. In an autopsy series that have been previously published, adrenal gland metastases have been identified in 40% of patients with lung cancer.
Bone Metastases
Metastases from lung cancer to bone are frequently symptomatic. Patients present with pain and elevated levels of alkaline phosphatases. Twenty percent of patients with NSCLC have bone metastases at presentation and osteolytic appearances are more common than osteoblastic ones. The most common sites of involvement are the vertebral bodies. Bone metastases are even more common in patients with SCLC, and represent 30–40%. Modern imaging studies (PET and PET/CT) have improved the ability to identify metastases to many organs including bone, with greater sensitivity than CT or bone scan.
Brain Metastases
Lung cancer is the malignancy that most commonly gives rise to brain metastasis which is a devastating complication [12]. Brain metastases are a major cause of morbidity and mortality in human malignancies in patients wit h NSCLC. The frequency of brain metastasis is greatest with adenocarcinoma and least with squamous cell carcinoma . Approximately 10% of the patients have brain metastases at the time of diagnosis, and approximately 40% of all patients with lung cancer will develop brain metastases during the course of the disease [13]. Patients with locally advanced NSCLC who are treated with chemotherapy and chest radiotherapy with or without surgery have a very high rate of developing brain metastases [14–17]. These patients also have a risk that ranges from 15 to 30% of failing first in the brain. Brain metastases from NSCLC have received increasing attention, because combined-modality therapy has led to improvements in intrathoracic local control and prolonged overall survival [18–20]. The risk for brain metastasis increases with larger primary tumor size and regional node involvement (which is a well-known phenomenon at the basis TNM staging system). For carefully selected patients, surgical resection may be feasible. Surgical resection of brain metastases may be feasible in cases that have operable NSCLC in the chest and solitary brain metastases. In patients with SCLC, metastases to brain are present in 20–30% at initial diagnosis. Without prophylactic irradiation, relapse in the brain occurs in 50% within the next 2 years after the diagnosis. Randomized trials have shown that the frequency of brain metastases can be significantly reduced with prophylactic cranial irradiation. It is important to identify the patients with NSCLC who are at greater risk of developing metastases because such metastases may exist in the absence of neurologic symptoms [21]. Furthermore, prophylactic cranial irradiation may be an effective modality preventing brain metastases in patients with NSCLC who receive adjuvant chemoradiation [16]. Despite advances in diagnosis, therapeutic modalities, and clinical practice guidelines, it remains unclear whether patients with NSCLC should be screened for brain metastases or not [22, 23].
Molecular Characteristics of Metastases in Comparison with Primary Tumor
Recent studies have advanced the hypothesis that there may be important differences in the primary tumor , lung tumor, and metastases of lung adenocarcinoma, regarding morphology, biomarker expression, and genotype [24]. The mutation status of metastases can differ from the primary tumors and also among metastases [3, 25]. The frequency of differences and the significance of the differences in pathologic variables between primary lung tumors and metastases and also previously systemically treated tumors have yet to be fully investigated [25, 26]. Both the cells within the primary tumor and the metastatic lesions can continue to diversify if the lesions grow and result in molecular differences between the primary and the metastatic tumor. To determine whether the genetic profiles are similar between the primary lung cancer and their paired metastases to the brain, we examined pairs of primary metastatic lung carcinomas by high-throughput genetic mutation profiling. We evaluated four-micron formalin-fixed paraffin embedded specimens from patients with lung cancer (women 52% and men 48%) with a median age of 65 years. The tumors investigated were 12 adenocarcinomas and nine squamous cell carcinomas and the corresponding brain metastases they developed after a median of 12.5 months (range 2–90 months) over a 35-month median follow-up time. We employed the sequenom mass spectrometry-based system (IPLEX protocol-oncomap analyses) for 252 genetic mutations in the following genes: ABL1, BRAF, EGFR, FGFR3, HRAS, KRAS, MET, N-ras, PBGFRA, PI3K, and RET. Some of the lower confidence mutations identified by IPLEX protocol were validated by homogeneous mass-extended (HME) technology . We found that nine patients (39.1%) had mutations only in the primary tumors Table 16.2. In five patients (21.7%) mutations were identified only in the brain metastases and in only three patients (13%) mutations were identified in both lung and brain metastases (Table 16.2). Except K-ras G12C mutation that was identified in two patients, all mutations were unique in each patient.
Table 16.2
Molecular characteristics of matched primary NSCLC and brain metastases
Gene | Present only in primary NSCLC | Present only in metastasis to brain | Present in both primary NSCLC and brain |
|---|---|---|---|
ABL1 | Y253F | G250E | |
BRAF | D594G | D594G | D594G (one case) |
EGFR | Exon19 del, D770_N771>AGG | ||
FGFR3 | K650T | ||
HRAS | G13D | ||
KIT | V559I | ||
KRAS | G12C | G12S; G12D; G12C | G12C (two cases) |
PDGFRA | T674I | ||
PI3K
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|