Benign Tumors of Bone
Cynthia M. Kelly
Musculoskeletal tumors are, in general, uncommon problems, and malignant tumors of bone are considered rare. Comparatively speaking, benign tumors of bone are more commonly seen by orthopaedic surgeons and primary care practitioners. Benign tumors of bone may exhibit various biologic and clinical behaviors that require a broad spectrum of treatment options. Management of these lesions is best handled by an orthopaedic surgeon and, in certain instances, by a fellowship-trained orthopaedic oncologist. Many benign tumors of bone are incidental findings, noted during radiographic evaluation of an extremity for an unrelated complaint such as a sports injury or other trauma. It is important to recognize lesions that are most likely benign processes that can be observed versus those that need to be treated surgically. In rare instances benign lesions have the potential to undergo malignant transformation. It is therefore important for the physician to understand these variations in biological behavior in order to care for patients appropriately.
Pathogenesis
Etiology
Most bone tumors, either benign or malignant, have no identifiable etiology.
Few benign bone lesions are associated with preexisting conditions or have a hereditary or familial pattern.
Pathophysiology
Unknown for most benign tumors of bone and is best described for congenital and inherited syndromes (Table 4.2-1)
Classification
Classification terms for benign bone tumors are based on their biological behavior, tissue of origin, or syndrome names generally associated with polyostotic diseases.
Based on biologic behavior
Stage of the lesion
Latent, active, and aggressive (see Box 4.2-1; see also Chapter 1, Evaluation of Bone Tumors)
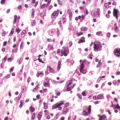
Based on tissue of origin
World Health Organization classifies tumors into general categories based on the type of neoplastic tissue within the lesion (Table 4.2-2).
Other lesions of bone that mimic tumors (Box 4.2-2)
Syndromes associated with polyostotic disease (Table 4.2-3)
Diagnosis
History and Physical Examination
History: including presenting complaint and past medical history
Patients with benign bone lesions generally present with one of four scenarios:
Painless bone mass
Incidental radiographic finding
Painful bone lesion
Pathologic fracture
An important early factor in evaluation of a patient with a benign tumor of bone is: “Is the lesion associated with pain?”
For those with pain, consideration should be given to the patient’s pain complaints and exacerbating activities.
For painless lesions, the history should focus on the means of discovery.
Clinical Features
Painless bone mass
Painless bone masses are usually noted as a bump on the affected bone and may be solitary or multiple.
Most common example: osteochondroma
Incidental radiographic finding
A common scenario is that a patient injures an area, an x-ray is obtained, and an asymptomatic bony lesion is noted. These incidentally identified lesions generally are benign, and important radiographic features to be considered in these situations will be discussed below.
Most common example: nonossifying fibroma (fibrous cortical defect)
Painful bone lesion
When a patient presents with pain as the primary complaint and an underlying tumor of bone is identified, a more thorough evaluation is warranted to rule out an aggressive benign tumor that is associated with structural compromise of the bone or even a malignancy.
Differential diagnosis in this situation may be extensive.
Pathologic fracture
Most children with a pathologic fracture through an underlying benign tumor of bone can be managed conservatively initially to allow for fracture healing, and then a biopsy may be performed in a delayed fashion if appropriate.
Key question in determining whether there is cause for concern: Was pain present preceding the time of the fracture?
Preceding pain: Possible aggressive benign or malignant lesion: may warrant biopsy∼hsurgical intervention
No preceding pain: Very likely a benign, inactive lesion
Common examples: nonossifying fibroma, simple bone cyst
Box 4.2-1 Staging of Benign Bone Lesions*
Stage 1 (latent)
Nonossifying fibroma
Enchondroma
Unicameral bone cyst
Osteochondroma
Osteoid osteoma
Fibrous dysplasia
Eosinophilic granuloma (Langerhans cell histiocytosis)
Stage 2 (active)
Enchondroma
Osteochondroma
Osteoid osteoma
Osteoblastoma
Giant cell tumor
Chondromyxoid fibroma
Fibrous dysplasia
Eosinophilic granuloma (Langerhans cell histiocytosis)
Aneurysmal bone cyst
Unicameral bone cyst
Osteofibrous dysplasia
Juxtacortical chondroma
Chondroblastoma
Stage 3 (aggressive)
Giant cell tumor
Osteoblastoma
Chondroblastoma
Aneurysmal bone cyst
*Many types of benign bone lesions may be classified in more than one stage based on their biologic behavior.
Table 4.2-1 Benign Bone Lesions With Consistent Genetic Defects And/Or Hereditary Or Familial Inheritance Patterns | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Physical Examination
General physical examination
Look for signs of multifocal disease (café-au-lait spots, axillary freckling, multiple bony masses, soft tissue myxomas, soft tissue hemangiomas, short stature, limb deformities), generalized lymphadenopathy.
Examine for possible sites of referred pain.
Focused examination concentrating on the area of concern
Specific findings to assess are the presence of a visible mass, limb length discrepancy, overlying skin changes, increased tactile temperature, presence of a soft tissue mass, tenderness on palpation of the area, compromised joint range of motion, surrounding muscle atrophy, neurovascular status of the limb and any lymphadenopathy.
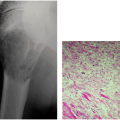
Radiographic Evaluation
X-ray films are a necessary part of the work-up of any patient with a musculoskeletal complaint.
At a minimum, two orthogonal view x-rays of the affected area should be obtained, an AP and a lateral view.
Oblique views may also be of assistance.
Example: avulsive cortical irregularity (periosteal desmoid), which always occurs at the posteromedial distal femoral metaphysis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree