© Springer International Publishing AG 2018
Philip T. Cagle, Timothy Craig Allen, Mary Beth Beasley, Lucian R. Chirieac, Sanja Dacic, Alain C. Borczuk, Keith M. Kerr, Lynette M. Sholl, Bryce Portier and Eric H. Bernicker (eds.)Precision Molecular Pathology of Lung CancerMolecular Pathology Libraryhttps://doi.org/10.1007/978-3-319-62941-4_1313. Predictive Biomarkers for Squamous Cell Carcinoma
(1)
Department of Pathology and Genomic Medicine, Houston Methodist Hospital, Houston, TX, USA
(2)
Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, New York, USA
Keywords
Lung cancerSquamous cell carcinomaImmune therapyPredictive biomarkerTherapeutic options for non-small cell lung cancer (NSCLC) have significantly grown in the last years; however, these novel therapeutic options have almost exclusively targeted non-squamous NSCLC. Therapeutic advancements made over the last decade have focused on the concept of “driver mutations ,” particularly alterations in kinase genes or other pathways thought to be essential for tumor cell growth and development [1]. Kinase inhibitors have improved survival in patients with the corresponding actionable mutations or translocations after laboratory testing for these predictive biomarkers in tumor samples; however, these actionable mutations and translocations are almost exclusively seen in patients with non-squamous NSCLC histology.
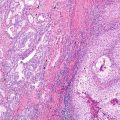
Squamous cell carcinoma of the lung has a very high relative mutational burden when compared to other malignancies [2]. Despite this high mutational burden, a targetable mutation has not been identified to date [3]. The high mutational burden, high immunogenicity (relevance discussed later), and lack of a currently identifiable actionable driver mutation correlate with cigarette smoking exposure [4, 5] typical of lung squamous cell carcinomas [1]. Although the number of lung squamous cell carcinomas has fallen over the last decades, it remains a common cancer annually accounting for over 400,000 new cancer cases globally and around 85,000 new cancer cases in the United States [1]. As such, more promising therapeutic options are sought compared to the current standard chemotherapy regiments.
A variety of common genomic alterations have been identified in squamous cell carcinoma of the lung, the most common being loss of TP53 and CDKN2A [6, 7]. Numerous other alterations are frequently identified, and some have been identified as potential therapeutic targets. For example, FGFR1 amplification (the most studied to date), PIK3CA mutation and PTEN mutation/deletion, EGFR amplification/protein overexpression, PDGFRA amplification/mutation, and DDR2 mutation [8] have all been identified as potential targets with potential corresponding predictive biomarkers. Unfortunately, clinical trials with novel therapies have been plagued by low response rates to date. Despite the lackluster success seen thus far, there is ongoing research in the field of squamous NSCLC. One such example being SOX2 overexpression in mice models seemingly promotes the development of squamous cell carcinoma over adenocarcinoma [9]. Perhaps as we begin to further understand the intricacies of known and currently unknown molecular and cellular pathways, more promising targeted treatments with corresponding predictive biomarkers will emerge for squamous NSCLC.
As stated earlier, tumors related to cigarette smoking exposure (like squamous NSCLC) tend to be highly immunogenic. A relatively recent advancement in the treatment of NSCLC in general (both squamous and adenocarcinoma histology) is the development of immune checkpoint therapy, particularly therapy blocking the interaction between PD-1 and PD-L1. PD-1 is expressed on T-cells, and the T-cell immune response is dampened when PD-1 is bound to its ligand (PD-L1) [10] essentially resulting in a T-cell anergic response. As such, upregulation of PD-L1 expression in tumor cells enables them to escape the immune response in a process sometimes referred to as “adaptive resistance ” [11]. Monoclonal antibodies targeting PD-1 or PD-L1 block the interaction and allow the immune system to recognize and attack tumor cells; these checkpoint inhibitor immunotherapies have shown remarkable responses in some patients [12, 13]. Immunohistochemistry for PD-L1 has been used as a predictive biomarker to identify patients who may respond favorably to therapy. However, immunohistochemical evaluation has its challenges. Firstly, there are multiple anti-PD-L1 antibodies available or in development, each approved for a different drug. It is not practical or feasible for pathology laboratories to perform multiple different immunohistochemical assays for a single protein. Performing multiple assays would require numerous tissue sections, potentially exhausting tissue blocks for other testing (i.e., other molecular studies for therapeutic decision making). Additionally, none of the available immunohistochemistry assays have been validated for cross-utilization at this time. Secondly, there is significant heterogeneity of PD-L1 expression in tumors [14], and often only a small biopsy specimen is tested in practice; as such the PD-L1 protein expression may be misrepresented on small biopsy specimens. Thirdly, positive or negative staining does not always correspond to therapeutic response [15–17]. Despite these limitations, immune checkpoint therapy associated with PD-L1 biomarker testing is another treatment option for squamous cell carcinoma and other NSCLC with some patients having dramatic responses. As our knowledge of immunotherapy advances, additional predictive markers may emerge, and evaluation of single or multiple proteins expressed by squamous cell carcinomas and other NSCLC may help better identify patients who will respond to such treatment regimens.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree