APPLICATIONS, TECHNIQUES, AND INTERPRETATION OF RADIONUCLIDE IMAGING
Part of “CHAPTER 34 – THYROID UPTAKE AND IMAGING“
APPLICATIONS OF IMAGING
Imaging is of value in distinguishing Graves disease from toxic nodular goiter, assessing the function of nodules, differentiating subacute thyroiditis and related conditions from Graves disease and toxic nodular goiter, defining occult thyroid lesions, determining the location and size of functional thyroid tissue, and detecting metastases from differentiated thyroid cancer. Perhaps the most frequent application of thyroid imaging is in evaluating the function of palpable nodules. A nodule is a palpatory or pathologic finding and cannot be defined by thyroid imaging alone. The imaging of palpable nodules allows normally functioning tissue to be distinguished from hypofunctioning (“cold”) or hyperfunctioning (“hot”) lesions. Hyperfunctional nodules (Fig. 34-1) may be associated with clinical or subclinical hyperthyroidism and are unlikely to be cancer. Hypofunctional nodules may be associated with a higher incidence of malignancy (see Chap. 39 and Chap. 40).
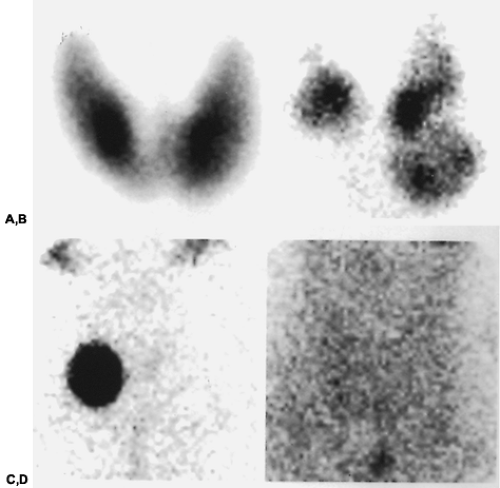 FIGURE 34-1. Typical images in (A) Graves disease; (B) toxic multinodular goiter; (C) solitary hyperfunctioning nodule; (D) destructive thyroiditis. |
Imaging with or without an uptake measurement may help differentiate hyperthyroidism due to thyroiditis (viral, postpartum, or amiodarone related), from hyperthyroidism due to Graves disease or nodular goiter (see Fig. 34-1).
Occult or nonpalpable thyroid lesions may be a clinical consideration in some patients without known primary tumors and in patients exposed to therapeutic x-rays or other radiation in infancy and childhood, who are at risk of developing a thyroid neoplasm later in life.22,23
Thyroid size generally is estimated by palpation or by ultra-sonography. Size also may be assessed scintigraphically, using a rectilinear scanner that provides a full-sized 1:1 image.24 Estimates of the size of the thyroid gland or thyroid nodule are usually used to calculate the amount of therapeutic radioiodine to be administered in hyperthyroidism and to assess the response to radioiodine or suppressive therapy. The use of ultrasonography to measure thyroid volume is discussed in Chapter 35.
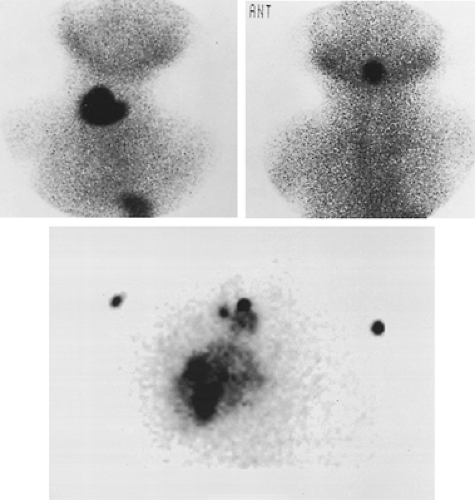
Imaging may help establish the presence of a nonpalpable thyroid gland, for instance in hypothyroid infants, and may help localize mediastinal, lingual, or other ectopic thyroid tissue25,26 (Fig. 34-2). Mediastinal imaging is useful to locate aberrant thyroid tissue that might manifest as a substernal mass on a chest radiograph, often with tracheal deviation.
Whole body radioiodine imaging, together with serum thyroglobulin determinations, is used to identify, locate, and monitor differentiated thyroid cancer (see Chap. 40).
TECHNIQUES OF IMAGING
IMAGING OF THE THYROID GLAND
The radiopharmaceuticals of choice are 123I and 99mTc pertechnetate. For mediastinal thyroid tissue, 123I imaging at 24 hours may have advantages over 99mTc imaging because activity in the heart blood pool on the 99mTc image may preclude optimal visualization of overlying thyroid tissue. Imaging with 99mTc, however, may suffice for most goiters with substernal extensions and, hence, can be used for the initial evaluation. 131I may be used in lieu of 123I, if the latter is not available. 131I offers the same advantage as 123I, and its more energetic gamma rays are less likely to be absorbed by the overlying sternum.
123I has theoretical advantages over 99mTc for the evaluation of lingual thyroid tissue because of the absence of significant 123I accumulation in the salivary glands, which may interfere with interpretation (the salivary glands trap but do not bind
99mTc or iodine, so only early imaging, as with 99mTc, shows accumulation of radioactivity). Nonetheless, 99mTc has been used successfully in assessing ectopic thyroid tissue.26
99mTc or iodine, so only early imaging, as with 99mTc, shows accumulation of radioactivity). Nonetheless, 99mTc has been used successfully in assessing ectopic thyroid tissue.26
Imaging is performed 4 or 24 hours after the administration of 0.3 to 0.4 mCi of 123I orally, or 24 hours after the oral ingestion of 0.03 to 0.05 mCi of 131I, or 20 to 30 minutes after the intravenous injection of ˜5 mCi of 99mTc pertechnetate. Standard imaging projections are anterior, left anterior oblique, and right anterior oblique.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree