Chapter Outline
Haemoglobinometry 19
Measurement of haemoglobin concentration using a spectrometer (spectrophotometer) or photoelectric colorimeter 19
Haemiglobincyanide (cyanmethaemoglobin) method 20
Diluent 20
Haemiglobincyanide reference standard 20
Method 21
Calculation of haemoglobin concentration 21
Direct spectrometry 22
Direct reading portable haemoglobinometers 22
Range of haemoglobin concentration in health 23
Packed cell volume or microhaematocrit 23
International Council for Standardisation in Haematology reference method 24
Surrogate reference method 24
Range of packed cell volume in health 24
Manual cell counts and red cell indices 24
Range of MCHC in health 25
Manual differential leucocyte count 25
Method 25
Basophil and eosinophil counts 26
Reporting the differential leucocyte count 26
Platelet count 27
Range of platelet count in health 27
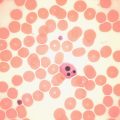
Reticulocyte count 27
Reticulocyte stains and count 27
Fluorescence methods for performing a reticulocyte count 30
Manual reference method 30
Range of reticulocyte count in health 30
Automated blood count techniques 30
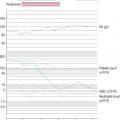
Haemoglobin concentration 31
Red blood cell count 31
Counting systems 31
Reliability of electronic counters 32
Setting discrimination thresholds 33
Packed cell volume and mean cell volume 33
Red cell indices 35
Variations in red cell volumes: red cell distribution width 35
Percentage hypochromic red cells and variation in red cell haemoglobinisation: haemoglobin distribution width 36
White blood cell count 36
Automated differential count 37
The automated immature granulocyte count 38
The automated nucleated red blood cell count 38
Automated digital imaging analysis of blood cells 39
New white cell parameters 39
Automated instrument graphics 40
Platelet count 40
Platelet count in health 40
Mean platelet volume 40
Reticulated platelets and immature platelet fraction 42
Reticulocyte count 42
Immature reticulocyte fraction 42
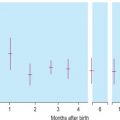
Reticulocyte counts in health 43
Measurement of reticulocyte haemoglobin 43
Point-of-care instruments 43
Calibration of automated blood cell counters 43
Flagging of automated blood counts 44
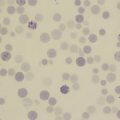
Microscopy 45
It is possible to use manual, semiautomated or automated techniques to determine the various components of the full blood count (FBC). Manual techniques are generally low cost with regard to equipment and reagents but are labour intensive; automated techniques entail high capital costs but permit rapid performance of a large number of blood counts by a smaller number of laboratory workers. Automated techniques are more precise, but their accuracy depends on correct calibration and the use of reagents that are usually specific for the particular analyser. Many laboratories now use automated techniques almost exclusively, but certain manual techniques are necessary as reference methods for standardisation. Manual methods may also be needed to deal with samples that have unusual characteristics that give discrepant results with automated analysers.
All the tests discussed in this chapter can be performed on venous or free-flowing capillary blood that has been anticoagulated with ethylenediaminetetra-acetic acid (EDTA) (see p. 4 ). Thorough mixing of the blood specimen before sampling is essential for accurate test results. Ideally, tests should be performed within 6 h of obtaining the blood specimen because some test results are altered by longer periods of storage. However, results that are sufficiently reliable for clinical purposes can usually be obtained on blood stored for up to 24 h at 4°C.
Haemoglobinometry
The haemoglobin concentration (Hb) of a solution may be estimated by measurement of its colour, by determination of its power of combining with oxygen or carbon monoxide or by analysis of its iron content. The methods to be described are all colour or light-intensity matching techniques, which also measure, to a varying extent, any methaemoglobin (Hi) or sulphaemoglobin (SHb) that may be present. The oxygen-combining capacity of blood is 1.34 ml of O 2 per g of haemoglobin. Ideally, for assessing the clinical consequences of anaemia, a functional estimation of Hb should be carried out by measurement of oxygen capacity, but this is hardly practical in the routine haematology laboratory. It gives results that are at least 2% lower than those given by the other methods, probably because a small proportion of inert pigment is always present. The iron content of haemoglobin can be estimated accurately, but again the method is impractical for routine purposes. Estimations based on iron content are generally taken as authentic, but iron bound to inactive pigment is included. Iron content is converted into haemoglobin by assuming the following relationship: 0.347 g of iron = 100 g of haemoglobin.
Measurement of haemoglobin concentration using a spectrometer (spectrophotometer) or photoelectric colorimeter
Only the haemiglobincyanide (HiCN; cyanmethaemoglobin) method is now in common use. It has the advantage over the oxyhaemoglobin (HbO 2 ) method of there being a stable and reliable reference preparation available. With the exception of several point-of-care instruments, the HbO 2 method is now rarely used. The method is given in the previous edition of this book.
Although the HiCN reagent contains cyanide, there is only 50 mg of potassium cyanide per litre and 600–1000 ml would have to be swallowed to produce serious effects. However, the use of potassium cyanide has been viewed as a potential hazard; alternative less hazardous reagents that have been introduced are sodium azide and sodium lauryl sulphate, , which convert haemoglobin to haemiglobinazide and haemiglobinsulphate, respectively. They are used in some automated systems, but no stable standards are available and they, too, are toxic substances that must be handled with care.
Other methods that have been used include Sahli’s acid–haematin method, which is less accurate because the colour develops slowly, is unstable and begins to fade almost immediately after it reaches its peak. The alkaline–haematin method gives a true estimate of total haemoglobin concentration even if carboxyhaemoglobin (HbCO), Hi or SHb is present; plasma proteins and lipids have little effect on the development of colour, although they cause turbidity. The original method was more cumbersome and less accurate than the HiCN or HbO 2 methods, but a modified method has been developed in which blood is diluted in an alkaline solution with nonionic detergent and read in a spectrometer at an absorbance of 575 nm against a standard solution of chlorohaemin. , One evaluation gave encouraging results, although another study showed a bias of 2.6% compared with the reference method, with nonlinearity in the relationship between haemoglobin concentration and absorbance at high and low haemoglobin concentrations.
Haemiglobincyanide (cyanmethaemoglobin) method
The haemiglobincyanide (cyanmethaemoglobin) method is the internationally recommended method for determining the haemoglobin concentration of blood. In some countries cyanide reagents are no longer available. The basis of the method is dilution of blood in a solution containing potassium cyanide and potassium ferricyanide. Haemoglobin, Hi and HbCO, but not SHb, are converted to HiCN. The absorbance of the solution is then measured in a spectrometer at a wavelength of 540 nm or in a photoelectric colorimeter with a yellow-green filter, such as Ilford 625, Wratten 74 (may be available on www.ebay.co.uk ) or Horiba XF3415, 530QM30 ( www.horiba.com ).
Diluent
The original (Drabkin) reagent had a pH of 8.6. The following modified solution listed in Table 3-1 , Drabkin-type reagent, as recommended by the International Committee (now Council) for Standardisation in Haematology (ICSH), has a pH of 7.0–7.4. It is less likely to cause turbidity from precipitation of plasma proteins and requires a shorter conversion time (3–5 min) than the original Drabkin solution, but it has the disadvantage that the detergent causes some frothing.
| Reagent | Amount |
|---|---|
| Potassium ferricyanide (0.607 mmol/l) | 200 mg |
| Potassium cyanide (0.768 mmol/l) | 50 mg |
| Potassium dihydrogen phosphate (1.029 mmol/l) | 140 mg |
| Nonionic detergent * | 1 ml |
| Distilled or deionised water | To 1 litre |
* Suitable nonionic detergents include Nonidet P40 substitute (Sigma–Aldrich; www.sigmaaldrich.com , Roche Diagnostics; http://lifescience.roche.com and other suppliers) or Triton X-100 (Sigma–Aldrich).
The pH must be checked with a pH meter at least once a month. The diluent should be clear and pale yellow. When measured against water as a blank in a spectrometer at a wavelength of 540 nm, the absorbance must be zero. If stored at room temperature in a brown borosilicate glass bottle, the solution keeps for several months. If the ambient temperature is higher than 30°C, the solution should be stored in the refrigerator but brought to room temperature before use. It must not be allowed to freeze. The reagent must be discarded if it becomes turbid, if the pH is found to be outside the 7.0–7.4 range or if it has an absorbance other than zero at 540 nm against a water blank.
Haemiglobincyanide reference standard
With the advent of HiCN solution, which is stable for many years, other standards have become outmoded. The ICSH has defined specifications on the basis of a relative molecular mass (molecular weight) of human haemoglobin of 64 458 (i.e. 16 114 as the monomer) and a millimolar area absorbance (extinction coefficient) of 11.0 (that is, the absorbance at 540 nm of a solution containing 55.8 mg of haemoglobin iron per litre).
Some standards are prepared from ox blood, which has the same extinction coefficient but a molecular weight of 64 532 (16 133 as the monomer). These specifications have been widely adopted; a World Health Organisation (WHO) International Standard has been established and a comparable reference material is available from the ICSH ( www.eurotrol.com ). A new lot of the haemoglobincyanide or haemoglobin standard was released in 2008. This replaces the previous lot and was produced using the same methodology previously specified by ICSH. The current standard has an assigned concentration value of 574.2 (± 5.1) mg/l or 35.63 (± 0.32) μmol/l; the exact concentration is indicated on the label. The stability expectation of this standard is 15 years but it will continue to be monitored on a twice-yearly basis over the lifetime of the lot. The haemoglobin standard provides a reference material from which both laboratory-based cell counters and point-of-care instruments calibrate their haemoglobin methods.
The HiCN solution is dispensed in 10 ml sealed ampoules and is regarded as a dilution of whole blood. The original Hb that it represents is obtained by multiplying the figure stated on the label by the dilution to be applied to the blood sample. Thus, if the standard solution contains 800 mg (0.8 g) of haemoglobin per litre, it will have the same optical density as a blood sample containing 160 g/l of haemoglobin if diluted 1 to 200 or as one containing 200 g/l of haemoglobin if diluted 1 to 250. Within the Système International d’Unités (SI), Hb may be expressed as mass concentration as g/l (or g/dl) or in terms of substance concentration as μmol/l = g/l × 0.062. For clinical purposes, there are practical advantages in expressing Hb in mass concentration per litre or per decilitre (dl) and this is our recommendation.
The HiCN reference preparation is intended primarily for direct comparison with blood that is converted to HiCN.
Method
Make a 1 in 201 dilution of blood by adding 20 μl of blood to 4 ml of diluent. Stopper the tube containing the solution and invert it several times. Let the test sample stand at room temperature for at least 5 min (to ensure the complete conversion of haemoglobin to haemiglobincyanide) and then pour it into a cuvette and read the absorbance in a spectrometer at 540 nm or in a photoelectric colorimeter with a suitable filter (see above) against a reagent blank. The absorbance of the test sample must be measured within 6 h of its initial dilution. The absorbance of a commercially available HiCN standard (brought to room temperature if previously stored in a refrigerator) should also be compared with that of a reagent blank in the same spectrometer or photoelectric colorimeter as was used for the patient sample. The standard should be kept in the dark and, to ensure that contamination is avoided, any unused solution should be discarded at the end of the day on which the ampoule is opened.
Calculation of haemoglobin concentration
Hb g / l = ∗ A 540 of test sample A 540 of standard × Conc . of standard × Dilution factor 201 † 1000
Preparation of standard graph and standard table
When many blood samples are to be tested, it is convenient to read the results from a standard graph or table relating absorbance readings to Hb in g/l for the specific instrument. This graph should be prepared each time a new photometer is put into use or when a bulb or other component is replaced. It can be prepared as follows.
Prepare five dilutions of the HiCN reference standard (or equivalent preparation) (brought to room temperature) with the cyanide–ferricyanide reagent according to Table 3-2 . Because the graph will be used to determine the haemoglobin measurements, it is essential that the dilutions are performed accurately.
| Tube | Haemoglobin * (%) | HiCN Volume (ml) | Reagent Volume (ml) |
|---|---|---|---|
| 1 | 100 (full strength) | 4.0 (neat) | None |
| 2 | 75 | 3.0 | 1.0 |
| 3 | 50 | 2.0 | 2.0 |
| 4 | 25 | 1.0 | 3.0 |
| 5 | 0 | None | 4.0 (neat) |
The haemoglobin concentration of the reference preparation in each tube should be plotted against the absorbance measurement. For example, if the label on the reference preparation states that it contains 800 mg/l (i.e. 0.8 g/l) and the method for haemoglobin measurement uses a dilution of 1:201, the respective haemoglobin concentrations of tubes 1–5 would be 160, 120, 80, 40 and 0 g/l.
Using linear graph paper, plot the absorbance values (formerly called optical density) on the vertical axis and the haemoglobin values on the horizontal axis. In some instruments, measurements are read as percentage transmittance; in this case, use semilogarithmic paper with the transmittance recorded on the vertical or log scale. The points should fit a straight line that passes through the origin. Providing that the standard has been correctly diluted, this provides a check that the calibration of the photometer is linear. From the graph, it is possible to construct a table of readings and corresponding haemoglobin concentration values. This is more convenient than reading values from a graph when large numbers of measurements are made. It is important that the performance of the instrument does not vary and that its calibration remains constant in relation to haemoglobin measurements. To ensure this, the reference preparation should be measured at frequent intervals, preferably with each batch of blood samples.
The main advantages of the HiCN method for haemoglobin determination are that it allows direct comparison with the reference standard and that the readings need not be made immediately after dilution so batching of samples is possible. It also has the advantage that all forms of haemoglobin, except SHb, are readily converted to HiCN.
The rate of conversion of blood containing HbCO is markedly slow. This difficulty can be overcome by prolonging the reaction time to 30 min before reading the results. The difference between the 5 and 30 min readings can be used as a semiquantitative method for estimating the percentage of HbCO in the blood.
As referred to earlier, lauryl sulphate or sodium azide can be used as nonhazardous substitutes for potassium cyanide. However, no stable standards are available for these methods so a sample of blood that has first had a haemoglobin value assigned by the HiCN method needs to be used as a secondary standard.
Abnormal plasma proteins or a high leucocyte count may result in turbidity when the blood is diluted in the Drabkin-type reagent. The turbidity can be avoided by centrifuging the diluted sample or by increasing the concentration of potassium dihydrogen phosphate to 33 mmol/l (4.0 g/l).
Direct spectrometry
The haemoglobin concentration of a diluted blood sample can be determined by spectrometry without the need for a standard, provided that the spectrometer has been correctly calibrated. The blood is diluted 1:201 (or 1:251) with cyanide–ferricyanide reagent (see p. 20 ) and the absorbance is measured at 540 nm. Haemoglobin concentration is calculated as follows:
Hb g / l = A 540 HiCN × 16 114 × Dilution factor 11.0 × d × 1000 or Hb μ mol / l = A 540 HiCN × Dilution factor 110 × d × 1000
When assigning a value to a haemoglobin solution that may be used as a reference preparation, it is necessary first to calibrate the spectrometer. This requires checking wavelength with a holmium oxide filter, absorbance with a set of calibrated neutral density filters and stray light with a neutral density filter at 220 nm (National Physical Laboratory, Teddington, UK, www.npl.co.uk ). Matched optical or quartz glass cuvettes with a transmission difference of < 1% at 200 nm should be used. Subsequently, the calibration of the spectrophotometer can be checked by verifying that it gives an accurate reading of the HiCN standard. Slight deviations from the expected A 540 HiCN value for the standard may be used to correct the results of test samples for a bias in measurement.
Direct reading portable haemoglobinometers
Colour comparators
These are simple clinical devices that compare the colour of blood against a range of colours representing haemoglobin concentrations. They are intended for anaemia screening in the absence of laboratory facilities and are described in Chapter 26 .
Portable haemoglobinometers
Portable haemoglobinometers have a built-in filter and a scale calibrated for direct reading of Hb in g/l or g/dl. They are generally based on the HbO 2 method. A number of instruments are now available that use a light-emitting diode of appropriate wavelength; they are standardised to give the same results as with the HiCN method.
The HemoCue system ( www.radiometer.co.uk/en-gb/products/hemocue ) is a well-established method for haemoglobinometry. It consists of a precalibrated, portable, battery-operated spectrometer; no dilution is necessary because blood is run by capillary action directly into a cuvette containing sodium nitrite and sodium azide, which convert the haemoglobin to azidemethaemoglobin. The absorbance is measured at wavelengths of 565 and 880 nm. Measurements are not affected by high levels of bilirubin, lipids or white cells and the HemoCue system is sufficiently reliable for use as a laboratory instrument; it is easy for nontechnical personnel to operate and is thus also suitable for use at point-of-care sites. The cuvettes must be stored in a container with a drying agent and kept within the temperature range of 15 to 30°C. Some devices are now available that use reagent-free cuvettes that will not deteriorate in adverse climatic conditions. The manufacturers of HemoCue have also released a portable system that measures both Hb and the white blood cell count (WBC), the HemoCue WBC.
Chempaq (Chempaq A/s, Farum, Denmark; http://chempaq-dk.business1.com/ ) produces two different portable multiplatform haematology analysers that use impedance cell counting and measurement of Hb by a spectrophotometric method on 20 μl of blood. The Chempaq XBC uses a disposable cartridge to measure three different test profiles, Hb alone or WBC, with three-part differential, plus Hb or Hb with red blood cell count (RBC), haematocrit (Hct), mean cell volume (MCV), mean cell haemoglobin (MCH) and mean cell haemoglobin concentration (MCHC). The Chempaq XDM701 uses the same principles but also reports a platelet count.
The DiaSpect Haemoglobinometry system ( www.diaspect.eu ) measures Hb in unaltered whole blood in a special plastic cuvette that also serves as the sampling device. The instrument is a portable spectrophotometer powered by 3.6 V integrated lithium-ion rechargeable batteries or by a 100–240 V adaptor. Because the cuvettes do not contain any reagents, they are not affected by temperature or humidity and no special storage conditions are required. They have a shelf life of at least 2 years. Haemoglobin fractions are measured from absorbance wavelengths between 400 and 800 nm. A patented method eliminates the impact of scattering from the blood cells while possible background turbidity from interfering substances is measured and compensated for at high wavelength. The results are displayed in < 5 s. An accuracy within ± 3 g/l for measurements between 10 and 200 g/l has been shown.
Noninvasive screening tests
Methods have been developed for using near-infrared spectroscopy at body sites, mainly a finger, to identify the spectral pattern of haemoglobin in an underlying blood vessel and derive a measurement of Hb. Several studies have shown an approximate correlation with blood haemoglobinometry. ,
Range of haemoglobin concentration in health
See Chapter 2, Tables 2-1 , 2-2 and 2-3 , for ranges for Hb in health. It should be noted that there are gender differences, diurnal variations and environmental and physiological factors that must also be taken into account.
Packed cell volume or microhaematocrit
The packed cell volume (PCV) can be used as a simple screening test for anaemia, as a reference method for calibrating automated blood count systems and as a rough guide to the accuracy of Hb measurements. The PCV × 1000 is about three times the Hb expressed in g/l (e.g. 0.36 × 1000 is approximately 120 × 3). In conjunction with estimations of Hb and RBC, PCV can be used in the calculation of red cell indices. However, its use in under-resourced laboratories may be limited by the need for a specialised centrifuge and a reliable supply of capillary tubes.
The microhaematocrit method for determining the PCV is carried out on blood contained in capillary tubes 75 mm in length and having an internal diameter of about 1 mm. The tubes may be plain for use with anticoagulated blood samples or coated inside with 1 international unit (iu) of heparin for the direct collection of capillary blood. The centrifuge used for the capillary tubes provides a centrifugal force of circa (c.) 12 000 g and 5 min centrifugation results in a constant PCV. When the PCV is > 0.5, it may be necessary to centrifuge for a further 5 min.
Allow blood from a well-mixed specimen, or from a free flow of blood by skin puncture, to enter the tube by capillarity, leaving at least 15 mm unfilled. Then seal the tube by a plastic seal (e.g. Cristaseal, Hawksley, Lancing, Sussex; www.hawksley.co.uk ). Sealing the tube by heating is not recommended because the seals tend to be tapered and there is the likelihood of lysis. After centrifugation for 5 min, measure the proportion of cells to the whole column (i.e. the PCV) using a reading device.
Accuracy of microhaematocrit
The microhaematocrit method has an adequate level of accuracy and precision for clinical utility. However, attention must be paid to a number of factors that may produce an inaccurate result.
Anticoagulant
K 2 -EDTA is recommended, because K 3 -EDTA causes shrinking of the red cells, reducing the PCV by about 2%. Anticoagulant concentration in excess of 2.2 mg/ml may also cause a falsely low PCV as a result of cell shrinkage.
Blood sample
Because the PCV gradually increases with storage, the test should be performed within 6 h of collecting the blood sample, but a delay of up to 24 h is acceptable if the blood is kept at 4°C.
Failure to mix the blood sample adequately will produce an inaccurate result. The degree of oxygenation of the blood also affects the result because the PCV of venous blood is ≈ 2% higher than that of fully aerated blood (which has lost CO 2 and taken up O 2 ). To ensure adequate oxygenation and sample mixing, the free air space above the sample should be > 20% of the container volume.
Capillary tubes
Variation of the bore of the tubes may cause serious errors if they are not within the narrow limits of defined specifications that should be met by manufacturers: length 75 ± 0.5 mm; internal diameter 1.07–1.25 mm; wall thickness 0.18–0.23 mm; and bore taper not exceeding 2% of the internal diameter over the entire length of the tube.
Centrifuge
Centrifuges should be checked at intervals (at least annually) by a tachometer for speed and by a stopwatch for timer accuracy. Efficiency of packing should also be tested by centrifuging samples of normal and polycythaemic blood for varying times from 5 to 10 min to determine the minimum time for complete packing of the red cells.
Reading
The test should be read as soon as possible after centrifugation because the red cells begin to swell and the interface becomes progressively more indistinct. To avoid errors in reading with the special reading device, a magnifying glass should be used. White cells and platelets (the buffy coat) must be excluded as far as possible from the reading of the PCV. If a special reading device is not available, the ratio of red cell column to whole column can be calculated from measurements obtained by placing the tube against arithmetic graph paper or against a ruler.
Plasma trapping
The amount of plasma trapped between red cells, especially in the lower end of the red cell column, and red cell dehydration during centrifugation generally counterbalance each other and the error caused by trapped plasma is usually not more than 0.01 PCV units. Thus, in routine practice, it is unnecessary to correct for trapped plasma, but if the PCV is required for calibrating a blood cell analyser or for calculating blood volume, the observed PCV should be reduced by a 2% correction factor after it has been centrifuged for 5 min or for 10 min with polycythaemic blood. It is, however, preferable to use the surrogate reference method. Plasma trapping is increased in macrocytic anaemias, spherocytosis, thalassaemia, hypochromic anaemias and sickle cell anaemia; it may be as high as 20% in sickle cell anaemia if all the cells are sickled.
International Council for Standardisation in Haematology reference method
Haemoglobin concentration is measured by the routine method on blood specimens with a range of Hb samples. Samples of the same specimens are then taken into special borosilicate glass capillary tubes, which are centrifuged for 5 min or longer to achieve full red cell packing. The tubes are then broken at the midpoint of the packed red cells, blood is extracted with a micropipette and its haemoglobin concentration is measured. PCV is calculated as the ratio of the Hb of whole blood to that of the packed cells. This method is appropriate for instrument and reagent manufacturers, but it is time-consuming, is potentially unsafe and requires significant expertise, which makes it impractical for occasional use in routine laboratories. Accordingly, the International Council for Standardisation in Haematology has developed a ‘surrogate reference method’.
Surrogate reference method
Equipment
- •
Standard microhaematocrit centrifuge
- •
Borosilicate glass capillary tubes with the following specifications: length 75 ± 0.5 mm; inner diameter 1.55 ± 0.085 mm; outer diameter 1.9 ± 0.085 mm (Drummond Scientific, Broomall, PA 19008: Catalogue #1–000–751C; www.drummondsci.com )
- •
Capillary tube holder consisting of a 75 × 25 mm glass slide mounted on a 75 × 50 mm slide
- •
Microscope fitted with a vernier scale and ocular crossbar
Method
- 1.
Take up duplicate samples of well-mixed blood into the specified capillary tubes and centrifuge as described on page 23.
- 2.
Promptly remove the tubes from the centrifuge, position each in turn against the edge of the 25 mm slide and place this on the stage of the microscope.
- 3.
Ensure that the capillary tube is aligned in a true horizontal position relative to the field of view and, using low power, note on the vernier scale the lengths of the tube at the interfaces of (a) red cells and seal, (b) red cells and leucocytes and (c) plasma and air.
- 4.
Calculate the spun PCV = ( b − a )/( c − a ). Determine the acceptability of paired measurements – duplicates must agree within 0.007 units; if they do not, the paired tests must be repeated.
- 5.
Calculate the surrogate reference PCV from the formula:
<SPAN role=presentation tabIndex=0 id=MathJax-Element-3-Frame class=MathJax style="POSITION: relative" data-mathml='SpunPCV−0.011.90.9736′>SpunPCV−0.011.90.9736SpunPCV−0.011.90.9736
Spun PCV − 0.011.9 0.9736
This formula applies only to the specified capillary tubes; other tubes require specific validation by the ICSH reference method so that an appropriate formula can be derived. If the surrogate reference measurements are to be used to validate equipment or methods, a minimum of six different blood samples are required, at least two in each of the ranges of PCV 0.20–0.25, 0.40–0.45 and 0.60–0.65. If necessary, the PCV of normal samples may be adjusted by the appropriate addition or removal of autologous plasma.
Range of packed cell volume in health
See Chapter 2, Tables 2-1 , 2-2 and 2-3 .
Manual cell counts and red cell indices
The principles of manual cell counts, the use of the haemocytometer counting chamber for manually counting white cells and platelets and the limitations of these measurements are described in Chapter 26 .
An accurate RBC enables the MCV and MCH to be calculated. In most laboratories, where these indices are provided by an automated system (see p. 35 ), they are of considerable clinical importance and are widely used in the classification of anaemia. Where automated analysers are not used, manual RBCs (and consequently, calculations of these red cell indices) are so imprecise and time-consuming that they have become obsolete.
The only measurement that can be obtained with reasonable accuracy by manual methods is MCHC because this is derived from Hb and PCV from the following formula:
MCHC g/ l = Hb g/ l ÷ PCV l / l .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree