Antimicrobial Stewardship: Programmatic Efforts to Optimize Antimicrobial Use
Robert C. Owens Jr.
William R. Jarvis
INTRODUCTION
Microbes account for 90% of the 1014 cells in the human body (1). Thus, it should not be surprising that the well-known benefits of antimicrobials must be balanced with an appreciation of their unintended effects on beneficial microbiota and the evolution of resistance. In essence, use of antimicrobials is a double-edged sword. Their life-saving benefits and disease-modifying effects can be nothing short of miraculous; however, the opposing edge of the sword can be just as sharp. Examples include serious patient harm in the form of adverse drug events (e.g., hepatotoxicity, torsades de pointes, anaphylaxis, renal failure), development of potentially life-threatening Clostridium difficile-associated disease (CDAD), and the emergence of antimicrobial resistance (2,3). While the first two can occur during therapy and are more tangible to the practicing clinician, the emergence of resistance often occurs late and may be less obvious.
It has been said that those who move forward without taking a moment to look back are doomed to repeat history. In 1956, noted microbiologist Ernest Jawetz once wrote:
On the whole, the position of antimicrobial agents in medical therapy is highly satisfactory. The majority of bacterial infections can be cured simply, effectively, and cheaply. The mortality and morbidity from bacterial diseases has fallen so low that they are no longer among the important unsolved problems of medicine. These accomplishments are widely known and appreciated (4).
He goes on to state the intentions of his paper: “the author wishes to call attention to the abuse of antibiotics, its causes and results…” (4). In the current antimicrobial era, some 50-plus years after these initially optimistic observations were made, an increasing number of infections are not easily treated, morbidity and mortality are appreciable, and many infectious diseases have become unsolved problems of modern medicine. The theme of Jawetz’s latter plea remains a challenge facing many infectious disease experts today, calling attention to the abuse of antimicrobials and its causes and results.
In fact, published data note that many prescribers today still do not fully value the importance of preserving these therapeutic resources. Twenty-five million pounds of antimicrobials are produced yearly for human consumption and are administered to 30% to 50% of hospitalized patients, with nonhospitalized Americans receiving 160 million courses (5). Yet, data show that as much as 50% of all antimicrobial use is inappropriate. Stewarding these precious resources has become a priority for many organizations, including the Infectious Diseases Society of America (IDSA), the Society of Healthcare Epidemiology of America (SHEA), the Society of Infectious Diseases Pharmacists, the Alliance for the Prudent Use of Antimicrobials, the Centers for Disease Control and Prevention (CDC), and the World Health Organization. In fact, joint guidelines endorsed by multiple societies have recently been published that reiterate the need for proactive, programmatic efforts to optimize the use of antimicrobials in healthcare settings (6).
Since the initial work of Finland and McGowan, a variety of interventional strategies has been shown to reduce unnecessary antimicrobial use, to optimize the dose and duration, and to minimize the collateral adverse effects of their use (7,8,9). Most studies have evaluated the impact of interventions on inpatient antimicrobial use and, to a lesser degree, outpatient antimicrobial use. This chapter shall reinforce why the judicious use of antimicrobials is essential and the implementation (including potential barriers) of an institutional approach is necessary to optimizing antimicrobial use. It shall also discuss the collaborative nature of these programs with infection control and prevention programs and the microbiology laboratory.
RATIONALE FOR OPTIMIZING ANTIMICROBIAL USE
ANTIMICROBIAL RESISTANCE
Optimizing antimicrobial use through appropriate selection, dosing, and duration can be viewed as a strategy to minimize the development of resistance among clinically important pathogens (10). Factors promoting resistance are complex, numerous, and extend beyond the use of antimicrobial agents in humans; as such, it is not surprising that they do not allow for a prompt resolution (11). Although antimicrobial resistance has been present on this earth since the days of the primordial soup, its practical onset began in the 1920s with the observation that Pfeiffer’s bacillus (now Haemophilus influenzae) showed a natural resistance to penicillin before its introduction for human use (12). With the introduction of Gerhard Domagk’s sulfa drugs in the 1930s, strains of Neisseria gonorrhea and Streptococcus pneumoniae were noted to have developed the so-called “insensitivity” (12). Observations from the laboratory moved to the clinic in the 1940s shortly after the introduction
of penicillin for the treatment of human infections. The miracle drug, penicillin, while initially effective for the treatment of Staphylococcus aureus bloodstream infection (BSI), began to fail to treat infections caused by penicillinase-elaborating strains as reported in Time magazine on May 15, 1944.
of penicillin for the treatment of human infections. The miracle drug, penicillin, while initially effective for the treatment of Staphylococcus aureus bloodstream infection (BSI), began to fail to treat infections caused by penicillinase-elaborating strains as reported in Time magazine on May 15, 1944.
Important to this discussion is the fact that studies have established a strong relationship between antimicrobial use and resistance. Levy et al. developed a biologic model that showed a clear relationship between antimicrobial use and the selection of resistance in humans (13). Additionally, supportive data can be gleaned from in vitro investigations, ecologic studies correlating drug exposure with resistance, controlled trials in which patients with previous use of antimicrobials were more likely to be colonized or infected with resistant bacteria, or prospective studies in which antimicrobial use was associated with the development of resistant flora (13,14,15). With many pharmaceutical companies no longer supporting anti-infective development and fewer new chemical entities being identified, we, now more than ever, should be concerned about the consequences of antimicrobial resistance (16).
Data from surveillance studies demonstrate that for community-acquired respiratory pathogens, resistance among S. pneumoniae or H. influenzae can be an obstacle in selecting and dosing the ideal regimen (17,18). For healthcare-associated infections (HAIs), resistance is an important impediment to treating patients with the correct antimicrobial and dose in a timely fashion. The effects of selecting the wrong antimicrobial and at the incorrect dose have measurable effects on patient outcomes as highlighted by several recent studies (19,20). Thus, an important value provided by a programmatic approach dedicated to the oversight of antimicrobial use and employed by the healthcare system is to “quarterback” and operationalize efforts to maximize the benefits of antimicrobials. Antimicrobial stewardship programs (ASPs) are able to drive the multidisciplinary development of locally customized disease- or pathogen-based guidelines, protocols, and order sets and to provide real-time human and, where available, computerized decision support in addition to their day-to-day interventions.
PATIENT SAFETY
Whether being used appropriately or inappropriately, antimicrobials have the potential for causing serious harm to patients. For example, macrolides, ketolides, or fluoroquinolones are associated with QT interval prolongation; macrolides or ketolides are associated with metabolic liability in the form of cytochrome P450 3A4 inhibition; trimethoprim-sulfamethoxazole is associated with Stevens-Johnson syndrome; and ß-lactams are best known for hypersensitivity reactions (3,21,22) while all antimicrobials are associated with CDAD (23). Disturbingly, the rate and severity of CDAD is increasing and our traditional treatment options appear to be less effective (24,25). The potential harm caused by antimicrobials should incentivize even the most temerarious clinicians not to casually prescribe antimicrobials in the setting of a nonbacterial infection or to stop therapy in a timely manner and carefully monitor patients off antimicrobials (2). In addition, antimicrobials are unique and unlike any other drug class. One can develop an infection because of a resistant pathogen without ever having received the particular antimicrobial it is resistant to; hence, antimicrobials are considered societal drugs because their use has societal consequences (26).
PROGRAMS TO OPTIMIZE ANTIMICROBIAL USE
HOSPITAL-BASED ASPS
A variety of studies has evaluated the impact of interventions on antimicrobial use in healthcare systems. These studies have been conducted using a wide range of resources, methodologies, interventions (often multiple), and outcome measures (usually considering cost, antimicrobial consumption, patient safety, and less frequently resistance). The culmination of these studies was considered and led to a guidance document developed jointly by IDSA and SHEA to provide the framework for developing, implementing, and monitoring the impact of ASPs (6).
IDSA/SHEA GUIDELINES FOR DEVELOPING AN INSTITUTIONAL PROGRAM TO ENHANCE ANTIMICROBIAL STEWARDSHIP
An effective ASP is financially self-supporting and is aligned with patient safety goals (8,27,28,29,30,31,32,33). For these reasons, there should be no excuse for an institution not to have a formal program dedicated to improving the quality of antimicrobial use. Realizing that institutions vary in size and type of specialty services offered, the ASP should be customized accordingly.
INTERVENTIONAL STRATEGY
Two major interventional styles have evolved over recent years. The first is prospective audit and feedback (“back-end” program). This entails obtaining a daily (or every other day for smaller hospitals) list of patients receiving antimicrobials and determining interventions, such as pharmacodynamic dosage adjustment, streamlining the de-escalation and identification of redundant therapy based on culture and susceptibility results, parenteral-to-oral conversions, drug-interaction identification, guideline/protocol compliance, and recommendation of more cost-effective treatments (Figure 14.1). Recommendations are provided to the prescriber in either written form or by direct conversation. Written forms of communication usually take place on nonpermanent forms placed in the patient’s medical record that are removed at discharge. This allows flexibility in what can be written and allows the ASP team member to communicate educational messages effectively and to provide citations or references on why the intervention is being recommended. The benefits of this type of program are its customizability to smaller- (29) or larger-size healthcare facilities (9,27); it avoids taking away the prescriber’s autonomy, which also increases productive “educational” dialogue; and it circumvents the potential for delays in initiating timely antimicrobial therapy since the antimicrobial is already prescribed. The downside is that recommendations are optional (although there are ways to correct repeated unaccepted recommendations by communicating with either the department chief or an institutional committee [e.g., medical executive committee, pharmacy and therapeutics committee, patient safety committee]). A program at Maine Medical Center (MMC) has employed this primary strategy for >5 years (8,27,33), and others have operated for longer periods of time (28).
The second chief strategy is a preauthorization or “front-end” program that restricts most antimicrobials to an approval process. A team member carries a pager or telephone and receives
approval requests for restricted antimicrobials. At the time of interaction, the antimicrobial either is justified and approved or an alternative recommendation is given. The University of Pennsylvania (34,35), The University of Pittsburgh (36), and others (37) have used preauthorization as their primary strategy for several years. The benefits of this strategy include the ability to funnel all initial antimicrobial prescribing through experts versed in antimicrobial therapy and the typical demonstration of these programs for immediate and significant cost savings. The potential downsides to this strategy include the loss of prescriptive autonomy that may lead to “gaming the system” (38) and the fostering of potentially adversarial relationships (if not properly implemented with buy-in from important and opinionated prescribers), the potential for delaying initial therapy, time- and resource-intensive plans (usually 7 days per week with contingency plans for night coverage), and the necessity to make decisions when the least amount of information is known about the actual infection (culture and antimicrobial susceptibility results are not available for 2 to 3 days, and the quality of information relayed to the ASP team member by prescriber can be variable (39)).
approval requests for restricted antimicrobials. At the time of interaction, the antimicrobial either is justified and approved or an alternative recommendation is given. The University of Pennsylvania (34,35), The University of Pittsburgh (36), and others (37) have used preauthorization as their primary strategy for several years. The benefits of this strategy include the ability to funnel all initial antimicrobial prescribing through experts versed in antimicrobial therapy and the typical demonstration of these programs for immediate and significant cost savings. The potential downsides to this strategy include the loss of prescriptive autonomy that may lead to “gaming the system” (38) and the fostering of potentially adversarial relationships (if not properly implemented with buy-in from important and opinionated prescribers), the potential for delaying initial therapy, time- and resource-intensive plans (usually 7 days per week with contingency plans for night coverage), and the necessity to make decisions when the least amount of information is known about the actual infection (culture and antimicrobial susceptibility results are not available for 2 to 3 days, and the quality of information relayed to the ASP team member by prescriber can be variable (39)).
In reality, although ASPs may lean toward one of the two primary strategies, overlap often exists. For example, the program at MMC, while relying primarily on prospective audit and feedback, does incorporate a limited number of antimicrobials that require approval (8). One of the most valuable aspects of an ASP is the institution-wide responsibility for overseeing the use of antimicrobials. Although in moderate-size or larger hospitals an infectious diseases (ID) physician consultation service, ID pharmacist, and infection control department often are present and coexist or collaborate on specific areas of interest, responsibility at the institutional level for antimicrobial stewardship is usually not assigned. An administratively supported ASP aligns resources from these various specialties and assigns responsibility to them.
TEAM MEMBERS
The IDSA/SHEA guidelines for developing an institutional program to enhance antimicrobial stewardship are very clear about the following: the ASP is directed or codirected by the two core team members, an ID physician and an ID-trained pharmacist, both receiving remuneration for their time. The pharmacist should have formal training in ID or be knowledgeable in the appropriate use of antimicrobials, with training being made available to maintain competency. Other team members optimally include a dedicated computer information support specialist, microbiologist, and an infection preventionist/hospital epidemiologist. Figure 14.2 illustrates an optimal schematic for collaboration and partnership that MMC uses and was adapted
from previous models (40). Administrative and committee support (e.g., pharmacy and therapeutics committee) is critical. The particular interventional philosophy, responsibilities, remuneration, and reporting measures should be discussed in advance of implementation to address expectations and resources. Effective communication between the ASP, administration, and an appropriate committee should be maintained to facilitate dialogue over time as the healthcare environment continues to change.
from previous models (40). Administrative and committee support (e.g., pharmacy and therapeutics committee) is critical. The particular interventional philosophy, responsibilities, remuneration, and reporting measures should be discussed in advance of implementation to address expectations and resources. Effective communication between the ASP, administration, and an appropriate committee should be maintained to facilitate dialogue over time as the healthcare environment continues to change.
PROSPECTIVE AUDIT AND FEEDBACK AND PREAUTHORIZATION STUDIES
PROSPECTIVE AUDIT AND FEEDBACK STRATEGY
Fraser et al. (27) designed a prospective randomized controlled study of interventions for targeted antimicrobials in hospitalized patients. The team included a part-time ID physician and a PharmD with antimicrobial expertise. The intervention group (N = 141) received suggestions (written or verbally), whereas the control group did not (N = 111). Controlling for severity of illness between groups, the outcomes were similar with respect to clinical and microbiologic response to therapy, adverse events, inpatient mortality, or readmission rates. Interventions included change to oral therapy (31%), regimen or dosing changes (42%), stopping therapy (10%), or ordering additional laboratory tests (18%); 85% of the suggestions were instituted. Multiple logistic regression models identified randomization to the intervention group as the sole predictor of lower antimicrobial expenditures. A conservative annualized reduction in antimicrobial expenditures of $97,500 was realized. The intervention group also showed a trend toward reduced mean length of stay compared to the controls (20 vs. 24 days, respectively). Fifty percent of patients receiving targeted regimens had their treatment refined on the third day of therapy, resulting in narrower spectrum therapy and lower antimicrobial costs; most important, reducing antimicrobial use did not adversely impact patient outcomes. This study was later used as a platform to implement an ASP that is more robust in types of activities and numbers of patients served by the program. The team currently includes a part-time ID physician (2 hours per day, 5 days per week) and a full-time ID PharmD. A close collaboration exists with the Department of Epidemiology and Infection Prevention, the ID division, the pharmacy, administration, the patient safety officer, and the pharmacy and therapeutics committee.
Srinivasan et al. studied the impact of an antimicrobial management program on antimicrobial expenditures at Johns Hopkins Hospital. Before the introduction of a comprehensive ASP, the hospital used a closed formulary system and employed prior approval requirements for several antimicrobials. The ASP consisted of a hospital-funded ID physician, ID PharmD, and data analyst. The team concurrently reviewed antimicrobial therapy in all areas of the hospital except pediatrics and oncology. Their interventions included a survey and the use of institution-specific guidelines, concurrent antimicrobial review, and educational sessions. A “knowledge, attitude, and beliefs” survey was used to determine the awareness of antimicrobial use and resistance and sense deficiencies in knowledge that could lead to targeted education among house staff (41). Interestingly, only 18% viewed the program as an obstacle to patient care and 70% wanted additional feedback on antimicrobial choices. Hospital guidelines were published and updated annually. Antimicrobial therapy interventions occurred before
culture, and susceptibility results were available only when actively solicited or when called for prior authorization of an antimicrobial agent. For all others, interventions were suggested at the time the microbiologic data became available. Compliance with suggested recommendations by the ASP was 79%. The costs for antimicrobial agents for the covered areas decreased by 6.4% the first year and 2.2% the second year. Assuming a steady inflation rate of 4.5%, savings translated to $224,753 and $413,998 for fiscal years 2002 and 2003, respectively.
culture, and susceptibility results were available only when actively solicited or when called for prior authorization of an antimicrobial agent. For all others, interventions were suggested at the time the microbiologic data became available. Compliance with suggested recommendations by the ASP was 79%. The costs for antimicrobial agents for the covered areas decreased by 6.4% the first year and 2.2% the second year. Assuming a steady inflation rate of 4.5%, savings translated to $224,753 and $413,998 for fiscal years 2002 and 2003, respectively.
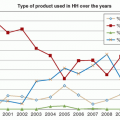
Bantar et al. demonstrated the impact of their ASP’s interventional component on antimicrobial use, cost savings, and antimicrobial resistance (42). The ASP consisted of an ID physician, two pharmacists, a microbiologist and laboratory technologist, an internal medicine physician, and a computer systems analyst. In 6-month periods, four consecutive intervention strategies were unveiled. During the first 6 months, an optional antimicrobial order form (ID diagnosis, pertinent epidemiologic data) was introduced and baseline data were collected (i.e., bacterial resistance, antimicrobial use, prescribing practice, HAI, and crude mortality rates). In the second period, an “initial intervention” period consisted of transforming the optional order form to a compulsory form and providing feedback to clinicians on the basis of a review of the data collected in the first period. In the third period, called the “education” period, clinicians were verbally engaged with each new antimicrobial order by members of the multidisciplinary team. The fourth or “active control” period was similar to the third period, but the ASP team member modified prescriptions if necessary. During the four periods, no antimicrobial agent was restricted. To estimate the rates of use of a particular drug in relation to other drugs, an index was calculated (e.g., rate of cefepime use to that for third-generation cephalosporins—ceftriaxone and ceftazidime—equaled cefepime/consumption of ceftriaxone and ceftazidime × 100). Consumption data were measured in defined daily doses (DDD). The program periods were associated with declining cost savings as time advanced (periods 2, 3, and 4 were associated with a reduction of $261,955, $57,245, and $12,881, respectively). Comparing antimicrobial order forms from period 1 (voluntary form and preintervention, N = 450) with period 4 (mandatory form with active intervention, N = 349), the ASP identified an increase in microbiologically based treatment intent (27% vs. 62.8%, respectively, p < 0.0001). The team intervened on 27% of the period 4 antimicrobial order forms. Of the interventions, either the dose or duration (not specified) was reduced in 11.5%, 47% involved streamlining therapy to a narrower choice, and 86.1% was associated with cost reduction. HAI impact (e.g., length of hospitalization and mortality; only length of stay was impacted significantly [p = 0.04]). The increased rate of cefepime use relative to third-generation cephalosporins was associated with declining third-generation cephalosporin resistance rates among Proteus mirabilis or Enterobacter cloacae but not to Escherichia coli or Klebsiella pneumoniae. The increased rate of aminopenicillin/sulbactam use relative to the third-generation cephalosporins in conjunction with a sustained reduction in vancomycin use was associated with a reduction in methicillin-resistant S. aureus (MRSA) rates. In addition, Pseudomonas aeruginosa resistance rates to carbapenems declined to 0% and were strongly associated with the reduction in carbapenem consumption.
The particular study by Bantar et al. is different than others in that it used a staggered approach to implementation. Although the cost reduction appeared to dwindle significantly in each newly introduced period, one cannot ignore the cumulative impact of the overall impact on cost. In addition, the final period offers a comprehensive mechanism for long-standing success and serves as a template to introduce other initiatives as deemed necessary. Part of the success related to reduction in antimicrobial resistance rates noted by this program is related to the high rate of carbapenem or ceftriaxone use and the “seldom”-ordered cefepime or aminopenicillin/sulbactam in conjunction with the types of problem pathogens noted at their hospital (e.g., AmpC phenotypes and carbapenem-resistant P. aeruginosa).




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree