Type of benign mesothelioma
Characteristics
Benign multicystic mesothelioma
Well-differentiated papillary mesothelioma
Benign adenomatoid type of mesothelioma
Predilection
Young to middle-aged women
Reproductive age women
Reproductive age women and men
Predisposing factor
Previous surgery or pelvic inflammatory disease
Not known
Not known
Clinical course
Hormone sensitive
Indolent course, rare malignant change
Indolent course, rare malignant change
Computerized tomography imaging
Multilocular cystic mass, multiple unilocular thin walled cysts, or unilocular cystic mass
Peritoneal thickening, multiple peritoneal nodules, omental infiltration, and ascites
Non-specific
Differential diagnosis
Cystic lymphangioma
Endometriosis
Cystic epithelial neoplasms of the ovaries
Pseudomyxoma peritonei
Peritoneal metastases
Serous papillary carcinoma of peritoneum
Tuberculous peritonitis
Solid type of metastatic intraperitoneal and retroperitoneal tumours
Testicular tumours
10.2 Diagnosis
Most patients are diagnosed incidentally, and clinical findings are also non-specific such as nausea, vomiting, and abdominal pain. However, retroperitoneal mass [10] or acute abdomen due to incisional incarcerated hernia [11] could also be developed in some cases. The palpable fixed mass always presents with tenderness on physical examination. We have reported a case with an incisional hernia, an abdominal discomfort, and a mass surrounded to the umbilicus due to BMPM [12].
Laboratory findings are non-specific for diagnosis of BMPM. An association between BMPM and increased serum CA 19–9 concentration has been described, and a minimally invasive laparoscopic approach enabled both diagnosis and surgical treatment of the disease [13].
Imaging features vary according to the appearance of this tumour. BMPM usually consists multiple cysts but it could be unilocular. Multiseptated cysts can be demonstrated by ultrasonography. However, computerized tomography (CT) is necessary to provide information about the extent and anatomic localization of the disease (Fig. 10.1). In some cases, the omentum can be invaded with multicystic mesothelioma. In our previous report, an intraperitoneal hypodense cystic mass surrounded the umbilicus and extended between the great curvature of the stomach, spleen, and tail of the pancreas extending caudally to the upper margin of the pelvis and resulted with hernia from midline incision scar with CT (Fig. 10.2) [12].
Fig. 10.1
T2-weighted coronal MRI image shows multiloculated cysts which occupied nearly the entire abdominal cavity and omental metastasis of BMPM. Cysts are noncommunicating in abdominal viscera but scalloping to small bowel and its mesentery
Fig. 10.2
Computed tomography images of the BMPM: the arrows indicate the incisional hernia (A), multicystic mass surrounded to umbilicus (B), and intraabdominal extension (C)
BMPM can also be determined with magnetic resonance imaging (MRI) that shows hypointense well-defined lesions on T1-weighted images and isointense clear watery fluid as intermediate signal intensity on T2-weighted images [14].
Radiological differential diagnosis is made with cystic lymphangioma, cystic epithelial neoplasms of the ovaries [9]. Pseudomyxoma peritonei may rarely resemble BMPM.
Because BMPM is extremely rare disease, preoperative diagnosis is also challenging. Laparoscopy remains the best diagnostic method that enables to establish the definitive diagnosis with obtaining biopsy. Therefore, we recommend diagnostic laparoscopy and laparoscopic biopsy both from cystic fluid and from tissue specimens.
Multiple floating cysts (Fig. 10.3), widespread multicystic nodular thickening of the visceral peritoneum (Figs. 10.4, 10.5, and 10.6), can be determined during laparotomy or laparoscopic exploration.

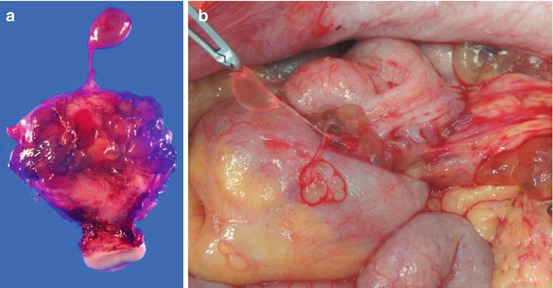

Fig. 10.3
Peritoneal floating cysts (*) and cysts connect with thin stalk to the peritoneal surface
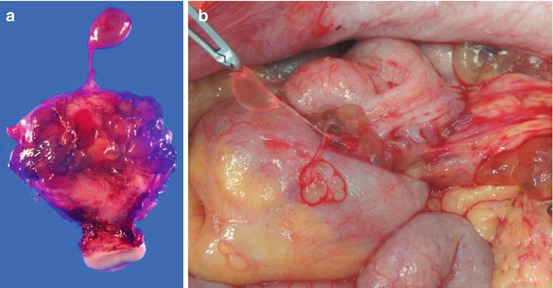
Fig. 10.4
(a) Resected BMPM showing multiple fluid-filled cysts on the uterus. Cysts connected with fine stalks from uterine surface. (b) Cysts are connected with serosal surface of the visceral organs and omentum
Fig. 10.5
Resected multicystic mesothelioma showing fluid-filled cysts on the caecum (a). Cyst was also found on greater omentum with haemorrhagic fluid (b)
Fig. 10.6
(a) Cysts on greater omentum above the hepatic flexure of the colon and (b, c) BMPM in greater omentum. (d) The cysts are connected with colonic serosa
10.3 Pathology
BMPM is a localized tumour arising from mesothelial cells. Pathological evaluation of BMPM shows that the tumour is composed of a multiple mesothelial-lined cystic structure containing thin watery secretions and lined by a single layer of mesothelial-like cells. Immunohistochemical analysis revealed positive expression of mesothelial cells (Fig. 10.7), calretinin (Fig. 10.8).
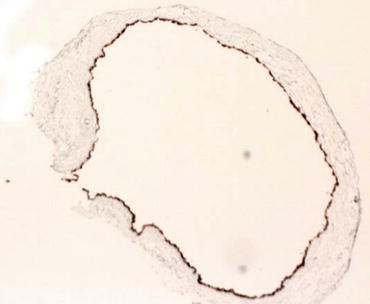
Fig. 10.7
Anti-Ki-67 antibody immunoreaction of cuboidal mesothelial cells lined on the inner surface of cysts (×100)
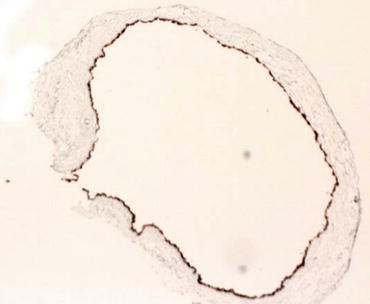
Fig. 10.8
Positive immunoreaction to anti-mesothelin antibody was detected on mesothelial-like cells in inner surface of peritoneal floating cyst (×100)
10.4 Management of BMPM
Surgery remains the mainstay of treatment with complete removal of the cystic lesions to avoid local recurrence even though there are no evidence-based treatment strategies for BMPM. Even the complete removal of the disease, high recurrence rates [15, 16] and malignant transformation [3, 4] have been reported. There is only two series of BMPM treated with aggressive surgery followed by heated intraperitoneal chemotherapy (HIPEC) [17, 18].
In first report, five cases of BMPM, four females and one male, were reviewed by Sethna et al. [17]. All patients were symptomatic, and in one patient prolonged conservative treatment for over 10 years resulted with transformation to the invasiveness with lymph node metastasis. Disease control of both ascites and pain in the abdomino-pelvic region was achieved in all patients treated with cytoreductive surgery with HIPEC. They concluded that BMPM should no longer be referred to as “benign” cystic mesothelioma and an aggressive treatment approach with complete disease eradication is the correct goal of treatment.
In second report, four patient of BMPM were reviewed by Baratti et al. [18]. All patients were symptomatic and recurrent cases. Disease control was achieved in three patients treated with cytoreductive surgery with HIPEC. One patient had a recurrence of BMPM and underwent to second-time cytoreductive surgery and HIPEC. They concluded that complete cytoreduction and HIPEC were more effective in preventing recurrence and transformation to malignancy of BMPM.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree